Nursing Paper Example on Avascular Necrosis
Nursing Paper Example on Avascular Necrosis
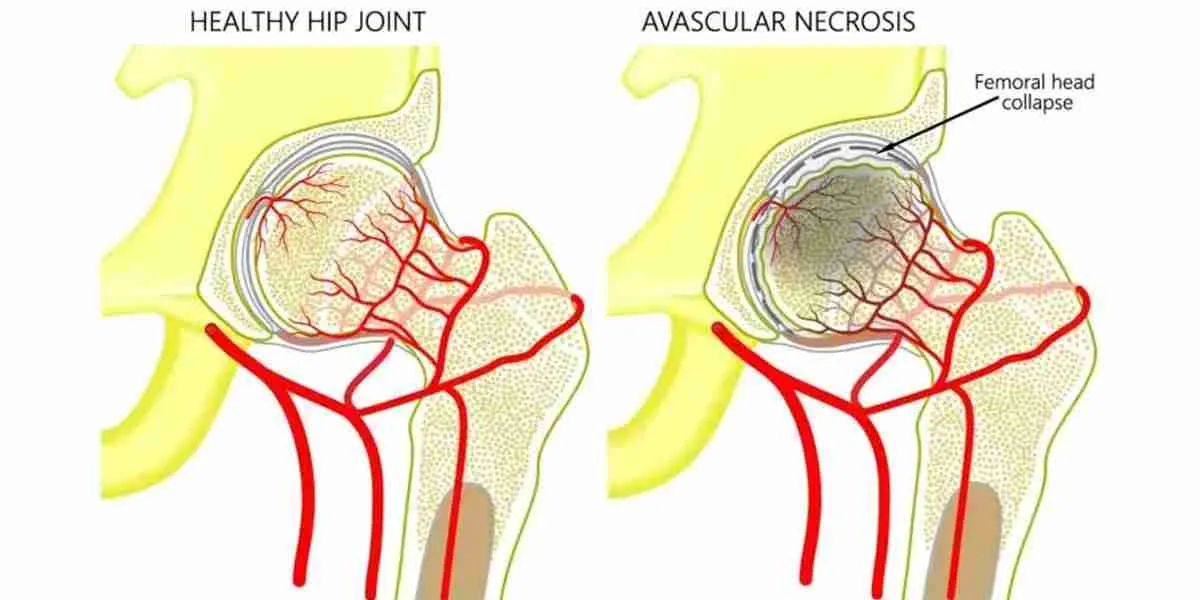
Avascular necrosis, also known as osteonecrosis, is a pathological condition characterized by the death of bone tissue due to disrupted blood supply. This leads to the gradual collapse of the bone and joint destruction if left untreated. It commonly affects weight-bearing bones such as the femoral head but can occur in any bone. The condition has multifactorial causes, with risk factors including trauma, corticosteroid use, and excessive alcohol consumption. Timely diagnosis and appropriate intervention are essential to prevent irreversible damage and disability.
Causes of Avascular Necrosis
The causes of avascular necrosis can be divided into traumatic and non-traumatic categories:
- Traumatic causes: Bone fractures and joint dislocations can disrupt the blood supply, leading to avascular necrosis.
- Non-traumatic causes:
Corticosteroid use: Prolonged or high-dose corticosteroid therapy can lead to fat embolism and vascular compromise.
Alcohol abuse: Chronic alcohol consumption disrupts fatty metabolism, leading to fat embolism and vascular blockage.
Blood disorders: Conditions like sickle cell anemia can cause blood vessel occlusion and tissue ischemia.
Autoimmune diseases: Lupus erythematosus and other autoimmune diseases can impair vascular integrity.
Idiopathic cases: In some individuals, the exact cause remains unknown.
Understanding the underlying cause aids in formulating a targeted treatment approach.
Signs and Symptoms
The clinical presentation of avascular necrosis varies based on the stage of the disease and the affected bone:
Early stages: Often asymptomatic or presenting with mild pain during activity.
Progressive stages: Persistent pain, both at rest and with movement. Restricted joint mobility due to pain and structural changes.
Advanced stages: Joint deformity and functional impairment due to bone collapse. Crepitus or grinding sensation during joint movement.
Patients often experience a delay in diagnosis due to the nonspecific nature of early symptoms.
Etiology
The etiology of avascular necrosis is closely linked to factors that impair bone vascularization:
Mechanical interruption: Traumatic events disrupt blood vessels directly.
