Nursing Paper Example on Keratoconus
Nursing Paper Example on Keratoconus
Nursing Paper Example on Keratoconus
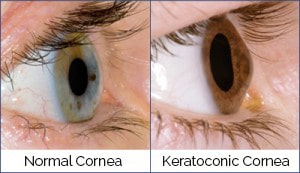
Keratoconus is a progressive eye disorder that causes the cornea to thin and bulge into a cone-like shape. This alteration distorts vision, leading to challenges with everyday activities such as reading or driving. The condition often starts in adolescence or early adulthood and progresses over time, sometimes stabilizing later in life. Advances in diagnostic techniques and treatments have improved outcomes, but early detection remains key to preserving vision.

Causes
The exact cause of keratoconus remains unclear, but both genetic and environmental factors are implicated. Studies indicate a strong genetic predisposition, with 10-15% of affected individuals reporting a family history. Environmental triggers like chronic eye rubbing, associated with allergies or irritants, may exacerbate corneal weakening. Collagen abnormalities within the corneal stroma also contribute. Additionally, oxidative stress is thought to weaken corneal tissue, particularly in genetically susceptible individuals (Gatinel & Saad, 2019).
Signs and Symptoms
Patients with keratoconus often experience blurred or distorted vision, sensitivity to light, and frequent changes in glasses prescriptions. Advanced cases may lead to severe vision impairment and visible corneal protrusion. Symptoms typically worsen in one eye before the other, though both eyes are usually affected. Astigmatism and nearsightedness are common, with some patients reporting “ghosting” or multiple images in their visual field (Paz Filgueira et al., 2021).
Etiology
The etiology of keratoconus involves genetic, biochemical, and mechanical factors. Studies have linked mutations in genes like VSX1 and LOX to the condition. Biochemical studies suggest an imbalance between oxidative damage and protective enzymes in the cornea. Mechanical stress from habits like eye rubbing or contact lens misuse can accelerate corneal thinning and protrusion (McMonnies, 2015). The interplay between these factors underscores the complex nature of keratoconus.
Pathophysiology
Keratoconus is characterized by progressive thinning and biomechanical weakening of the corneal stroma. Collagen fibrils in the cornea lose their structural organization, leading to protrusion and irregular astigmatism. Oxidative stress exacerbates the condition, causing apoptosis of keratocytes and further weakening the corneal matrix. Advanced cases can develop corneal scarring, particularly at the apex of the cone, further reducing visual acuity (Meek et al., 2019).
Diagnosis
Keratoconus is diagnosed through a combination of clinical evaluation and imaging techniques. Slit-lamp examination reveals characteristic signs such as Fleischer rings, Vogt striae, and corneal thinning. Corneal topography remains the gold standard for detecting early-stage keratoconus by mapping corneal curvature. Advanced techniques like Scheimpflug imaging and optical coherence tomography (OCT) provide detailed analysis of corneal thickness and shape, enabling early intervention (Szczotka-Flynn et al., 2020).
Treatment Regimens
Treatment depends on disease severity and progression. In early stages, glasses or soft contact lenses can correct vision. As the condition advances, rigid gas-permeable or scleral lenses may be needed to improve visual acuity. Corneal cross-linking (CXL), a minimally invasive procedure, halts progression by strengthening corneal collagen. In severe cases, surgical interventions like corneal transplants or implantation of intracorneal ring segments (ICRS) are necessary to restore vision (O’Brart, 2021).
Patient Education
Educating patients about keratoconus involves explaining the progressive nature of the disease and the importance of regular eye exams. Patients should avoid eye rubbing to minimize mechanical stress on the cornea. Discussion of treatment options, including benefits and risks, empowers patients to make informed decisions. For those requiring contact lenses, proper care and hygiene are crucial. Genetic counseling may be considered for families with a history of keratoconus (McMonnies, 2015).
Conclusion
Keratoconus is a complex, progressive eye condition that can significantly impair vision if untreated. Advances in diagnostic technologies and treatments, including corneal cross-linking, have improved outcomes. Early detection, combined with patient education and tailored therapies, is essential to preserving vision and quality of life. Further research into its underlying mechanisms may lead to more effective interventions and preventive strategies.
References
Gatinel, D., & Saad, A. (2019). The challenges of diagnosing early keratoconus. Journal of Refractive Surgery, 35(5), 318-319. https://doi.org/10.3928/1081597X-20190422-01
Meek, K. M., & Knupp, C. (2019). Corneal structure and transparency. Progress in Retinal and Eye Research, 49, 1-16. https://doi.org/10.1016/j.preteyeres.2015.08.002
McMonnies, C. W. (2015). Mechanisms of rubbing-related corneal trauma in keratoconus. Cornea, 34(6), 801-806. https://doi.org/10.1097/ICO.0000000000000455
O’Brart, D. P. (2021). Corneal cross-linking: A review. Journal of Cataract and Refractive Surgery, 47(6), 749-769. https://doi.org/10.1097/j.jcrs.0000000000000517
Paz Filgueira, C. L., & de Moura, L. A. (2021). Advances in keratoconus diagnosis and treatment. Arquivos Brasileiros de Oftalmologia, 84(4), 1-12. https://doi.org/10.5935/0004-2749.20210022Szczotka-Flynn, L., Flanagan, J., & Varikooty, J. (2020). Innovations in keratoconus management. Contact Lens & Anterior Eye, 43(5), 431-438. https://doi.org/10.1016/j.clae.2020.01.005