Nursing Paper Example on Ankylosing Spondylitis
Nursing Paper Example on Ankylosing Spondylitis
Ankylosing spondylitis is a chronic inflammatory disease primarily affecting the spine and sacroiliac joints, causing pain, stiffness, and progressive loss of spinal mobility. It is classified as a type of axial spondyloarthritis and has systemic effects that can involve other joints and organs, such as the eyes, heart, and lungs. The condition is often associated with a genetic marker called HLA-B27, although its precise etiology remains unclear. Early recognition and management are critical to preventing irreversible spinal damage and maintaining quality of life.
Causes of Ankylosing Spondylitis
The exact cause of ankylosing spondylitis remains unknown, but it is believed to involve a combination of genetic, environmental, and immunological factors.
Genetic predisposition: The HLA-B27 gene is present in approximately 85-90% of individuals with ankylosing spondylitis. While not everyone with this gene develops the disease, its presence significantly increases risk.
Immune dysregulation: Dysregulated immune responses, including the activation of T cells and cytokines like tumor necrosis factor-alpha (TNF-α) and interleukin-17 (IL-17), play a crucial role in disease progression.
Environmental factors: Infections, particularly of the gastrointestinal or genitourinary tracts, may trigger the onset in genetically predisposed individuals.
Signs and Symptoms
The symptoms of ankylosing spondylitis can vary widely in severity but typically include the following:
Back pain and stiffness: Chronic back pain, particularly in the lower spine, is a hallmark symptom. Stiffness is often worse in the morning and improves with activity.
Peripheral arthritis: Pain and swelling may affect joints such as the hips, shoulders, knees, or ankles.
Enthesitis: Inflammation of entheses, the sites where tendons or ligaments attach to bone, is common. Common areas include the Achilles tendon and plantar fascia.
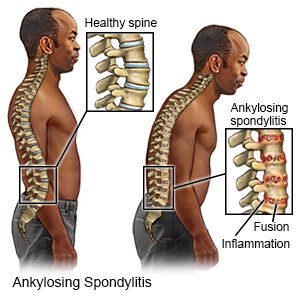
Reduced spinal mobility: Progressive fusion of the vertebrae leads to limited spinal flexibility and a characteristic “question mark” posture.
Extra-articular manifestations: These include:
Eye involvement: Acute anterior uveitis, characterized by eye pain, redness, and blurred vision.
Cardiovascular complications: Aortitis and conduction abnormalities.
Pulmonary fibrosis: Rarely, fibrosis of the upper lobes of the lungs may occur.
Etiology
The pathogenesis of ankylosing spondylitis is complex, involving genetic predisposition, immune system activation, and environmental triggers.
Genetics: HLA-B27 is the strongest known genetic factor. However, additional genetic loci such as ERAP1 (endoplasmic reticulum aminopeptidase 1) have been implicated.
Immunological factors: The disease involves excessive activation of pro-inflammatory cytokines, particularly TNF-α and IL-17, which drive inflammation and bone remodeling.
Environmental influences: The role of infections as triggers, particularly by certain gut bacteria, is supported by increased gut permeability and dysbiosis in some patients.
Pathophysiology
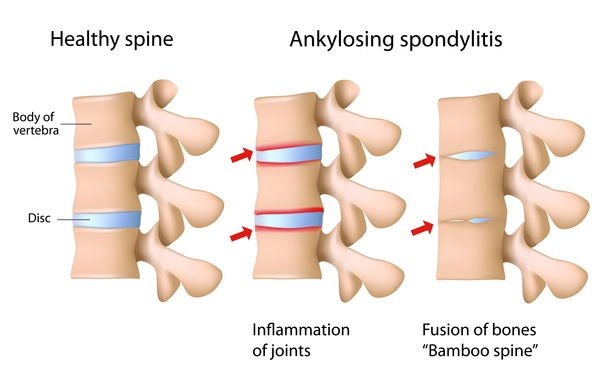
The hallmark of ankylosing spondylitis is chronic inflammation of the sacroiliac joints and spine, leading to new bone formation and eventual fusion of the vertebrae.
