Nursing Paper Example on Addison’s Disease
Nursing Paper Example on Addison’s Disease
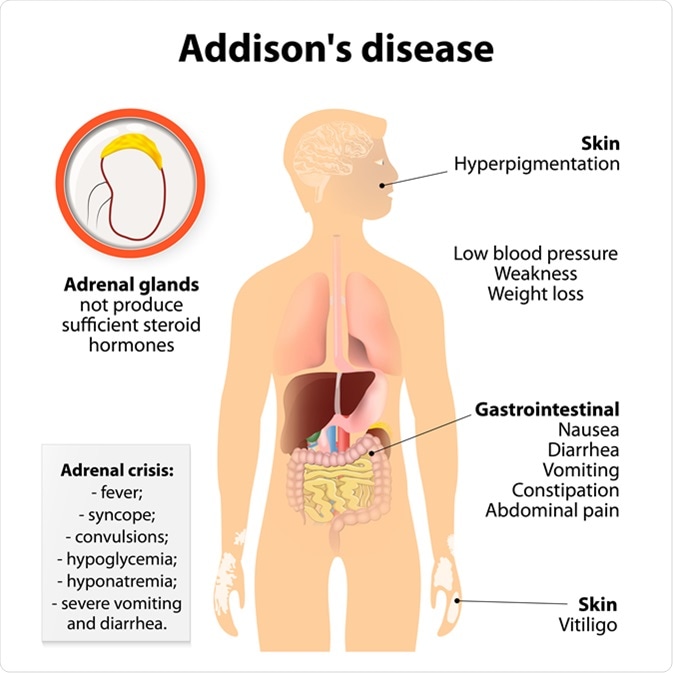
Addison’s disease, also known as primary adrenal insufficiency, is a rare but serious disorder of the adrenal glands. This disease occurs when the adrenal glands, which are located on top of the kidneys, do not produce enough of certain hormones, particularly cortisol and aldosterone. