Nursing Paper Example on Adenovirus Infection
Nursing Paper Example on Adenovirus Infection
Adenoviruses are a group of viruses that can cause a variety of infections in humans, primarily affecting the respiratory, gastrointestinal, and ocular systems. Adenovirus infections are common, particularly in children, but they can also occur in adults, especially in crowded settings like military barracks, schools, and hospitals. While most adenovirus infections are self-limiting and mild, they can lead to more severe complications in individuals with weakened immune systems. This paper will explore the causes, signs and symptoms, etiology, pathophysiology, diagnostic criteria, treatment regimens, and patient education for adenovirus infections.
Causes of Adenovirus Infection
Adenovirus infections are caused by the adenovirus family, which consists of over 50 distinct serotypes. These viruses are highly contagious and spread through respiratory droplets, direct contact, or contaminated water. The primary causes of adenovirus infection include:
- Airborne transmission: Adenoviruses are primarily spread via respiratory droplets from coughs and sneezes, making respiratory infections the most common type.
- Fecal-oral transmission: Some serotypes of adenovirus can cause gastrointestinal infections and spread through contaminated food or water.
- Direct contact: Adenovirus can spread through touching surfaces contaminated with the virus, which is why frequent handwashing is important.
- Close contact settings: Crowded environments, such as daycare centers, military barracks, and healthcare facilities, facilitate the transmission of adenovirus infections.
Signs and Symptoms
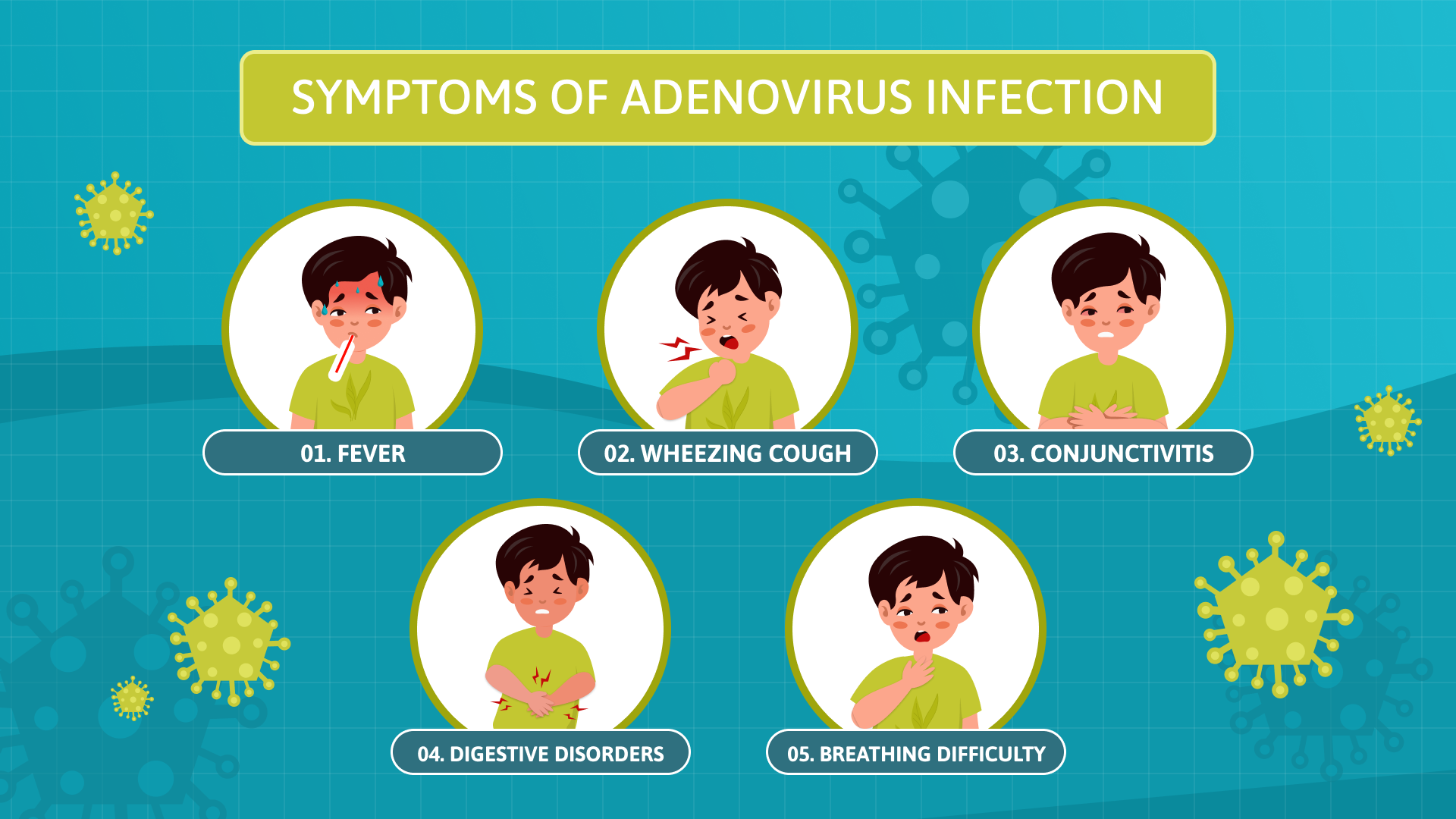
Adenovirus infections can present with a wide range of symptoms depending on the site of infection. Common symptoms include:
- Respiratory symptoms: The most common manifestation of adenovirus infection is respiratory illness, which can range from mild cold-like symptoms to more severe conditions like pneumonia or bronchiolitis. Symptoms may include:
- Fever
- Sore throat
- Runny nose
- Cough
- Shortness of breath
- Gastrointestinal symptoms: Adenoviruses can also cause gastroenteritis, with symptoms such as:
- Diarrhea
- Vomiting
- Abdominal pain
- Nausea
- Ocular symptoms: Some serotypes of adenovirus affect the eyes, causing conjunctivitis or “pink eye.” Symptoms include:
- Red, watery eyes
- Itching or irritation
- Sensitivity to light
