Mrs. Walsh CABG Surgery
Mrs. Walsh CABG Surgery
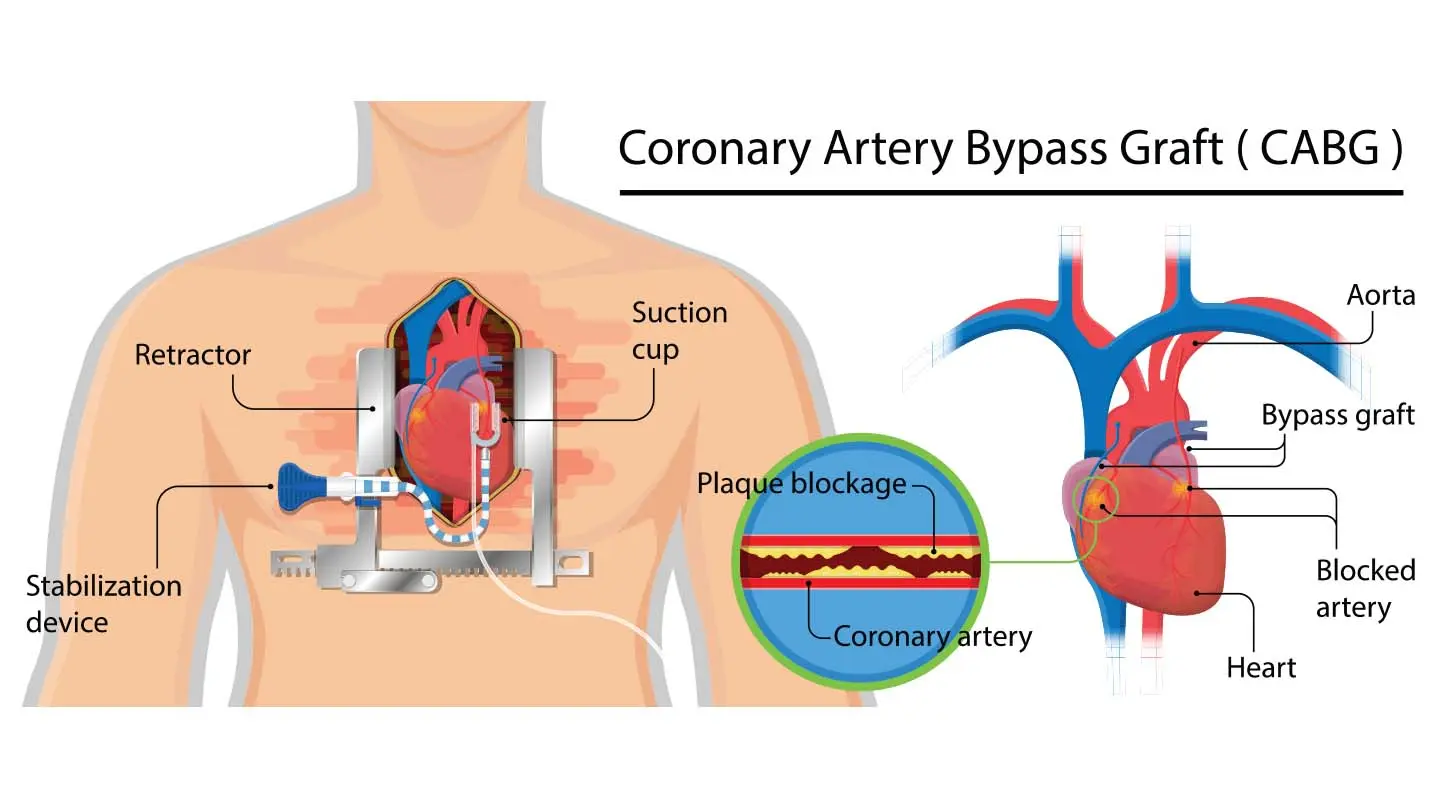
Mrs. Walsh, a woman in her 70s, was in critical condition after repeat coronary artery bypass graft (CABG) surgery. Her family lived nearby when Mrs. Walsh had her first CABG surgery. They had moved out of town but returned to our institution, where the first surgery had been performed successfully. Mrs. Walsh remained critically ill and unstable for several weeks before her death. Her family was very anxious because of Mrs. Walsh’s unstable and deteriorating condition, and a family member was always with her 24 hours a day for the first few weeks.
