Managing Pediatric Urinary Tract Infection
PEER 11. The nurse needs to familiarize with the history of symptoms exhibited by Shelly. For instance, the nurse needs information on the young girl’s urine color. Urine concentration and description of cloudiness are equally relevant assessment factors because she already knows there is increased volume and urgency (Masika & Armstrong, 2017). Hourly visits to the bathroom are a critical indicator that there could be a urinary tract infection (UTI) but additional assessment details such as odor would provide further information to help assess gravity, diagnosis and subsequent care and treatment. (Managing Pediatric Urinary Tract Infection)
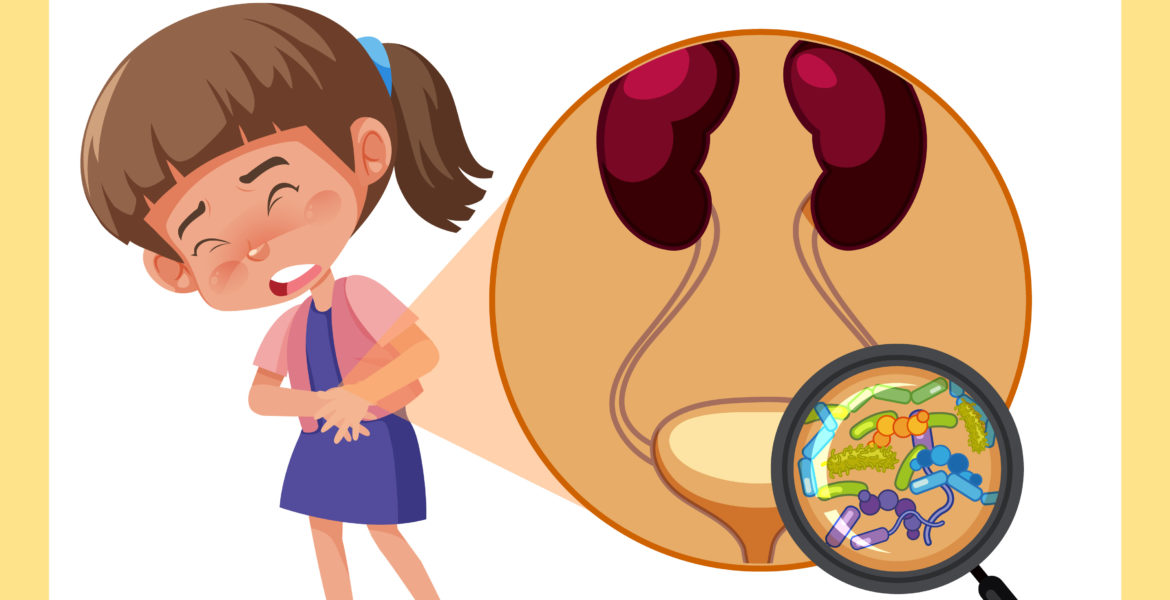
Escherichia coli is a typical causative microorganism that is responsible for the urinary tract infection (UTI). Klebsiella is equally culpable for UTI as well as Proteus spp, although they mostly suggest the presence of stone disease (Taylor & Moore, 2018). The increased levels of gram-positive bacteria also show that enterococcus and staphylococcus are microorganisms related to UTI.
The four-year-old Shelly needs antibiotics to address her situation. Some of the ideal medications include trimethoprim or sulfamethoxazole, which exist as Bactrim or Septra. The alternative pharmacological treatment is amoxicillin or clavulanate, alternatively known as Augmentin (Taylor & Moore, 2018). Cephalosporins such as Suprax, cefprozil, and Keflex are equally effective medication to treat the UTI infection.
Shelly and her parents require patient education to minimize exposure to the causative microorganisms. For instance, Shelly needs information such as wiping strategy after urination or bowel movement. As a child, she might not be acquainted with the recommended front to back technique. The frequent urination on an hourly basis means Shelly needs an equally habitual intake of fluids such as cranberry juice (Masika & Armstrong, 2017). The teaching priorities should focus on behavioral changes for Shelly in the daycare. Minimizing exposure and high levels of sanitation at the facility will reduce or eliminate the recurrence of UTI. (Managing Pediatric Urinary Tract Infection)
PEER 2. In this case study, 4-year-old preschooler Shelly’s mother has reported to the nurse practitioner that Shelly has urinary frequency, painful urination, and fever spike that return to an elevated baseline a few hours of being administered an antipyretic (Tylenol). These are classic signs and symptoms of a urinary tract infection (UTI) (CDC, 2017). It’s important to note that a diagnosis of a UTI, especially in a child, will need further assessment and evaluation. These symptoms alone are not enough to diagnose Shelly. In order to diagnose Shelly with a UTI, the nurse practitioner should take appropriate measures with the aim to assess the external genitalia and palpate the abdomen, suprapubic region, and costovertebral angles to elicit tenderness (Schmidt & Copp, 2015). Redness of the external vagina, foul-smelling discharge, and tenderness of the vagina to touch may further indicate a UTI and assist with a proper diagnosis (CDC, 2017).
