Nursing Paper Example on Hidradenitis Suppurativa
Nursing Paper Example on Hidradenitis Suppurativa
Hidradenitis suppurativa (HS) is a chronic skin condition characterized by the formation of painful, inflamed lumps and abscesses in areas where skin rubs together, such as the armpits, groin, buttocks, and under the breasts. This condition primarily affects hair follicles and sweat glands, leading to the development of lesions that may drain pus or blood. Over time, repeated flare-ups can result in scar tissue and tunnels under the skin. HS is often misdiagnosed or dismissed as simple acne or boils, making timely treatment critical to reducing complications.
Causes
The exact cause of HS is not fully understood, but genetic and environmental factors are believed to play a role. A major contributing factor is inflammation within the hair follicles and sweat glands. The condition has a strong genetic component, as it is often seen in families, suggesting an inherited predisposition.
Environmental triggers such as obesity, smoking, hormonal changes, and friction from tight clothing can exacerbate symptoms. Lifestyle factors, particularly smoking, are significant risk factors for the disease, worsening the severity and frequency of flare-ups. Additionally, alterations in immune system functioning are thought to play a role in the abnormal inflammatory response associated with HS.
While it is not classified as an autoimmune disorder, the body’s immune system appears to mistakenly attack the skin’s hair follicles, causing the inflammation and abscesses that define the disease. However, not all cases of HS are genetically determined, and environmental triggers can also play a key role in the development and exacerbation of the condition.
Signs and Symptoms
The hallmark symptoms of hidradenitis suppurativa are painful, inflamed lumps or abscesses in the skin’s folds, often leading to abscess formation and pus drainage. These lumps may rupture over time, releasing foul-smelling fluid. These painful lumps can recur in the same areas, causing the formation of tunnel-like structures under the skin called sinus tracts. Over time, repeated flare-ups lead to the thickening of the skin and the formation of scar tissue. The affected areas typically include the armpits, groin, buttocks, and under the breasts, but any skin fold can be involved.
Early-stage symptoms may present as small, pimple-like lumps that progress into larger abscesses. As the disease progresses, these areas may become swollen, red, and tender. Individuals may also experience an increased frequency of flare-ups, leading to chronic discomfort and even disability in severe cases. In addition to visible skin changes, patients with hidradenitis suppurativa may experience systemic symptoms such as fever and fatigue during active flare-ups.
Etiology
The precise etiology of hidradenitis suppurativa remains unclear, though it is thought to involve a combination of genetic, environmental, and immunological factors. A family history of the condition is a strong indicator of a genetic predisposition, suggesting that certain genetic mutations may contribute to its onset. Mutations in the NF-kB pathway, which regulates immune responses and inflammation, have been linked to HS. This pathway’s dysfunction can result in an exaggerated inflammatory response in the skin’s hair follicles and sweat glands.
Environmental factors, particularly smoking, obesity, and excessive friction or sweating, are known to increase the risk of HS flare-ups. Hormonal changes, especially those occurring during puberty or menstruation, are also considered important factors in the development of the disease, with many individuals noticing a worsening of symptoms during these times. The inflammation in HS is not caused by bacterial infection, though infected abscesses can develop secondary to the primary condition.
Pathophysiology
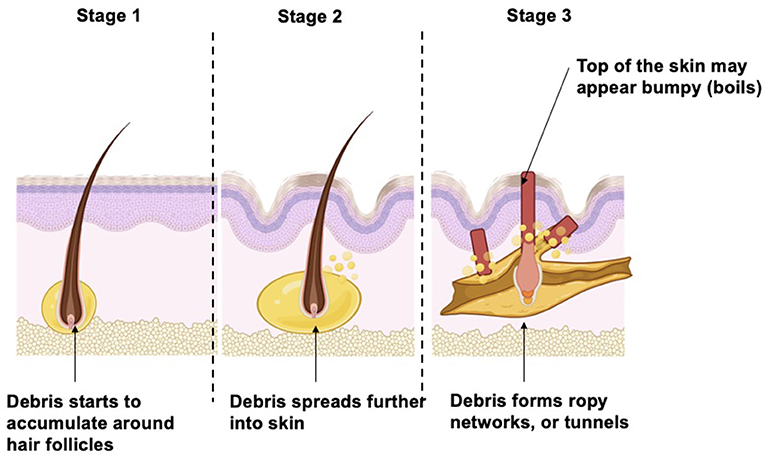
Hidradenitis suppurativa is believed to arise from a combination of hyperkeratinization and inflammation of the hair follicles, particularly in areas of friction. This inflammation leads to the blockage of sweat glands, followed by the formation of painful lumps and abscesses. Over time, these abscesses may rupture, causing the release of pus or blood. Repeated flare-ups lead to the formation of scar tissue, and the development of sinus tracts and fistulas, which are abnormal connections between skin surfaces.
