Parkinson’s Disease Diagnosis
Parkinson’s Disease Diagnosis
A 67-year-old man presents to the health care provider with chief complaint of tremors in his arms. He also has noticed some tremors in his leg as well. The patient is accompanied by his son, who says that his father has become “stiff” and it takes him much longer to perform simple tasks. The son also relates that his father needs help rising from his chair.
Physical exam demonstrates tremors in the hands at rest and fingers exhibit “pill rolling” movement. The patient’s face is not mobile and exhibits a mask-like appearance. His gait is uneven, and he shuffles when he walks, and his head/neck, hips, and knees are flexed forward. He exhibits jerky or cogwheeling movement.
The patient states that he has episodes of extreme sweating and flushing not associated with activity. Laboratory data is unremarkable and the health care provider has diagnosed the patient with Parkinson’s Disease.
Case Study Analysis: Parkinson’s Disease Diagnosis
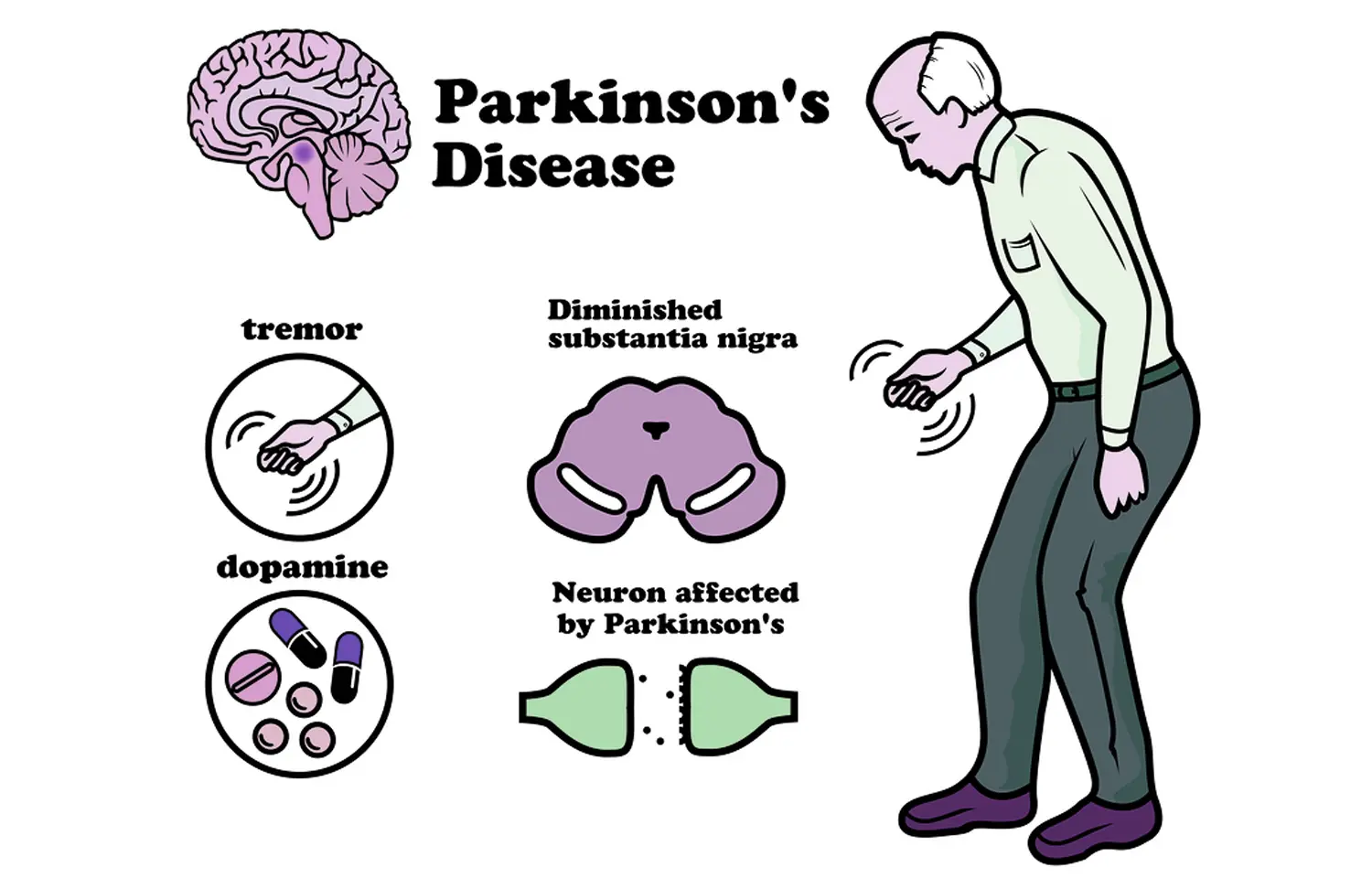
The case of a 67-year-old man presenting with tremors, stiffness, and other characteristic symptoms is indicative of Parkinson’s Disease. Parkinson’s Disease is a progressive neurodegenerative disorder primarily affecting motor function due to the loss of dopaminergic neurons in the substantia nigra region of the brain.
