Nursing Paper Example on Typhus
Nursing Paper Example on Typhus
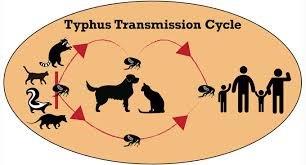
Typhus is a group of infectious diseases caused by the Rickettsia bacteria, which is transmitted to humans through arthropod vectors like lice, fleas, and mites. There are three main types of typhus: epidemic typhus, endemic (or murine) typhus, and scrub typhus. Each of these diseases has distinct causative agents, vectors, and geographic prevalence, though they share similarities in symptom presentation and treatment protocols.
Types of Typhus and Their Causes
- Epidemic Typhus:
- Causative Agent: Rickettsia prowazekii
- Vector: Body lice (Pediculus humanus corporis)
- Transmission: Epidemic typhus occurs when lice carrying R. prowazekii bite a person, and bacteria enter through the bite wound or skin abrasions. Outbreaks are often associated with crowded, unsanitary living conditions and colder climates (Raoult & Roux, 1999).
- Endemic (Murine) Typhus:
- Causative Agent: Rickettsia typhi
- Vector: Fleas, especially the rat flea (Xenopsylla cheopis)
- Transmission: Murine typhus is transmitted to humans through flea bites. It is endemic in regions with high rat populations, particularly in urban settings with warm climates (Azad, 1990).
- Scrub Typhus:
- Causative Agent: Orientia tsutsugamushi
- Vector: Chiggers (larval mites of the family Trombiculidae)
- Transmission: Scrub typhus occurs when chiggers carrying O. tsutsugamushi bite humans. It is prevalent in rural areas across Asia-Pacific and is especially common in scrubland environments (Kelly et al., 2009).
(Nursing Paper Example on Typhus)
Signs and Symptoms of Typhus
The symptoms of typhus generally emerge within 5–14 days following exposure. Although all forms of typhus share common symptoms, they vary in severity.
- Common Symptoms Across Typhus Types:
- Fever and Chills: High fever is a primary symptom across all typhus types.
- Headache and Myalgia: Severe headache, joint pain, and muscle aches accompany the fever.
- Rash: A maculopapular rash usually appears a few days after the onset of fever. This rash often spreads from the trunk to the extremities (Prakash & Desai, 2016).
- Symptoms Specific to Epidemic Typhus:
- Mental Confusion and Delirium: In severe cases, patients may exhibit delirium or confusion.
- Gangrene: Due to poor blood circulation, epidemic typhus can lead to gangrene of the extremities, particularly in untreated cases (Raoult & Roux, 1999).
- Symptoms of Scrub Typhus:
- Eschar at Bite Site: A distinctive black, crusted lesion called an eschar may form at the chigger bite site, serving as a pathognomonic sign.
- Lymphadenopathy: Swelling of lymph nodes is common and can be severe (Kelly et al., 2009).
Pathophysiology of Typhus Infections
Typhus infections result from the invasion of endothelial cells, which line the blood vessels. After entering the bloodstream, Rickettsia and Orientia bacteria attack these cells, leading to widespread vascular inflammation.
- Endothelial Damage and Vasculitis:
- Rickettsia and Orientia bacteria replicate within endothelial cells, causing cell lysis and the release of bacteria into surrounding tissues. The resulting inflammation, known as vasculitis, disrupts blood flow and leads to tissue damage.
- In cases of severe typhus, vasculitis can result in multi-organ damage, as blood flow to organs such as the kidneys, liver, and brain becomes compromised (Weiss et al., 2016).
- Immune Response:
- The immune system’s response to typhus infection involves macrophages, neutrophils, and inflammatory cytokines. The cytokine release causes systemic inflammation, leading to symptoms such as fever, rash, and pain.
- In the case of scrub typhus, the immune response to O. tsutsugamushi can sometimes lead to an exaggerated inflammatory response, causing complications like respiratory distress and shock (Kelly et al., 2009).
Diagnosis of Typhus
Early diagnosis of typhus is challenging due to its nonspecific symptoms. However, laboratory tests and clinical history, particularly recent exposure to vectors, help confirm typhus.
