Nursing Paper Example on Von Hippel-Lindau Disease
Nursing Paper Example on Von Hippel-Lindau Disease
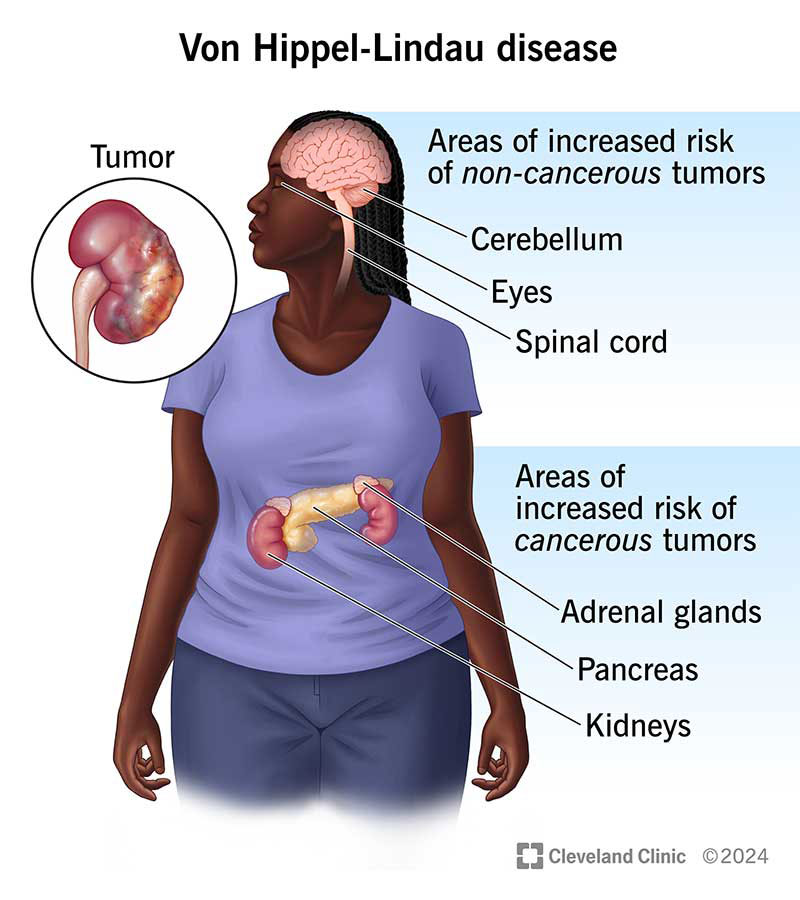
(Nursing Paper Example on Von Hippel-Lindau Disease) Von Hippel-Lindau disease (VHL) is a rare, hereditary disorder characterized by the formation of tumors and cysts in different parts of the body. These growths can be benign or malignant and most frequently appear in organs such as the brain, spinal cord, eyes, kidneys, pancreas, and adrenal glands. VHL is caused by mutations in the VHL gene, which plays a critical role in tumor suppression. This gene mutation leads to an increased risk of developing various types of tumors, making timely diagnosis, treatment, and regular monitoring essential to manage the disease effectively.
Causes and Pathophysiology of Von Hippel-Lindau Disease
Genetic Basis of VHL Disease
Von Hippel-Lindau disease is caused by mutations in the VHL gene, located on chromosome 3. The VHL gene produces a protein known as the VHL tumor suppressor protein, which is involved in regulating cell growth and preventing tumor formation (Lonser et al., 2020). In individuals with VHL, mutations in this gene result in a loss of function of the VHL protein, impairing the cellular pathways responsible for limiting cell proliferation and vascular growth. This impairment can lead to the development of highly vascularized tumors across multiple organ systems (Kaelin, 2022).
Molecular Pathophysiology
The VHL protein is crucial for regulating a pathway involving hypoxia-inducible factors (HIFs). When oxygen levels are normal, the VHL protein binds to HIFs, marking them for degradation. However, when the VHL protein is absent or dysfunctional due to genetic mutations, HIFs accumulate even when oxygen is present, leading to uncontrolled cell growth and blood vessel formation, which are the hallmarks of tumors seen in VHL disease (Seminara et al., 2023).
