Alterations in Cardiovascular and Respiratory Systems
Alterations in Cardiovascular and Respiratory Systems
(Alterations in Cardiovascular and Respiratory Systems)
Introduction
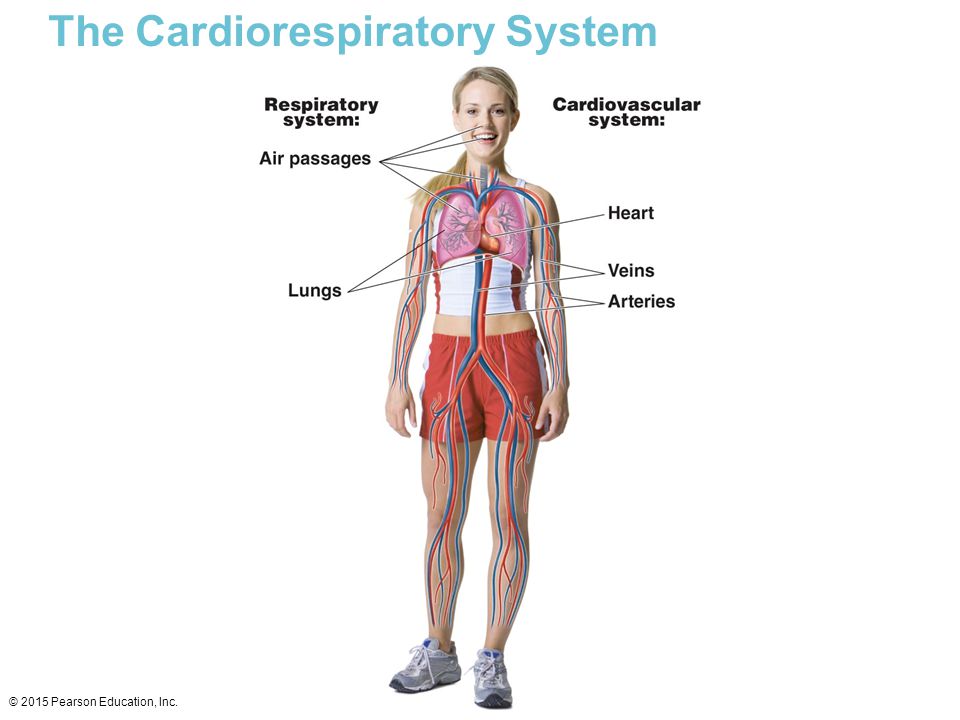
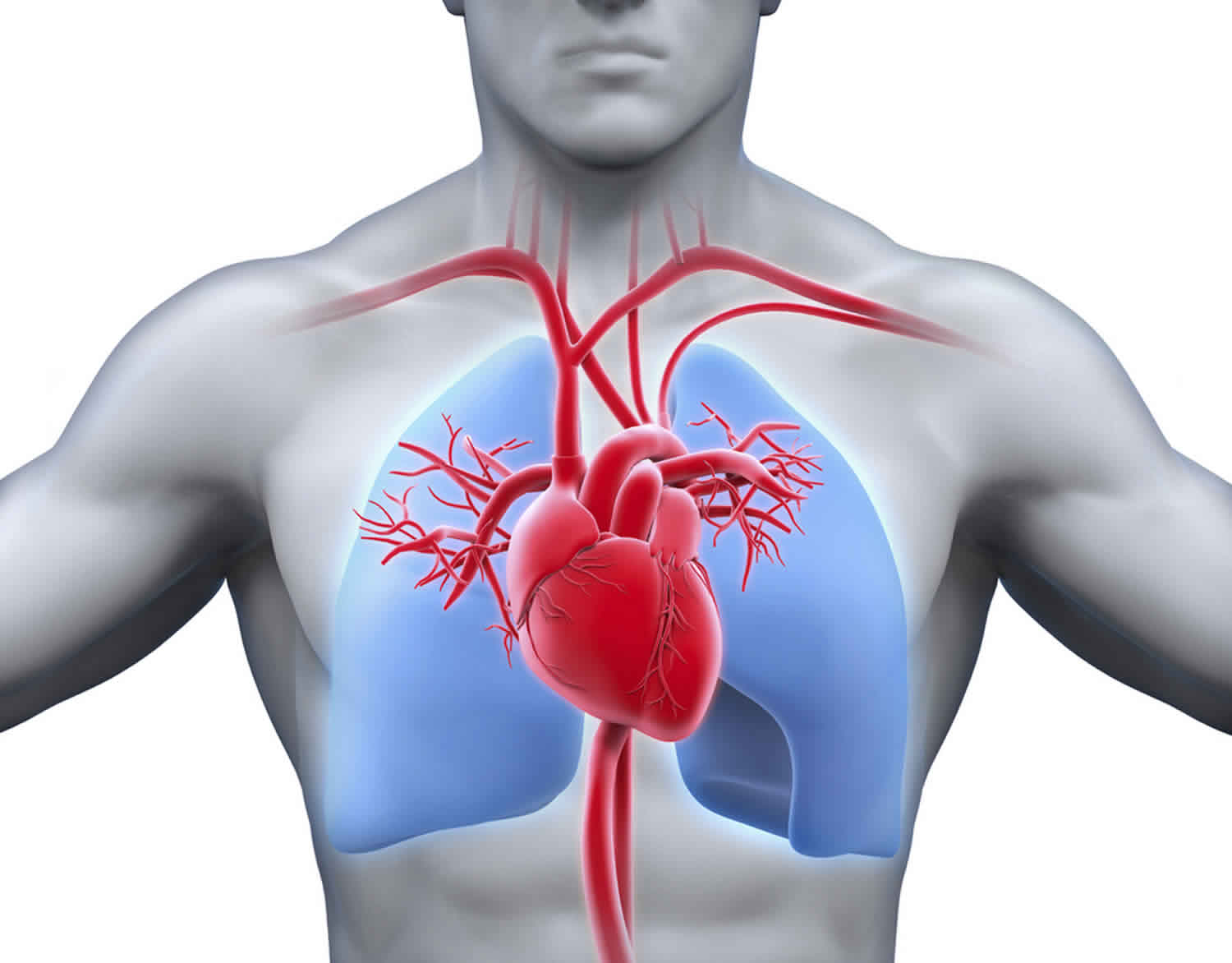
The cardiorespiratory system operates to serve body organs and tissues with enough oxygen supply in relation to oxygen intake. The physiological interactions between the cardiovascular and respiratory systems are complex and fundamental in optimal patient management. Alterations in these systems, for instance, altered intrathoracic pressure, can be transferred to the heart and lungs, dramatically altering cardiovascular performance (Cross et al., 2020). This paper addresses alterations in cardiovascular and respiratory systems, pathophysiological processes in these systems that contribute to disease systems, how the process affects each other, and ethnic/racial that affect physiological functioning. (Alterations in Cardiovascular and Respiratory Systems)
Cardiovascular and cardiopulmonary pathophysiologic processes of why the patient presents these symptoms
The patient has gained weight and is experiencing shortness of breath, peripheral edema, and abdominal swelling. A Framingham study shows that the prevalence of arterial pressure is high among overweight individuals. There is a direct correlation between hypertension and body weight in adults (Mendoza et al., 2020). The patient complains of weight gain, which is a likely cause of increased arterial pressure or hypertension, whose first symptom is shortness of breath (Oldroyd et al., 2022). The peripheral edema can be attributed to the high blood pressure due to constricted veins and arteries because any activity that increases capillary pressure, minimizes oncotic pressure, raises endothelial permeability, or impacts lymphatic drainage, can lead to edema. The abdominal swelling can be as a result of a large amount of fluid accumulating in the abdomen, which can be attributed to portal hypertension. (Alterations in Cardiovascular and Respiratory Systems)
How the cardiovascular and cardiopulmonary pathophysiologic processes interact to affect the patient
