Nursing Paper Example on Granulomatosis with Polyangiitis
/in Assignment Help, Homework Help, Nursing Paper Help /by Aimee GraceNursing Paper Example on Granulomatosis with Polyangiitis
Granulomatosis with polyangiitis (GPA), formerly known as Wegener’s granulomatosis, is a rare, systemic vasculitis affecting small to medium-sized blood vessels. It is characterized by necrotizing granulomas primarily in the respiratory tract and kidneys. GPA often presents with a wide range of symptoms, making diagnosis challenging. Early detection and treatment are crucial to preventing severe organ damage and improving prognosis. This autoimmune disease typically occurs in adults, with a slight predominance in males, and has no clear genetic or environmental cause.
Causes
The exact cause of GPA remains unknown. However, it is believed to result from an abnormal immune response triggered by environmental or infectious agents. Research suggests that bacterial or viral infections may initiate the autoimmune response.
Genetic predisposition may also play a role, particularly variants in human leukocyte antigen (HLA) genes that regulate immune function. Environmental factors such as exposure to silica and other occupational hazards have been loosely associated with GPA but require further study.
Signs and Symptoms
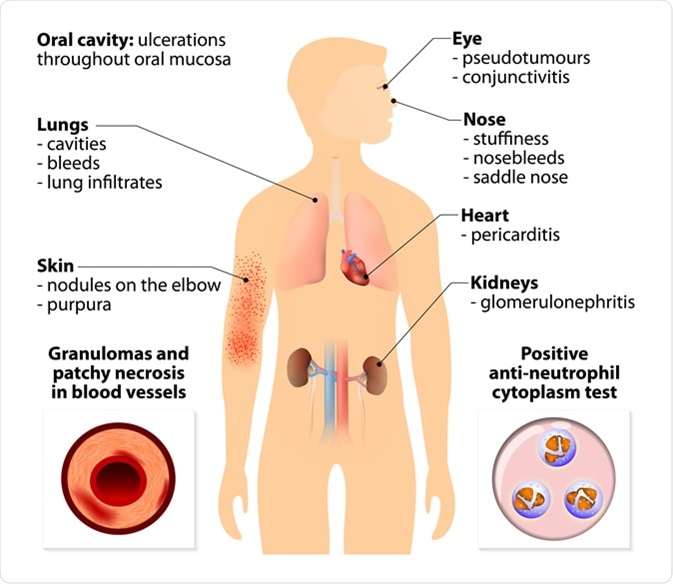
The clinical presentation of GPA is variable, but it typically involves the respiratory tract, kidneys, and other organ systems. Common symptoms include persistent nasal congestion, nosebleeds, and sinus infections due to inflammation in the upper respiratory tract. Lung involvement may lead to coughing, shortness of breath, and hemoptysis. Kidney involvement often manifests as rapidly progressive glomerulonephritis, which can cause hematuria and proteinuria.
Generalized symptoms such as fever, weight loss, and fatigue are also common. Skin rashes, joint pain, and eye inflammation may occur in some patients, reflecting systemic vasculitis.
Etiology
GPA is an autoimmune disease primarily driven by the production of antineutrophil cytoplasmic antibodies (ANCAs). These autoantibodies target proteins in neutrophils, particularly proteinase-3, leading to neutrophil activation and subsequent vascular inflammation.
The underlying etiology involves complex interactions between genetic susceptibility, environmental triggers, and immune system dysregulation. Although the precise mechanism remains unclear, studies suggest that activated neutrophils release inflammatory mediators, causing endothelial injury and granuloma formation.
Pathophysiology
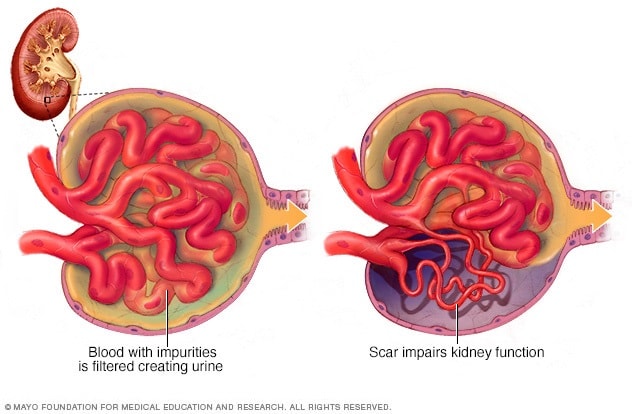
The pathophysiology of GPA involves immune-mediated inflammation of blood vessels and surrounding tissues. ANCAs play a central role by activating neutrophils, which adhere to vascular endothelium and release reactive oxygen species and proteolytic enzymes. This process damages blood vessel walls, leading to necrosis and granuloma formation.