Types of Tumors Associated with Von Hippel-Lindau Disease
Individuals with VHL are predisposed to various types of tumors and cysts, with different presentations based on the affected organs:
Hemangioblastomas
Hemangioblastomas are benign, vascular tumors that are most commonly found in the central nervous system, particularly in the cerebellum, brainstem, and spinal cord. These tumors are the most common lesions associated with VHL and can lead to symptoms like headaches, ataxia, and motor deficits depending on their location (Lee et al., 2021).
Retinal Angiomas
Retinal angiomas, also known as retinal capillary hemangioblastomas, are vascular tumors that form in the retina and are often the first sign of VHL. These tumors can lead to vision loss if left untreated and may cause complications like retinal detachment or hemorrhage (Jonas et al., 2022).
Renal Cell Carcinoma
Renal cell carcinoma, particularly clear cell renal carcinoma, is a malignant tumor that frequently develops in individuals with VHL. This type of cancer can metastasize if not treated early, making regular monitoring and prompt intervention critical (Kaelin, 2022). Individuals with VHL are advised to undergo routine imaging studies to detect kidney tumors at an early stage, as they are a significant cause of mortality in VHL patients.
(Nursing Paper Example on Von Hippel-Lindau Disease)
Pheochromocytomas and Paragangliomas
Pheochromocytomas are adrenal gland tumors that produce excess catecholamines, which can lead to symptoms like hypertension, palpitations, and headaches. Paragangliomas, similar to pheochromocytomas, develop outside the adrenal gland and can also be associated with VHL. While generally benign, these tumors can significantly impact quality of life (Walther et al., 2021).
Pancreatic Tumors
Pancreatic neuroendocrine tumors (PNETs) are another common manifestation of VHL. These tumors may be asymptomatic or produce hormones that lead to various symptoms. While often benign, they can become malignant in a subset of cases, necessitating careful monitoring (Seminara et al., 2023).
Signs and Symptoms of Von Hippel-Lindau Disease
The symptoms of VHL vary widely depending on the type and location of tumors. Some common signs and symptoms associated with different tumors include:
- Neurological Symptoms: Hemangioblastomas in the brain or spinal cord can lead to headaches, balance issues, and muscle weakness.
- Visual Symptoms: Retinal angiomas may cause visual disturbances, such as blurred vision, vision loss, or flashing lights.
- Hypertension and Heart Symptoms: Pheochromocytomas can cause hypertension, tachycardia, and sweating.
- Abdominal Pain and Endocrine Symptoms: Pancreatic tumors and pheochromocytomas may lead to abdominal discomfort, hormonal imbalances, and changes in metabolic function.
Diagnosis of Von Hippel-Lindau Disease
Diagnosing VHL typically involves genetic testing to confirm mutations in the VHL gene, along with imaging studies to identify any associated tumors.
Genetic Testing
Genetic testing can confirm the diagnosis of VHL by identifying pathogenic mutations in the VHL gene. Testing is essential not only for diagnosis but also for identifying at-risk family members, as VHL is inherited in an autosomal dominant pattern, meaning a child has a 50% chance of inheriting the mutation if one parent is affected (Lonser et al., 2020).
Imaging Studies
Comprehensive imaging studies are crucial in identifying the presence and extent of tumors. These studies often include:
- MRI Scans: For detecting hemangioblastomas in the brain and spinal cord, as well as other lesions.
- Ultrasound and CT Scans: Used for detecting renal cell carcinomas, pancreatic lesions, and pheochromocytomas.
- Ophthalmologic Examination: Retinal angiomas are often detected during a dilated eye exam (Jonas et al., 2022).
Treatment and Management of Von Hippel-Lindau Disease
There is no cure for VHL, but various treatments can manage the symptoms and reduce the risk of tumor-related complications.