This case study depicts an alteration in cardiovascular and respiratory or cardiopulmonary systems as a result of weight gain. According to research, excess weight leads to fatty material build-up in the arteries, increasing arterial pressure because of the contractions in the arteries (Mendoza et al., 2020). The increased arterial pressure is a pathophysiological process of the cardiovascular system that leads to an alteration in the cardiopulmonary processes because the body is struggling to supply cells with adequate oxygen, requiring more blood to supply adequate oxygen (Cross et al., 2020). This alteration in the cardiopulmonary system as a result of the cardiovascular system is linked to the patient experiencing shortness of breath. (Alterations in Cardiovascular and Respiratory Systems)
Racial/ethnic variables that may impact physiological functioning
Most diseases, especially chronic diseases, vary by race and ethnicity. For instance, in the case of cardiovascular diseases, there is a high prevalence of hypertension among black adults, with 59% of black adults experiencing hypertension. Also, the likelihood of developing hypertension is twice among black women than among white women. Type 2 diabetes is more prevalent among American Indians, with 1 in 4 adults developing the disease compared to 1 in 12 whites (Cleveland Clinic, 2022). Regarding heart failure, the risk of a black man experiencing heart failure is 70% compared to a white man and 50% for black women compared with white women (Cleveland Clinic, 2022). Black adults are also more likely to experience coronary artery disease, heart attack, and stroke than other racial and ethnic groups. (Alterations in Cardiovascular and Respiratory Systems)
Modifiable and Non-modifiable Risks
Modifiable factors contributing to these numbers or racial disparities regarding physiological functioning include lifestyles and the living environment that encourages a sedentary lifestyle, minimal physical activity, and unhealthy eating patterns, money and resources to acquire basic needs, quality of education, quality of healthcare