The process is thought to involve an abnormal immune response where the body’s immune system, instead of protecting the skin, triggers inflammation in the affected areas. This chronic inflammation results in the progressive damage to skin structures and the underlying tissue.
Over time, individuals with HS may experience significant scarring, thickened skin, and the development of painful, interconnected tunnels under the skin. In severe cases, extensive scarring can lead to functional and aesthetic impairments, and complications such as secondary infections and mobility limitations may occur.
DSM-5 Diagnosis
Hidradenitis suppurativa is not specifically classified in the DSM-5, as it is a dermatologic condition rather than a psychiatric disorder. Diagnosis is primarily clinical and involves evaluating the patient’s symptoms, medical history, and physical examination findings. No definitive laboratory test or imaging is required for the diagnosis, but it may be confirmed through the identification of characteristic skin lesions in areas of friction.
In some cases, biopsy or culture may be necessary to rule out other conditions or confirm the presence of infection. The diagnosis is typically made based on the presence of recurrent, painful abscesses, sinus tracts, and scarring, often in the armpits, groin, buttocks, and under the breasts. In some cases, associated systemic symptoms such as fever or malaise may also aid in diagnosis.
Treatment Regimens
Management of hidradenitis suppurativa focuses on controlling inflammation, preventing infection, and reducing the frequency and severity of flare-ups. Mild cases may be treated with topical antibiotics or corticosteroids to reduce inflammation and prevent infection. In more severe cases, oral antibiotics such as tetracycline or doxycycline may be prescribed to reduce bacterial colonization and inflammation.
Additionally, biologic agents targeting the immune system, such as adalimumab, have shown promise in reducing flare-ups and managing the condition long-term. Surgical intervention may be necessary in advanced cases to remove abscesses or to drain cysts and sinus tracts. In some instances, patients may require skin grafts to restore the affected areas after significant scarring.
Lifestyle changes, including weight management and smoking cessation, are essential components of treatment to reduce flare-up frequency and severity. Pain management may also be part of the treatment regimen, with nonsteroidal anti-inflammatory drugs (NSAIDs) or opioids being used in severe cases. Early intervention is key to preventing long-term complications and improving quality of life.
Patient Education
Patient education is an integral part of managing hidradenitis suppurativa. Educating patients on the nature of the disease, its triggers, and the importance of early intervention can help reduce the severity of symptoms and improve outcomes.
Smoking cessation is strongly recommended, as tobacco use is a major risk factor for flare-ups. Patients should also be educated on the role of weight management in controlling the condition, as obesity can exacerbate symptoms. In addition, patients should be instructed on proper skin hygiene to reduce irritation and the risk of infection in affected areas. For those with recurrent flare-ups, it is important to avoid tight clothing or friction in areas prone to the condition.
Medications prescribed for HS, including antibiotics or biologics, should be taken as directed, and patients should be aware of potential side effects. In cases of severe disease, patients should be informed about the potential need for surgery, and psychological support may be necessary to address the emotional and social challenges associated with living with a chronic skin condition.
Conclusion
Hidradenitis suppurativa is a chronic and often painful condition that primarily affects areas where skin rubs together, such as the armpits and groin. Although the exact cause remains unclear, it is believed to involve a combination of genetic, environmental, and immunological factors. Early intervention with lifestyle modifications, medications, and, when necessary, surgery, can help manage the disease and improve the quality of life for affected individuals. Educating patients on the importance of avoiding triggers, maintaining proper hygiene, and adhering to treatment plans is essential to managing the condition effectively.
References
Ting, T. Y., & Tey, H. L. (2021). Hidradenitis suppurativa: Epidemiology, pathogenesis, and diagnosis. Journal of Clinical Medicine, 10(11), 2345. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8002679/
Zouboulis, C. C., & Bechara, F. G. (2020). Hidradenitis suppurativa: Current concepts in pathogenesis and treatment. Journal of Dermatology, 47(7), 712-725. https://doi.org/10.1111/1346-8138.15431
Saunte, D. M. L., & Jemec, G. B. E. (2020). Hidradenitis suppurativa: Advances in diagnosis and treatment. Journal of the American Academy of Dermatology, 82(2), 323-333. https://doi.org/10.1016/j.jaad.2019.06.036



