Nursing Paper Example on Calciphylaxis
Nursing Paper Example on Calciphylaxis
Calciphylaxis, also known as calcific uremic arteriolopathy, is a rare but severe disorder characterized by systemic vascular calcification, ischemic skin lesions, and high mortality rates. It predominantly occurs in individuals with end-stage renal disease (ESRD) but may also affect those without kidney disease. The condition results from calcium-phosphate metabolism disturbances, vascular injury, and pro-inflammatory processes. Timely diagnosis and management are critical to improving patient outcomes.
Causes of Calciphylaxis
Calciphylaxis arises from multifactorial causes, including disturbances in mineral metabolism, vascular injury, and systemic inflammation.
Disturbed calcium-phosphate metabolism: Hyperphosphatemia and hypercalcemia in ESRD patients contribute to vascular calcification. Secondary hyperparathyroidism exacerbates imbalances in calcium and phosphate levels.
Medication-related factors: Calcium-based phosphate binders and vitamin D analogs increase calcium-phosphate product levels, promoting vascular calcification. Warfarin inhibits matrix Gla-protein, a natural inhibitor of vascular calcification.
Systemic inflammation and vascular injury: Chronic inflammation and oxidative stress damage vascular endothelium, facilitating calcification.
Risk factors: Female sex, obesity, diabetes mellitus, and hypoalbuminemia increase calciphylaxis risk.
Understanding these factors highlights the importance of managing metabolic abnormalities to prevent calciphylaxis.
Signs and Symptoms
Calciphylaxis manifests with a combination of cutaneous, systemic, and metabolic features.
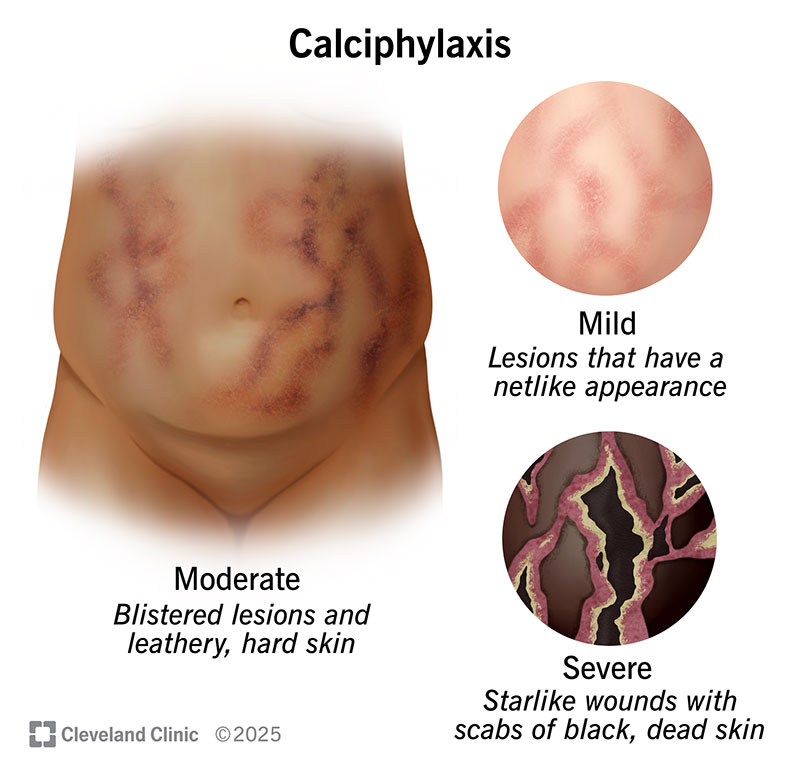
Cutaneous manifestations: Painful skin lesions that progress to necrotic ulcers. Lesions are commonly located on the thighs, abdomen, and buttocks. Surrounding skin may appear violaceous or mottled.
Systemic features: Fever and malaise. Secondary bacterial infections, which may lead to sepsis.
Metabolic abnormalities: Persistent hyperphosphatemia and hypercalcemia. Elevated parathyroid hormone levels due to secondary hyperparathyroidism.
These symptoms often overlap with other conditions, complicating diagnosis.
Etiology
Calciphylaxis primarily results from a complex interplay of vascular injury, pro-calcification factors, and inflammatory processes.
Vascular calcification: Calcium-phosphate deposition occurs in the medial layer of small arteries. Matrix Gla-protein inhibition contributes to unregulated calcification.
Inflammation and endothelial dysfunction: Chronic inflammation promotes endothelial injury, enhancing calcium deposition and thrombotic occlusion.
Pro-coagulant state: Thrombosis of microvasculature worsens ischemia, leading to necrotic skin lesions.