in the various communities, resources like nutritious foods, and societal factors like discrimination, violence, and capacity to build supporting relationships (Budreviciute et al., 2020). Some factors, like family history of illness and genetic factors, cannot be modified, but the risk can be reduced by optimizing the modifiable risk factors. (Alterations in Cardiovascular and Respiratory Systems)
Conclusion
Cardiovascular and cardiorespiratory systems interact at an optimal level to ensure optimal body functioning. However, alterations in one system can lead to an alteration in another, contributing to disease systems like shortness of breath, as indicated in the case study. In most cases, cardiovascular pathophysiological processes alter normal cardiorespiratory system functioning. Some races and ethnicities are more likely to develop particular diseases; for instance, black adults are more likely to develop cardiovascular diseases like heart failure, heart attack, stroke, and hypertension, than other races and ethnicities. The risk can be reduced by optimizing modifiable factors like lifestyles, living environment, education level or health literacy, financial ability, and quality of healthcare services. (Alterations in Cardiovascular and Respiratory Systems)
References
Budreviciute, A., Damiati, S., Sabir, D. K., Onder, K., Schuller-Goetzburg, P., Plakys, G., … & Kodzius, R. (2020). Management and prevention strategies for non-communicable diseases (NCDs) and their risk factors. Frontiers in public health, 788.
Cleveland Clinic. (2022). How Race and Ethnicity Impact Heart Disease. https://my.clevelandclinic.org/health/articles/23051-ethnicity-and-heart-disease/
Cross, T. J., Kim, C. H., Johnson, B. D., & Lalande, S. (2020). The interactions between respiratory and cardiovascular systems in systolic heart failure. Journal of Applied Physiology, 128(1), 214-224.
Mendoza, M. F., Kachur, S. M., & Lavie, C. J. (2020). Hypertension in obesity. Current Opinion in Cardiology, 35(4), 389-396.
Oldroyd, S. H., Manek, G., Sankari, A., & Bhardwaj, A. (2022). Pulmonary Hypertension. In StatPearls. StatPearls Publishing.