Granulomas, a hallmark of GPA, consist of macrophages, multinucleated giant cells, and lymphocytes and are particularly prominent in the respiratory tract. Kidney involvement occurs when immune complexes deposit in glomeruli, causing glomerulonephritis. The systemic nature of GPA reflects widespread vascular inflammation.
(Nursing Paper Example on Granulomatosis with Polyangiitis)
Diagnosis
The diagnosis of GPA relies on clinical evaluation, laboratory tests, and imaging studies. Blood tests often reveal elevated inflammatory markers such as erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP). The presence of ANCAs, specifically proteinase-3 ANCA, is highly suggestive of GPA but not definitive.
Imaging studies, including chest X-rays and computed tomography (CT), can identify granulomas and other abnormalities in the lungs and sinuses. Tissue biopsy remains the gold standard for diagnosis, with findings of necrotizing granulomas and vasculitis confirming the disease.
Treatment Regimens
Treatment for GPA aims to suppress inflammation, prevent disease progression, and manage organ damage. Initial therapy typically involves high-dose corticosteroids combined with immunosuppressive agents such as cyclophosphamide or rituximab. Corticosteroids rapidly reduce inflammation, while immunosuppressive drugs target the underlying autoimmune process.
For maintenance therapy, methotrexate or azathioprine is often used to reduce the risk of relapse. In severe cases, plasma exchange may be employed to remove ANCAs from the bloodstream. Patients with kidney involvement may require dialysis or, in rare cases, kidney transplantation.
Patient Education
Education is a critical component of GPA management. Patients should understand the chronic nature of the disease and the importance of adherence to treatment regimens to prevent relapses. Awareness of potential medication side effects, including infections and bone loss due to long-term corticosteroid use, is essential.
Regular follow-ups with healthcare providers are necessary to monitor disease activity and organ function. Patients should also be encouraged to maintain a healthy lifestyle, including smoking cessation, to reduce additional cardiovascular risks.
Research and Future Directions
Advances in understanding GPA are leading to new therapeutic approaches. Ongoing research focuses on identifying specific genetic markers and immune pathways involved in the disease. Monoclonal antibodies targeting inflammatory cytokines and immune cells, such as rituximab, are being studied for their efficacy and safety in long-term disease control.
Additionally, biomarkers for early detection and monitoring disease activity are under investigation. These developments hold promise for improving outcomes and reducing the burden of GPA.
Conclusion
Granulomatosis with polyangiitis is a complex autoimmune disease characterized by systemic vasculitis and granuloma formation. Although its exact cause is unknown, it is closely associated with ANCAs and immune dysregulation. Early diagnosis and aggressive treatment are vital to preventing irreversible organ damage and improving quality of life. Advances in immunotherapy and ongoing research provide hope for better management and outcomes for patients with this challenging condition.
References
Jennette, J. C., & Falk, R. J. (2020). Pathogenesis of ANCA-associated vasculitis: The role of autoantibodies and neutrophils. Annual Review of Pathology: Mechanisms of Disease. https://www.annualreviews.org
Falk, R. J., & Jennette, J. C. (2023). Clinical features and diagnosis of granulomatosis with polyangiitis. New England Journal of Medicine. https://www.nejm.org
Yates, M., Watts, R. A., & Scott, D. G. (2021). Advances in the treatment of ANCA-associated vasculitis. Lancet Rheumatology. https://www.thelancet.com
Niles, J. L., & Mejia-Vilet, J. M. (2023). Immunosuppressive therapy in granulomatosis with polyangiitis: Current strategies. Kidney International Reports. https://www.kidney-international.org
Luqmani, R. A., & Suppiah, R. (2020). Long-term management and prognosis of granulomatosis with polyangiitis. Rheumatology (Oxford). https://academic.oup.com/rheumatology