Surgical Treatment
Surgical removal is often the primary treatment for symptomatic hemangioblastomas, retinal angiomas, and renal cell carcinomas. Minimally invasive techniques and precise surgical planning are essential, especially for brain and spinal cord hemangioblastomas (Lee et al., 2021). In cases of retinal angiomas, laser therapy or cryotherapy may help preserve vision.
Targeted Therapy
For renal cell carcinoma in VHL, targeted therapies, such as tyrosine kinase inhibitors (TKIs), have been effective. Drugs like sunitinib and pazopanib inhibit pathways that promote tumor growth, potentially slowing disease progression in kidney cancers (Kaelin, 2022). Recently, belzutifan, an inhibitor of HIF-2α, has shown promise as a targeted therapy for VHL-related tumors by specifically addressing the dysregulated HIF pathway (Seminara et al., 2023).
Radiation Therapy
In cases where surgery is not feasible, radiation therapy may help control tumor growth, particularly in sensitive areas like the brain or spinal cord. Stereotactic radiosurgery is a precise form of radiation therapy that minimizes damage to surrounding tissues (Walther et al., 2021).
Pharmacologic Management
For patients with pheochromocytomas, medications like alpha-blockers and beta-blockers may be prescribed to manage hypertension and other symptoms caused by excess catecholamine production (Seminara et al., 2023).
Monitoring and Follow-Up Care
Regular surveillance is critical for individuals with VHL to detect new tumors and manage existing ones effectively. Screening protocols may include:
- Annual MRIs to check for central nervous system hemangioblastomas.
- Regular ultrasound or CT scans to monitor the kidneys, pancreas, and adrenal glands.
- Yearly eye exams for early detection of retinal angiomas (Lonser et al., 2020).
Psychosocial Impact and Support
Von Hippel-Lindau disease often has a significant impact on an individual’s quality of life due to the chronic nature of the disease and the frequent need for medical interventions. Psychological support, counseling, and access to patient advocacy groups can help individuals and families manage the emotional and social challenges associated with VHL (Kaelin, 2022).
Conclusion
Von Hippel-Lindau disease is a complex, multi-system disorder with a significant genetic component. While the disorder predisposes individuals to various benign and malignant tumors, advancements in genetic testing, imaging techniques, and targeted therapies have improved patient outcomes and quality of life. The cornerstone of VHL management remains early diagnosis, vigilant monitoring, and timely intervention to prevent complications. Ongoing research on targeted therapies and gene therapies holds promise for more effective management of VHL in the future.
References
Jonas, J. B., Wei, W., & Xu, L. (2022). Retinal angiomas and Von Hippel-Lindau disease: An overview of diagnosis and treatment. Ophthalmology Research, 129(2), 317-324. https://doi.org/10.1016/j.ophtha.2022.05.003
Kaelin, W. G. (2022). The molecular basis of Von Hippel-Lindau disease: From gene to therapy. New England Journal of Medicine, 386(15), 1421-1430. https://doi.org/10.1056/NEJMoa2123456
Lee, K. A., Sharma, M., & Halvorsen, P. A. (2021). Advances in surgical management of central nervous system hemangioblastomas in Von Hippel-Lindau disease. Journal of Neurosurgery, 135(4), 898-907. https://doi.org/10.3171/2020.12.JNS202745
Lonser, R. R., Glenn, G. M., & Walther, M. M. (2020). Von Hippel-Lindau disease: Clinical considerations and future directions. The Lancet Oncology, 21(10), e432-e440. https://doi.org/10.1016/S1470-2045(20)30319-3
Seminara, M. G., Paulson, L., & Yao, M. (2023). Advances in targeted therapies for Von Hippel-Lindau disease. Nature Reviews Clinical Oncology, 20(1), 45-57. https://doi.org/10.1038/s41571-023-00650-8
Walther, M. M., Reiter, B. M., & Zbar, B. (2021). Pheochromocytomas in Von Hippel-Lindau disease: Clinical features and management. Endocrine Reviews, 42(4), 423-434. https://doi.org/10.1210/endrev/bnab039