Intravascular causes: Fat embolism and sickle-shaped red blood cells block small vessels supplying the bone.
Extravascular compression: Edema and increased intraosseous pressure compress blood vessels, leading to ischemia.
The complex interplay of these factors determines the progression and severity of the disease.
Pathophysiology
The pathophysiology of avascular necrosis involves ischemia, necrosis, and secondary bone remodeling:
Ischemia: Disruption of blood supply causes localized ischemia in the bone.
Bone cell death: Osteocytes and bone marrow cells die within hours to days of ischemia.
Structural weakening: Necrosis weakens the bone structure, leading to microfractures and collapse.
Reactive processes: Surrounding bone and cartilage attempt repair, but the weakened structure often leads to further damage.
This progressive cycle of damage and repair underscores the need for early intervention.
DSM-5 Diagnosis
Avascular necrosis is not classified under the DSM-5 as it is a physical condition rather than a psychiatric disorder. However, patients may experience mental health challenges such as depression or anxiety due to chronic pain or disability.
Diagnosis
The diagnosis of avascular necrosis involves clinical evaluation and imaging studies:
- Clinical features:
Pain, limited range of motion, and history of risk factors like corticosteroid use or trauma.
- Imaging studies:
X-rays: Detect late-stage bone collapse and joint deformity.
Magnetic resonance imaging (MRI): The most sensitive method for detecting early-stage avascular necrosis.
Bone scans: Identify areas of decreased bone activity.
Computed tomography (CT): Provides detailed views of bone integrity.
A combination of these tools ensures accurate diagnosis and staging.
Treatment Regimens
Treatment of avascular necrosis aims to preserve joint function and prevent disease progression.
- Non-surgical management:
Pharmacological therapy: Bisphosphonates, anticoagulants, and vasodilators may improve blood flow and slow progression.
Lifestyle modifications: Weight management and smoking cessation reduce stress on affected joints.
Physical therapy: Exercises to maintain joint function and strengthen surrounding muscles.
- Surgical interventions:
Core decompression: Relieves intraosseous pressure and promotes revascularization.
Bone grafting: Provides structural support and aids in regeneration.
Osteotomy: Redistributes weight-bearing stress to unaffected bone areas.
Joint replacement: Used in advanced stages with significant joint destruction.
The choice of treatment depends on the stage, location, and severity of the disease.
Patient Education
Educating patients about avascular necrosis is vital for successful management:
Understanding risk factors: Patients should be aware of modifiable risk factors, such as alcohol consumption and corticosteroid use.
Early symptom recognition: Teach patients to seek medical attention for unexplained joint pain.
Adherence to therapy: Emphasize the importance of following prescribed treatments and attending follow-up appointments.
Preventive strategies: Encourage joint protection through weight control and the use of assistive devices.
Empowering patients with knowledge improves treatment outcomes and quality of life.
Additional Considerations
Complications: Joint collapse, osteoarthritis, and chronic pain are significant complications of untreated avascular necrosis.
Prognosis: Early-stage disease has a better prognosis, while advanced stages often require surgical intervention.
Conclusion
Avascular necrosis is a debilitating condition requiring prompt recognition and comprehensive management. Advances in imaging and therapeutic techniques have improved early detection and treatment outcomes. By addressing risk factors, initiating timely treatment, and educating patients, the progression of this disease can be mitigated, preserving joint function and quality of life.
References
Mont, M. A., Cherian, J. J., Sierra, R. J., Jones, L. C., & Lieberman, J. R. (2015). Osteonecrosis of the femoral head: What the orthopedist needs to know. AAOS Now, 23(6), 38-47. https://aaos.org
Weinstein, R. S. (2012). Glucocorticoid-induced osteonecrosis. Endocrine, 41(2), 183-190. https://doi.org/10.1007/s12020-011-9569-8
Assouline-Dayan, Y., Chang, C., Greenspan, A., Shoenfeld, Y., & Gershwin, M. E. (2002). Pathogenesis and natural history of osteonecrosis. Seminars in Arthritis and Rheumatism, 32(2), 94-124. https://doi.org/10.1053/sarh.2002.33720
Jones, L. C., & Hungerford, D. S. (2004). Osteonecrosis: Etiology, diagnosis, and treatment. Current Opinion in Rheumatology, 16(4), 443-449. https://doi.org/10.1097/01.bor.0000133022.42985.d6



