Role of the Strategic Planner
2100 word essay.
Create an essay discussing the following:
How has the role of the strategic planner changed over the past several decades? What new skills will be essential for the strategic planner?
How does the scanning process create a “window” to the external environment? How does the window concept help in understanding organizations and the types of information they produce?
Strategic assumptions and how you would respond to them in a strategic planning assessment.
Assignment Expectations
Length: 2100 words.
Structure: Include a Title page, introduction, conclusion and reference page in APA style. These do not count towards the minimum word count for this assignment.
References: Include at least six scholarly sources to support your claims. Reference must be current and within 5 years.

The Evolving Role of Strategic Planners and New Skills Needed
Over the past several decades, the role of strategic planners in organizations has evolved significantly. Initially, strategic planning was focused on setting long-term goals and identifying pathways to achieve them. Planners primarily worked with leadership teams to ensure the organization’s mission and vision were aligned with its operational goals. However, the complexities of the modern business environment have required strategic planners to develop new competencies, including adaptability, data analysis, and cross-disciplinary collaboration. (Role of the Strategic Planner)
Changes in the Role of Strategic Planners
In the past, strategic planners were mainly responsible for forecasting based on historical data, creating static long-term plans, and aligning organizational resources to achieve set goals. Today, their role has expanded to include managing uncertainty and responding to rapid changes in both internal and external environments. The emergence of technology, globalization, and increased competition has reshaped industries, forcing strategic planners to be more agile in their approach.
Modern strategic planners must now be able to deal with dynamic business landscapes, frequently updating their plans and responding to emerging trends. This means they must not only understand the internal workings of their organizations but also have a comprehensive understanding of external forces, such as regulatory changes, market shifts, and technological innovations. For example, digital transformation and the rise of data-driven decision-making have greatly influenced how strategic planners operate. In addition to forecasting, they must now guide organizations in navigating disruptive technologies, often integrating digital strategies into the overall planning process.
Furthermore, strategic planners have become key contributors to risk management. In contrast to the traditional static planning methods, which assumed a relatively predictable future, modern planners must consider a wide range of potential future scenarios, making contingency planning an essential part of their role. This shift reflects the increasing need for strategic flexibility, allowing organizations to quickly pivot in response to unforeseen events, such as economic crises or sudden changes in market demand.
New Skills for Strategic Planners
As the role of strategic planners evolves, so do the skills required for success in the profession. One of the most critical new skills is data analysis. Modern strategic planners must be adept at interpreting vast amounts of data to inform their decision-making processes. The rise of big data and advanced analytics means planners can no longer rely solely on intuition or experience; they must base their strategies on solid, evidence-based insights. By leveraging data, they can identify emerging trends, spot potential risks, and make informed decisions about resource allocation.
In addition to data literacy, strategic planners need strong technological proficiency. The increasing integration of technology in business operations means that planners must be comfortable with digital tools and platforms. For instance, they must be able to use business intelligence software, data visualization tools, and forecasting models to track performance and predict future trends. These technological skills allow planners to move beyond traditional methods of strategy formulation, adopting more agile and responsive approaches to planning.
Another essential skill for modern strategic planners is adaptability. As businesses face faster changes in their environments, planners need the ability to quickly revise strategies in response to new information. This requires a flexible mindset and the capacity to work under pressure, managing both long-term planning and short-term decision-making simultaneously. This adaptability is crucial in industries that experience rapid technological advances or volatile market conditions.
Lastly, strategic planners must excel in communication and collaboration. As organizations become more interdisciplinary, planners must work closely with departments such as finance, marketing, operations, and IT to ensure that strategies are holistic and integrated. Strong interpersonal skills are necessary for gaining buy-in from various stakeholders and ensuring that the strategic plan is effectively executed across the organization.