- Other symptoms: Adenoviruses can also cause rashes, urinary tract infections, and, in rare cases, encephalitis or myocarditis.
The severity of symptoms can vary depending on the individual’s age, overall health, and immune status. In healthy individuals, adenovirus infections are generally self-limiting, but in immunocompromised patients, they can lead to severe complications.
Etiology
Adenovirus infections are caused by the adenovirus family, which includes types that can infect both humans and animals. The viruses are classified into several groups (A-F) based on their genetic makeup, and each group is associated with different clinical manifestations. The most common serotypes responsible for human infections are:
- Group A (types 12, 18, 31)
- Group B (types 3, 7)
- Group C (types 1, 2, 5)
- Group D (types 8, 19, 37)
Adenoviruses are double-stranded DNA viruses that are relatively stable in the environment, which allows them to persist for extended periods. The presence of specific proteins on the surface of the virus helps it to attach to and enter host cells. Once inside, the virus can replicate and infect a variety of tissues, leading to the diverse range of symptoms observed in adenovirus infections.
Pathophysiology
The pathophysiology of adenovirus infections involves the virus’s interaction with host cells, leading to inflammation and immune response. Adenoviruses primarily infect epithelial cells lining the respiratory tract, gastrointestinal tract, and conjunctiva, but they can also affect other tissues, such as the urinary tract and central nervous system. The process of infection includes the following steps:
- Attachment and entry: The virus enters host cells by binding to specific receptors, such as the coxsackievirus and adenovirus receptor (CAR). Once the virus attaches to the cell, it is internalized through endocytosis.
- Replication: Inside the host cell, the adenovirus genome is uncoated, and viral replication occurs in the nucleus. This process results in the production of new viral particles that are released from the host cell to infect neighboring cells.
- Immune response: The host’s immune system recognizes the infected cells and mounts an inflammatory response. This response includes the activation of immune cells such as T lymphocytes and the release of cytokines. While the immune system works to clear the infection, this immune response contributes to the symptoms of inflammation, such as fever and swelling.
