Nursing Paper Example on Dysautonomia
Nursing Paper Example on Dysautonomia
Dysautonomia refers to a group of disorders that affect the autonomic nervous system, responsible for controlling involuntary bodily functions such as heart rate, blood pressure, digestion, and temperature regulation. The condition can manifest in various forms and degrees of severity, ranging from mild to life-altering.
Causes of Dysautonomia
The causes of dysautonomia depend on the specific type of the disorder. Some cases arise due to genetic predisposition, while others develop secondary to other conditions or triggers. Key causes include:
- Primary Dysautonomia:
Genetic mutations, such as those seen in familial dysautonomia (Riley-Day syndrome).
Autoimmune dysfunction, as observed in autoimmune autonomic ganglionopathy.
- Secondary Dysautonomia:
Chronic illnesses such as diabetes, Parkinson’s disease, or multiple sclerosis.
Physical trauma or spinal cord injuries.
Viral infections, including Epstein-Barr virus and COVID-19.
Exposure to toxins or certain medications.
The underlying mechanism typically involves damage, degeneration, or dysfunction of the autonomic nerves or their receptors (National Institute of Neurological Disorders and Stroke [NINDS], 2023).
Signs and Symptoms of Dysautonomia
Dysautonomia can present with a broad spectrum of symptoms that vary based on the affected autonomic functions. Common signs include:
- Cardiovascular Symptoms:
Orthostatic hypotension: A sudden drop in blood pressure upon standing.
Tachycardia or bradycardia.
- Gastrointestinal Symptoms:
Gastroparesis: Delayed stomach emptying leading to nausea, bloating, and vomiting.
Diarrhea or constipation.
- Neurological Symptoms:
Dizziness or fainting (syncope).
Headaches and fatigue.
- Other Symptoms:
Heat intolerance and abnormal sweating.
Bladder dysfunction.
Difficulty regulating body temperature.
The severity and combination of symptoms can vary significantly among individuals.
Types of Dysautonomia
Several forms of dysautonomia exist, each with unique characteristics. Common types include:
- Postural Orthostatic Tachycardia Syndrome (POTS):
Affects mostly young women and causes an abnormal increase in heart rate upon standing.
- Multiple System Atrophy (MSA):
A rare neurodegenerative disorder with autonomic failure and motor dysfunction.
- Neurocardiogenic Syncope:
Leads to fainting episodes triggered by stress, pain, or prolonged standing.
- Familial Dysautonomia (Riley-Day Syndrome):
A genetic condition primarily affecting individuals of Ashkenazi Jewish descent.
- Autoimmune Autonomic Ganglionopathy:
An autoimmune condition where antibodies attack autonomic nerve receptors.
Each type has distinct features and may require tailored treatment.
Pathophysiology of Dysautonomia
The autonomic nervous system is divided into the sympathetic and parasympathetic branches. Dysautonomia arises from the imbalance or failure of these systems, which may involve:
- Nerve Degeneration:
Loss of nerve fibers in the autonomic ganglia or peripheral nerves, as seen in MSA.
- Immune-Mediated Damage:
Antibody attacks on acetylcholine receptors, leading to autonomic dysfunction.
- Abnormal Reflexes:
Dysregulated baroreceptor reflexes cause blood pressure instability.
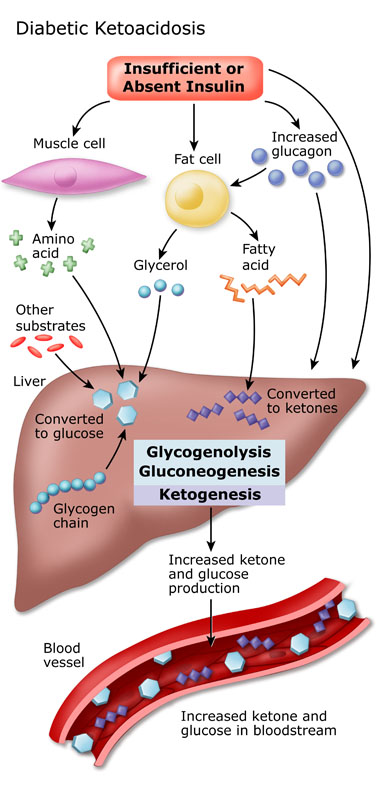
- Metabolic Impairment:
Poor glucose metabolism in diabetes-induced autonomic neuropathy.
These abnormalities lead to systemic dysregulation of multiple physiological functions.
Diagnosis of Dysautonomia
Diagnosing dysautonomia is challenging due to its diverse presentation. Common diagnostic methods include:
- Clinical History:
Detailed evaluation of symptoms and their progression.
- Autonomic Testing:
Tilt table test to assess blood pressure and heart rate responses.
Sweat tests to evaluate sudomotor function.
Heart rate variability and Valsalva maneuver.
- Blood Tests:
To rule out secondary causes like infections, autoimmune disorders, or metabolic issues.
- Imaging:
MRI or CT scans to identify structural abnormalities in the brain or spinal cord.
Collaborative care involving neurologists, cardiologists, and other specialists is often required for an accurate diagnosis.
Treatment Regimens for Dysautonomia
Treatment for dysautonomia is individualized, focusing on symptom management and addressing the underlying cause.
Lifestyle Modifications
Increased salt and fluid intake to improve blood volume and prevent orthostatic hypotension.
Compression garments to enhance venous return.
Regular exercise tailored to the patient’s capacity.
Medications
- Cardiovascular Drugs:
Midodrine for low blood pressure.
Beta-blockers for heart rate control in POTS.
- Neurological Medications:
Gabapentin or pregabalin for neuropathic pain.
Immunosuppressants for autoimmune causes.
- Gastrointestinal Treatments:
Prokinetics like metoclopramide for gastroparesis.
Laxatives or antidiarrheal agents as needed.
Physical Therapy
Recumbent or water-based exercises to improve cardiovascular fitness without triggering symptoms.
Advanced cases, such as MSA, may require palliative care to address progressive disability.
Complications Associated with Dysautonomia
Untreated dysautonomia can lead to significant complications, including:
Chronic fatigue and reduced quality of life.
Recurrent syncope, increasing the risk of falls and injuries.
Progressive organ dysfunction in neurodegenerative forms.
Prompt diagnosis and treatment are essential to mitigate these risks.
Prognosis
The prognosis for dysautonomia varies based on the underlying cause. While conditions like POTS often respond well to treatment, neurodegenerative forms like MSA have a poorer outlook due to their progressive nature.
Patient Education
Education is vital for effective dysautonomia management. Patients should:
Understand their condition and triggers for symptom exacerbation.
Follow prescribed treatment plans and attend regular follow-ups.
Maintain a healthy lifestyle and monitor hydration and nutrition.
Support groups and resources from organizations like Dysautonomia International can provide additional support.
Conclusion
Dysautonomia encompasses a range of disorders with diverse causes, symptoms, and outcomes. Comprehensive management involves accurate diagnosis, symptom control, and addressing the underlying etiology. With appropriate care, many individuals with dysautonomia can achieve improved function and quality of life.
References
Dysautonomia International. (2023). What is Dysautonomia?
https://www.dysautonomiainternational.org
National Institute of Neurological Disorders and Stroke (NINDS). (2023). Dysautonomia Information Page.
https://www.ninds.nih.gov
Mayo Clinic. (2023). Dysautonomia: Symptoms and Causes.
https://www.mayoclinic.org
Cleveland Clinic. (2023). Dysautonomia: Types, Symptoms, Causes, Diagnosis & Treatment.
https://my.clevelandclinic.org