Initial inflammation: Inflammatory cells infiltrate the entheses and surrounding tissues, releasing cytokines like TNF-α and IL-17. This leads to enthesitis, pain, and swelling.
Chronic inflammation: Persistent inflammation causes tissue damage and the release of growth factors, such as bone morphogenetic proteins (BMPs), which promote new bone formation.
New bone formation: Pathological bone formation bridges vertebrae, resulting in the fusion of the spine (ankylosis).
Systemic effects: Chronic inflammation may extend to other tissues, explaining the extra-articular manifestations such as uveitis and cardiovascular involvement.
DSM-5 Diagnosis
Ankylosing spondylitis is not a psychiatric disorder and is not categorized in the DSM-5. However, chronic pain and reduced mobility associated with the disease can lead to psychological issues, such as depression or anxiety. These secondary mental health conditions should be assessed and managed as part of a holistic treatment plan.
Diagnosis
The diagnosis of ankylosing spondylitis involves clinical evaluation, imaging, and laboratory tests.
- Clinical criteria:
Chronic back pain lasting more than three months.
Morning stiffness improving with activity.
Reduced range of motion in the spine.
- Imaging studies:
X-rays: Early changes include sacroiliitis, while later stages show spinal fusion.
MRI: Detects early inflammatory changes, including bone marrow edema.
- Laboratory tests:
HLA-B27 testing: Positive in most patients but not diagnostic alone.
Elevated inflammatory markers: Increased C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR).
Treatment Regimens
The management of ankylosing spondylitis aims to reduce inflammation, alleviate symptoms, and prevent complications.
- Pharmacological treatment:
Nonsteroidal anti-inflammatory drugs (NSAIDs): First-line treatment for pain and inflammation.
Biologics: Tumor necrosis factor-alpha inhibitors (e.g., adalimumab, etanercept) or interleukin-17 inhibitors (e.g., secukinumab) are effective in severe cases.
Disease-modifying antirheumatic drugs (DMARDs): Limited to peripheral arthritis as they are less effective for axial symptoms.
- Physical therapy: Exercises to improve spinal mobility, posture, and overall fitness are crucial in long-term management.
- Surgical intervention: Joint replacement surgery may be required for severe hip involvement.
- Lifestyle modifications: Smoking cessation and regular exercise can help maintain lung capacity and spinal health.
Patient Education
Educating patients with ankylosing spondylitis is essential for effective disease management.
Understanding the disease: Patients should learn about the chronic nature of the disease and the importance of early intervention.
Importance of adherence: Regular use of prescribed medications and participation in physical therapy is vital for symptom control.
Self-management strategies: Encouraging patients to maintain an active lifestyle, practice good posture, and use ergonomic aids.
Monitoring for complications: Educating patients to recognize symptoms of uveitis, cardiac issues, or severe pain requiring medical attention.
Conclusion
Ankylosing spondylitis is a chronic inflammatory condition that significantly impacts patients’ quality of life if left untreated. Advances in understanding its pathophysiology have led to the development of effective treatments, particularly biologic therapies targeting specific cytokines. Early diagnosis, combined with a multidisciplinary approach involving medications, physical therapy, and patient education, is crucial for managing symptoms and preventing long-term complications.
References
Brown, M. A., & Kenna, T. J. (2020). The genetics of ankylosing spondylitis. Rheumatology, 59(Supplement_4), iv19-iv27. https://doi.org/10.1093/rheumatology/keaa343
Sieper, J., Poddubnyy, D., & Miossec, P. (2022). Axial spondyloarthritis: Advances in pathogenesis and treatment. The Lancet, 400(10360), 1081-1093. https://doi.org/10.1016/S0140-6736(22)01548-7
Ward, M. M., Deodhar, A., & Akl, E. A. (2019). Update of the American College of Rheumatology/Spondylitis Association of America/Spondyloarthritis Research and Treatment Network guidelines for the treatment of ankylosing spondylitis and nonradiographic axial spondyloarthritis. Arthritis Care & Research, 71(10), 1285-1299. https://doi.org/10.1002/acr.24025