The Scanning Process and the “Window” to the External Environment
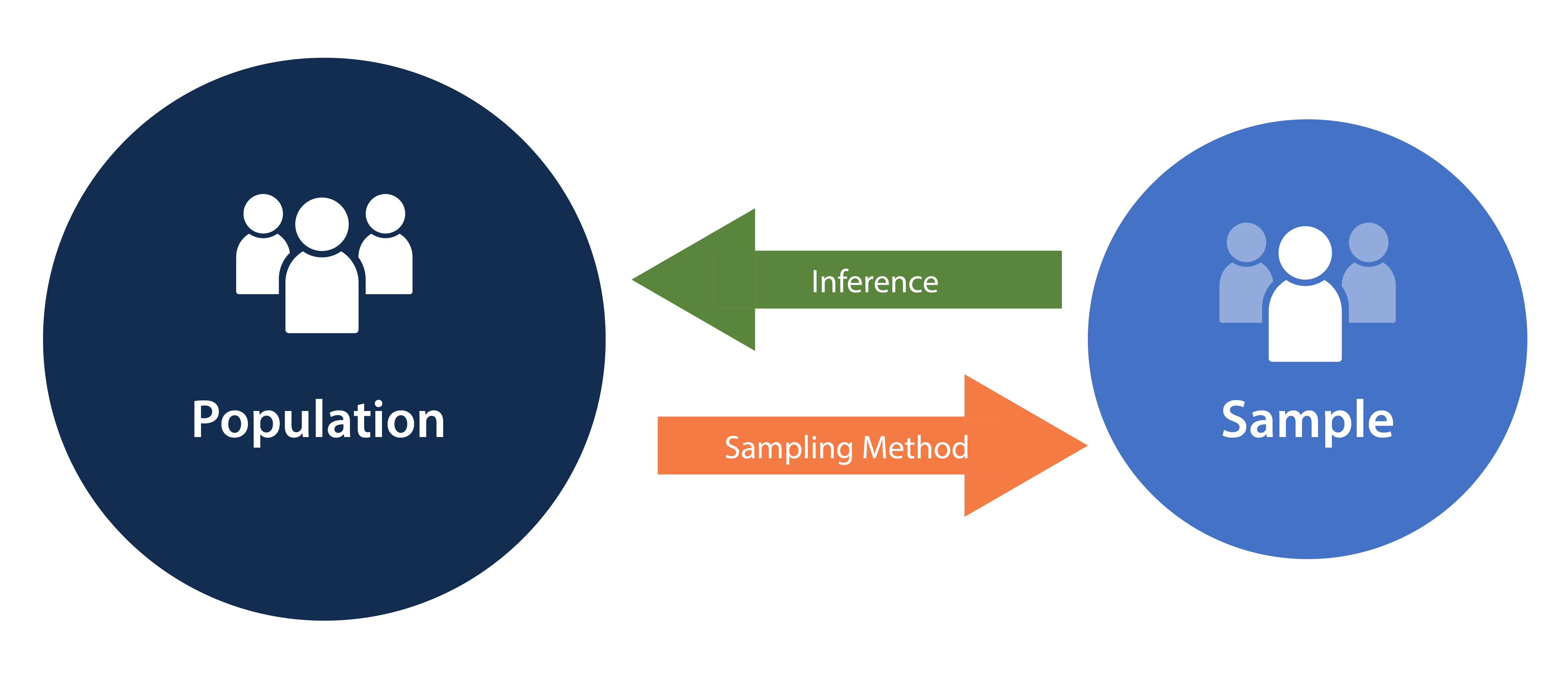
Environmental scanning is a critical tool in strategic planning, providing planners with the ability to monitor and analyze external factors that could impact the organization. The scanning process involves collecting information about trends, opportunities, and threats in the external environment, including political, economic, social, and technological forces. This process creates a “window” to the external environment, offering planners a comprehensive view of factors that may influence the organization’s strategic decisions.
The window concept helps planners understand organizations by allowing them to see beyond the internal operations of the business. It broadens the planner’s perspective, showing how external variables—such as changes in consumer preferences, regulatory updates, or economic fluctuations—affect organizational performance. By looking through this window, strategic planners can make informed decisions that align with both internal goals and external realities. (Role of the Strategic Planner)
For example, a company operating in the healthcare industry might use environmental scanning to identify emerging regulatory changes that could impact their operations. This window to the external environment would allow the company to adapt its strategy to remain compliant while also identifying potential opportunities, such as new market segments or partnerships. The scanning process ultimately enables planners to anticipate changes and stay proactive, rather than merely reacting to external events as they occur.