DSM-5 Diagnosis
Adenovirus infections are not specifically addressed in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5), as it is a physical viral infection and not a psychiatric disorder. The diagnosis of adenovirus infection is typically based on clinical evaluation, laboratory tests, and imaging studies.
- Clinical evaluation: Physicians assess the patient’s symptoms, medical history, and possible exposure risks (e.g., close contact settings, recent travel to endemic areas).
- Laboratory tests: Diagnosis can be confirmed by detecting adenovirus DNA or antigens in patient samples. Polymerase chain reaction (PCR) testing is the gold standard for detecting adenovirus in respiratory, stool, or ocular samples.
- Imaging studies: In severe cases, such as pneumonia or other systemic manifestations, chest X-rays or CT scans may be used to assess the extent of the infection.
Treatment Regimens
Most adenovirus infections are self-limiting and require only supportive care. However, treatment approaches may vary depending on the severity of the infection and the patient’s immune status:
- Supportive care: For mild respiratory or gastrointestinal symptoms, the mainstay of treatment is hydration, rest, and fever control with antipyretics such as acetaminophen or ibuprofen. In some cases, cough medications and decongestants may be used.
- Antiviral therapy: In severe cases, especially in immunocompromised individuals, antiviral drugs such as cidofovir or brincidofovir may be used. These antiviral agents can inhibit adenovirus replication but are typically reserved for patients who are at high risk for complications.
- Ocular treatment: For adenoviral conjunctivitis, treatment focuses on symptom relief with lubricating eye drops, antihistamines, and sometimes topical corticosteroids to reduce inflammation.
In patients with severe infections, such as pneumonia, hospitalization and more aggressive treatment may be required, including mechanical ventilation or antiviral therapy.
Patient Education
Patient education is crucial in preventing the spread of adenovirus infections and promoting proper management. Key areas of education include:
- Hygiene practices: Since adenoviruses are transmitted through respiratory droplets and contaminated surfaces, patients should be educated on the importance of frequent handwashing, especially after coughing or sneezing.
- Avoiding close contact: Individuals with adenovirus infections should avoid close contact with others, particularly those in vulnerable groups, such as infants, the elderly, and immunocompromised individuals.
- Recognizing symptoms: Patients should be informed about the common symptoms of adenovirus infection, including respiratory, gastrointestinal, and ocular signs, and encouraged to seek medical care if they experience severe symptoms.
- Vaccination: While there is currently no vaccine for adenovirus infections in the general population, military personnel may receive an adenovirus vaccine (types 4 and 7) to prevent respiratory illness caused by these serotypes. Patients should be informed about available preventive measures in specific settings, such as military or healthcare facilities.
Conclusion
Adenovirus infections are a common and diverse group of viral infections that can affect various systems in the body. While most cases are mild and self-limiting, severe infections can occur, particularly in immunocompromised individuals. Early diagnosis, supportive care, and appropriate management are essential to prevent complications. Understanding the transmission, symptoms, and treatment options for adenovirus infections can help reduce the spread of the virus and improve patient outcomes.
References
Ksiazek, T. G., & Shieh, W. J. (2000). Adenovirus. In Infectious Diseases of the Respiratory Tract (pp. 403-413). Springer. https://doi.org/10.1007/978-1-4612-1461-9_28
Lee, J. S., & Dittmer, D. P. (2015). Adenovirus infections. Current Opinion in Virology, 15, 54-59. https://doi.org/10.1016/j.coviro.2015.07.003
Monto, A. S. (2004). Seasonal variation in the epidemiology of respiratory adenovirus infections. Journal of Clinical Microbiology, 42(5), 2200-2203. https://doi.org/10.1128/JCM.42.5.2200-2203.2004
Allington, J. P., & McKinnon, P. (2016). Adenovirus: Diagnosis and clinical considerations. Journal of Clinical Virology, 74, 48-53. https://doi.org/10.1016/j.jcv.2015.12.011