The nurse became involved with this family while Mrs. Walsh was still in surgery because family members were very anxious that the procedure was taking longer than it had the first time and made repeated calls to the critical care unit to ask about the patient. The nurse met with the family and offered to go into the operating room to talk with the cardiac surgeon to better inform the family of their mother’s status.
One of the helpful things the nurse did to assist this family was to establish a consistent group of nurses to work with Mrs. Walsh, so that family members could establish trust and feel more confident about the care their mother was receiving. This eventually enabled family members to leave the hospital for intervals to get some rest. The nurse related that this was a family whose members were affluent, educated, and well informed, and that they came in prepared with lists of questions. A consistent group of nurses who were familiar with Mrs. Walsh’s particular situation helped both family members and nurses to be more satisfied and less anxious. The family developed a close relationship with the three nurses who consistently cared for Mrs. Walsh and shared with them details about Mrs. Walsh and her life.
The nurse related that there was a tradition in this particular critical care unit not to involve family members in care. She broke that tradition when she responded to the son’s and the daughter’s helpless feelings by teaching them some simple things that they could do for their mother. They learned to give some basic care, such as bathing her. The nurse acknowledged that involving family members in direct patient care with a critically ill patient is complex and requires knowledge and sensitivity. She believes that a developmental process is involved when nurses learn to work with families.
She noted that after a nurse has lots of experience and feels very comfortable with highly technical skills, it becomes okay for family members to be in the room when care is provided. She pointed out that direct observation by anxious family members can be disconcerting to those who are insecure with their skills when family members ask things like, “Why are you doing this? Nurse ‘So and So’ does it differently.” She commented that nurses learn to be flexible and to reset priorities. They should be able to let some things wait that do not need to be done right away to give the family some time with the patient.
(Mrs. Walsh CABG Surgery)
One of the things that the nurse did to coordinate care was to meet with the family to see what times worked best for them; then she posted family time on the patient’s activity schedule outside her cubicle to communicate the plan to others involved in Mrs. Walsh’s care.
When Mrs. Walsh died, the son and daughter wanted to participate in preparing her body. This had never been done in this unit, but after checking to see that there was no policy forbidding it, the nurse invited them to participate. They turned down the lights, closed the doors, and put music on; the nurse, the patient’s daughter, and the patient’s son all cried together while they prepared Mrs. Walsh to be taken to the morgue. The nurse took care of all intravenous lines and tubes while the children bathed her. The nurse provided evidence of how finely tuned her skill of involvement was with this family when she explained that she felt uncomfortable at first because she thought that the son and daughter should be sharing this time alone with their mother.
Then she realized that they really wanted her to be there with them. This situation taught her that families of critically ill patients need care as well. The nurse explained that this was a paradigm case that motivated her to move into a CNS role, with expansion of her sphere of influence from her patients during her shift to other shifts, other patients and their families, and other disciplines.”
Critical thinking activities
- Discuss the clinical narrative provided here using the unfolding case study format to promote situated learning of clinical reasoning (Benner, Hooper-Kyriakidis, & Stannard, 2011).
- Regarding the various aspects of the case as they unfold over time, consider questions that encourage thinking, increase understanding, and promote dialogue, such as: What are your concerns in this situation? What aspects stand out as salient? What would you say to the family at given points in time? How would you respond to your nursing colleagues who may question your inclusion of the family in care?
- Using Benner’s approach, describe the five levels of competency and identify the characteristic intentions and meanings inherent at each level of practice.
References
Benner, P., Hooper-Kyriakidis, P., & Stannard, D. (2011). Clinical wisdom and interventions in critical care: A thought process approach. Jones & Bartlett Learning. https://www.jblearning.com/catalog/productdetails/9781284044192
Cox, C. L., & Kahn, D. L. (2016). Family involvement in care of critically ill patients: An integrative review. American Journal of Critical Care, 25(5), 399-409. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5077376/
Lindley, L. C., & Smith, M. D. (2015). Nursing care of the critically ill: Family-centered care. Nursing Clinics of North America, 50(3), 523-532.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5117861/
Mason, D. J., Leavitt, J. K., & Chaffee, M. W. (2016). Policy & Politics in Nursing and Health Care. Elsevier. https://www.elsevier.com/books/policy-and-politics-in-nursing-and-health-care/mason/978-0-323-39481-2
National Organization of Nurse Practitioner Faculties (NONPF). (2018). Core Competencies for Nurse Practitioners. https://www.nonpf.org/resource/resmgr/competencies/2018_Nonpf_Core_Competencies.pdf