Strategic Assumptions in a Planning Assessment
Strategic assumptions are beliefs or hypotheses that organizations hold regarding the future conditions in which they will operate. These assumptions can include expectations about market trends, customer behavior, technological advancements, or regulatory environments. Assumptions are an integral part of the strategic planning process, as they form the basis for decision-making and future planning.
In a strategic planning assessment, I would respond to strategic assumptions by critically evaluating their validity and ensuring they are grounded in reliable data. First, I would assess whether the assumptions align with current trends identified through environmental scanning and data analysis. For example, if the assumption is that customer demand for a specific product will increase, I would analyze market data and industry reports to determine whether this expectation is realistic.
Next, I would develop contingency plans for key strategic assumptions. Since assumptions are inherently uncertain, it is important to consider alternative scenarios and plan for different outcomes. This process involves creating “what-if” analyses to evaluate how changes in key assumptions might affect the strategic plan. For instance, if an assumption about future technology adoption does not materialize, the organization needs to be prepared with alternative strategies.
Additionally, I would prioritize flexibility in responding to strategic assumptions. Given the unpredictability of many external factors, it is essential to maintain agility in the strategic plan. I would regularly review and update assumptions as new information becomes available, ensuring that the plan remains relevant and effective over time. This approach allows the organization to stay ahead of potential risks and capitalize on new opportunities as they arise.
Conclusion
The role of strategic planners has evolved from simple forecasting and goal-setting to managing dynamic environments and addressing complex challenges. Modern planners need to be adaptable, data-driven, and technologically proficient to succeed in today’s fast-paced business world. Environmental scanning provides a crucial window into the external environment, helping planners make informed decisions and prepare for future challenges. Strategic assumptions, when carefully evaluated and regularly updated, can guide organizations in navigating uncertainty and ensuring long-term success. As strategic planning continues to evolve, planners will need to embrace these changes and develop the necessary skills to lead organizations toward a sustainable future. (Role of the Strategic Planner)
References
Johnson, G., Scholes, K., & Whittington, R. (2019). Exploring Corporate Strategy: Text & Cases (11th ed.). Pearson Education. https://www.pearson.com/uk/educators/higher-education-educators/product/Johnson-Exploring-Corporate-Strategy-Text-Cases/9781292002545.html
Thompson, A. A., Peteraf, M. A., Gamble, J. E., & Strickland III, A. J. (2020). Crafting & Executing Strategy: The Quest for Competitive Advantage. McGraw-Hill Education. https://www.mheducation.com/highered/product/crafting-executing-strategy-quest-competitive-advantage-concepts-cases-thompson-peteraf/M9781260261529.html
Porter, M. E. (1985). Competitive Advantage: Creating and Sustaining Superior Performance. Free Press. https://www.simonandschuster.com/books/Competitive-Advantage/Michael-E-Porter/9781416595847
Mintzberg, H. (1994). The Rise and Fall of Strategic Planning. Free Press. https://www.simonandschuster.com/books/The-Rise-and-Fall-of-Strategic-Planning/Henry-Mintzberg/9781451697558
Ansoff, H. I., & McDonnell, E. J. (1990). Implanting Strategic Management. Prentice-Hall. https://www.amazon.com/Implanting-Strategic-Management-H-Igor-Ansoff/dp/0134518311
Bryson, J. M. (2018). Strategic Planning for Public and Nonprofit Organizations: A Guide to Strengthening and Sustaining Organizational Achievement. John Wiley & Sons. https://www.wiley.com/en-us/Strategic+Planning+for+Public+and+Nonprofit+Organizations:+A+Guide+to+Strengthening+and+Sustaining+Organizational+Achievement,+5th+Edition-p-9781119071600
Do you need a similar assignment done for you from scratch? Order now!
Use Discount Code "Newclient" for a 15% Discount!