Key Symptoms and Clinical Presentation
The patient exhibits several hallmark signs of Parkinson’s Disease:
- Tremors: The presence of resting tremors in the arms and “pill-rolling” movements of the fingers are classic symptoms. These tremors typically occur when the muscles are relaxed.
- Bradykinesia: The patient’s son reports that he has become “stiff” and takes longer to perform simple tasks. Bradykinesia, or slowness of movement, is a core feature of the disease.
- Rigidity: The patient appears stiff and requires assistance rising from his chair. Rigidity is often observed in the limbs and neck.
- Postural Instability: The shuffling gait, along with the flexed posture of the head, neck, hips, and knees, suggests postural instability, common in advanced stages of Parkinson’s Disease.
- Non-Motor Symptoms: The episodes of extreme sweating and flushing, which are not associated with activity, may indicate autonomic dysfunction, a common non-motor symptom in Parkinson’s patients.
Diagnosis
The diagnosis of Parkinson’s Disease is primarily clinical and relies on the presence of at least two of the following motor symptoms: tremor, rigidity, bradykinesia, and postural instability (MDS Task Force, 2015). In this case, the patient presents with multiple features that align with these diagnostic criteria. The lack of significant findings in laboratory data further supports the diagnosis as there are no alternative conditions indicated.
Differential Diagnosis
While the clinical presentation strongly suggests Parkinson’s Disease, several other conditions could mimic its symptoms, necessitating careful differential diagnosis:
- Essential Tremor: This is characterized by action tremors rather than resting tremors and is less likely given the rigidity and bradykinesia present in this patient.
- Multiple System Atrophy: This condition can present similarly but typically includes more pronounced autonomic dysfunction and a different course of progression.
- Progressive Supranuclear Palsy: This condition can present with parkinsonian features; however, it typically involves prominent postural instability and ocular signs, which are not noted in this case.
Treatment Options
The management of Parkinson’s Disease focuses on alleviating symptoms and improving quality of life. Common treatment options include:
- Levodopa/Carbidopa: This is the most effective treatment for motor symptoms. Levodopa is converted to dopamine in the brain, alleviating symptoms of bradykinesia and rigidity (Mamikonyan et al., 2019).
- Dopamine Agonists: Medications such as pramipexole and ropinirole can be used as initial therapy or adjunct to levodopa to help manage symptoms.
- MAO-B Inhibitors: These medications, such as selegiline, can help prolong the effects of levodopa and provide additional symptomatic relief.
Conclusion
This case study illustrates the clinical features of Parkinson’s Disease, highlighting the importance of accurate diagnosis based on observable symptoms. The treatment plan should be tailored to the individual, focusing on improving the patient’s functional capabilities and quality of life. Ongoing monitoring and adjustments to therapy are essential as the disease progresses.
References
Mamikonyan, E., LaPorte, D., & Dorsey, E. R. (2019). Clinical management of Parkinson’s disease: A review. American Journal of Health-System Pharmacy, 76(14), 1039-1048. https://doi.org/10.1093/ajhp/zxz095
MDS Task Force on Rating Scales. (2015). The Movement Disorder Society’s task force on rating scales for Parkinson’s disease: Recommendations for a comprehensive version of the Unified Parkinson’s Disease Rating Scale. Movement Disorders, 30(7), 1006-1022. https://movementdisorders.onlinelibrary.wiley.com/doi/full/10.1002/mds.25412
Schapira, A. H. V., & Mann, D. M. A. (2019). Neurodegenerative diseases. In G. K. C. S. Hu & A. H. V. Schapira (Eds.), Textbook of Clinical Neurology (pp. 505-517). Elsevier. https://www.elsevier.com/books/textbook-of-clinical-neurology/hu/978-0-323-50713-7
Gao, A. F., & Lang, A. E. (2016). Parkinson’s disease: diagnosis and management. BMJ, 355, i6282. https://www.bmj.com/content/355/bmj.i6282
Simmons, Z., & Decker, P. (2018). Parkinson’s Disease: Diagnosis and Treatment. Primary Care: Clinics in Office Practice, 45(3), 465-486. https://doi.org/10.1016/j.pop.2018.04.002