- Clinical Evaluation:
- Symptom Assessment: Physicians examine symptoms like high fever, rash, and eschar formation in scrub typhus to differentiate typhus from other febrile illnesses.
- Exposure History: Recent travel or exposure to areas with high vector populations, such as rural or impoverished areas, is an important diagnostic factor (Prakash & Desai, 2016).
- Laboratory Testing:
- Serological Tests: Serological assays like the Weil-Felix test and indirect immunofluorescence are commonly used to detect antibodies specific to Rickettsia or Orientia bacteria.
- Polymerase Chain Reaction (PCR): PCR tests identify bacterial DNA, offering high sensitivity for early detection, particularly in epidemic typhus cases (Raoult & Roux, 1999).
Treatment and Management of Typhus
Prompt antibiotic therapy is critical in managing typhus, especially in severe cases where complications are likely.
- Antibiotic Therapy:
- Doxycycline: Doxycycline is the first-line treatment for all types of typhus. It is effective in reducing symptoms and mortality rates when administered early.
- Alternative Antibiotics: Chloramphenicol is used as an alternative, particularly in regions with limited access to doxycycline, though its use is restricted due to potential side effects (Weiss et al., 2016).
- Supportive Care:
- Hydration and Fever Management: Supportive care, including hydration and antipyretics, helps manage fever and dehydration.
- Monitoring for Complications: In severe cases, particularly epidemic typhus, patients may require intensive monitoring for complications such as renal failure or respiratory distress.
(Nursing Paper Example on Typhus)
Prevention and Control of Typhus
Preventing typhus infections relies on controlling vector populations and taking personal protective measures in endemic areas.
- Vector Control:
- Insecticides and Hygiene: Effective use of insecticides, rodent control, and improved sanitation can significantly reduce louse and flea populations, limiting the spread of typhus.
- Vaccination Research: While there is no vaccine for typhus, research continues in this area to address epidemic outbreaks in at-risk populations (Weiss et al., 2016).
- Personal Protective Measures:
- Use of Repellents: Applying insect repellents, especially in areas prone to scrub typhus, provides protection against chigger bites.
- Protective Clothing: Wearing long sleeves and pants in endemic regions reduces exposure to vectors.
- Public Health Education:
- Educating communities on vector prevention and symptoms of typhus helps in early detection and timely treatment, lowering morbidity and mortality rates associated with the disease (Kelly et al., 2009).
Complications of Typhus
Typhus infections, especially epidemic and scrub typhus, can lead to life-threatening complications if left untreated.
- Multi-Organ Failure:
- Vasculitis resulting from typhus can lead to organ damage and failure, especially in the kidneys, liver, and lungs. Scrub typhus is particularly associated with respiratory distress syndrome.
- In cases of epidemic typhus, sepsis may result from bacterial invasion of the bloodstream, causing shock and potentially fatal outcomes (Weiss et al., 2016).
- Neurological Complications:
- Typhus infections can lead to neurological symptoms like confusion, delirium, and even coma in severe cases.
- Encephalitis, a serious inflammation of the brain, can occur, particularly with epidemic typhus (Prakash & Desai, 2016).
Conclusion
Typhus remains a public health concern, particularly in regions with poor sanitation and limited healthcare access. Each type of typhus—epidemic, murine, and scrub—poses specific risks and requires targeted prevention and treatment strategies. Early diagnosis, effective antibiotic therapy, and vector control measures are vital in reducing typhus-related morbidity and mortality, particularly in areas prone to outbreaks. Addressing these factors is crucial to controlling typhus and protecting vulnerable populations from this potentially deadly disease.
References
Azad, A. F. (1990). Epidemiology of Murine Typhus. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2466734/
Kelly, D. J., Richards, A. L., Temenak, J., Strickman, D., & Dasch, G. A. (2009). The Past and Present Threat of Rickettsial Diseases to Military Medicine and International Public Health. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2680247/
Prakash, S. & Desai, D. (2016). A comprehensive review on typhus fever. https://pubmed.ncbi.nlm.nih.gov/27215832/
Raoult, D., & Roux, V. (1999). Rickettsioses as paradigms of new or emerging infectious diseases. https://academic.oup.com/cid/article/29/5/963/286447