Additionally, the healthcare provider will need urinary analysis, imaging of the urinary tract, and blood tests to confirm their diagnosis. Urinary culture and sensitivity can reveal the causative microorganism of Shelly’s UTI and is pivotal in the diagnosis and treatment of a UTI (White, 2011). The most common microorganism that causes a UTI is the bacterium Escherichia coli (E. Coli) and is the causative microorganism of 85 percent of cases of UTI in the pediatric population (CDC, 2017). E. coli is commonly found in the G.I tract and feces. In women and girls, improper perineal care is the primary way E. coli spread from the anus (after a bowel movement) to the vaginal canal (Robinson, Finlay, Lang, Bortolussi, & Canadian Paediatric Society, Infectious Diseases and Immunization Committee, Community Paediatrics Committee, 2014).
Anatomically, the short distance between the urethra and the bladder in girls and women accounts for the higher rate of UTI in this population group than that of boys and men. For a young child like Shelly, medication dosing must be prescribed with careful and special precautions. Ordering the lowest therapeutic dose with little to no adverse effect is the primary goal when prescribing medication in children. It’s important to note the narrow therapeutic index of medication for children, in which drug toxicity is possible with only a slightly higher than the recommended dose. If the urine analysis and urinary culture and sensitivity indicate the presence of E. coli as the causative microorganism, an antibiotic should be prescribed.
In the past, amoxicillin used to be prescribed with the dose based on body weight in kg, but due to the recent high rate of E. coli resistance to amoxicillin, alternate antibiotics have been prescribed for children with UTI. According to White (2011), combination therapy of amoxicillin with clavulanate (Augmentin) prescribed as 25-45 mg/kg/day q12h is more effective than prescribing amoxicillin alone. Cephalosporins are recognized as the drug of choice for UTI in children. If I was the practitioner, I would prescribe cefixime (Suprax) 8 mg/kg every 24 hours divided into every 12 hours for 5-7 days as recommended by White (2011) due to the low dosage compared to other antibiotics. The adverse effect of flatulence and abdominal pain one may experience when taking cefixime is surprisingly more bearable than the nausea and vomiting one may experience when taking Augmentin.
Prior to discharging Shelly from the clinic, as a nurse practitioner, patient and family teaching are very important. Even though she is only 4 years old, Shelly is at the age in which she is potty-trained and goes to the bathroom on her own. In a child-friendly way with simple and clear very directions, Shelly should be told to avoid holding her pee and to use the bathroom as soon as she feels she has to go. When at the daycare, she should ask her teachers to use the bathroom and not hold her urine for long.
Shelly should be instructed to wipe from front to back to avoid spreading bacteria to her vaginal area. Cranberry juice has been proven to help with urinary tract infections with getting rid of the bacteria and managing the symptom dysuria and frequency. Shelly’s mother can be instructed to give Shelly cranberry juice to drink throughout the day. For children, cranberry can be too tart and they may not enjoy drinking it. Shelly’s mother can be instructed to dilute cranberry juice with water for Shelly to have at lunch.
Cotton underwear has been asserted to prevent against incidences of UTI. Shelly’s mother should be instructed to make her daughter only wear cotton panties. Sugary food and beverages, bubble baths, perfumed soaps, tight-fitting clothes, and spicy foods all can contribute to making UTI worse and should be avoided by Shelly (Figueroa, 2016). As stopping antibiotics before treatment is finished can lead to resistance, Shelly’s mother should be instructed to complete the full course of treatment. Re-evaluation by urine culture and analysis should be done a week after the end of treatment and a follow-up appointment is necessary. (Managing Pediatric Urinary Tract Infection)
References
Figueroa, C. A. (2016). Pediatric urinary tract infections: An overview. American Family Physician, 94(5), 350-357.
https://www.aafp.org/pubs/afp/issues/2016/0901/p350.html
Robinson, J. A., Finlay, J. C., Lang, M., Bortolussi, R. A., & Canadian Paediatric Society, Infectious Diseases and Immunization Committee, Community Paediatrics Committee. (2014). Guidelines for the management of urinary tract infections in children. Paediatrics & Child Health, 19(4), 205-217. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3996145/