This pathophysiology underscores the systemic nature of calciphylaxis and its high morbidity and mortality.
Pathophysiology
The pathogenesis of calciphylaxis involves several interconnected mechanisms:
Calcium-phosphate imbalance: Hyperphosphatemia and hypercalcemia lead to vascular smooth muscle cell transdifferentiation into osteoblast-like cells, promoting calcification.
Vascular injury and thrombosis: Endothelial injury and hypercoagulability contribute to thrombosis and ischemia in small arterioles.
Inflammatory processes: Cytokine release exacerbates vascular damage and calcification.
Adipose tissue involvement: Calcification predominantly affects arterioles within subcutaneous adipose tissue, leading to skin necrosis.
These processes result in ischemic tissue damage, non-healing ulcers, and systemic complications.
DSM-5 Diagnosis
As calciphylaxis is not a psychiatric condition, it is not classified under the DSM-5.
Diagnosis
Diagnosis of calciphylaxis is primarily clinical but may require supportive investigations.
Clinical evaluation:
Assessment of painful skin lesions and systemic symptoms.
Risk factors such as ESRD, diabetes, and hyperparathyroidism should be evaluated.
Laboratory tests:
Elevated calcium-phosphate product.
High parathyroid hormone levels.
Inflammatory markers such as C-reactive protein.
Imaging:
Plain X-rays or CT scans may reveal vascular calcification.
Bone scintigraphy highlights areas of calcification and inflammation.
Skin biopsy:
Confirms diagnosis by showing calcification of small vessel walls and thrombotic occlusion.
Biopsy carries a risk of poor wound healing.
Prompt recognition and diagnosis are essential for initiating effective treatment.
Treatment Regimens
Calciphylaxis management involves a combination of medical, surgical, and supportive interventions.
Medical therapies:
Sodium thiosulfate:
Chelates calcium, reduces oxidative stress, and improves wound healing.
Vitamin K supplementation:
Restores matrix Gla-protein function, inhibiting vascular calcification.
Parathyroidectomy:
Indicated for refractory secondary hyperparathyroidism.
Dialysis modifications:
Use of low-calcium dialysate to reduce calcium-phosphate product levels.
Intensified dialysis to improve phosphate clearance.
Wound care:
Aggressive management of skin ulcers with debridement and infection control.
Analgesia:
Multimodal pain management, including opioids and non-opioid analgesics.
Timely and multidisciplinary care is crucial for improving survival and quality of life.
Patient Education
Educating patients about calciphylaxis is essential for promoting adherence to treatment and preventing complications.
Risk factor modification: Adherence to dietary phosphate restrictions and prescribed medications. Avoiding calcium-based phosphate binders.
Early recognition: Prompt reporting of new skin lesions or worsening pain to healthcare providers.
Lifestyle modifications: Maintaining a healthy weight and managing diabetes. Engaging in smoking cessation to improve vascular health.
Support groups and counseling services can help patients cope with the psychological burden of this chronic condition.
Additional Considerations
Complications: Non-healing ulcers and secondary infections. Sepsis is a leading cause of mortality in calciphylaxis.
Prognosis: High mortality rates, exceeding 50% in some cohorts. Early diagnosis and aggressive treatment improve outcomes.
Research and future directions: Investigating novel therapies targeting vascular calcification pathways. Evaluating the role of emerging biomarkers in early diagnosis.
Conclusion
Calciphylaxis is a complex and life-threatening condition requiring a multidisciplinary approach to diagnosis and treatment. The interplay of metabolic, inflammatory, and vascular factors underpins its pathogenesis, resulting in severe morbidity and high mortality rates. Comprehensive management strategies, including medical therapy, dialysis modifications, and patient education, can significantly improve outcomes. Continued research into innovative treatment modalities holds promise for reducing disease burden and improving patient survival.
References
Brandenburg, V. M., & Kramann, R. (2020). Calciphylaxis: A still unmet challenge. Clinical Kidney Journal, 13(2), 282-284. https://doi.org/10.1093/ckj/sfz178
Nigwekar, S. U., et al. (2018). Calciphylaxis: Risk factors, diagnosis, and treatment. American Journal of Kidney Diseases, 66(1), 133-146. https://doi.org/10.1053/j.ajkd.2015.12.030
Weenig, R. H. (2017). Calciphylaxis: Current concepts in pathogenesis, diagnosis, and treatment. Journal of the American Academy of Dermatology, 56(4), 569-579. https://doi.org/10.1016/j.jaad.2006.08.064
National Kidney Foundation. (2023). Understanding calciphylaxis. https://www.kidney.org/atoz/content/calciphylaxis
U.S. National Library of Medicine. (2023). Calciphylaxis: Overview and management. https://medlineplus.gov/calciphylaxis.html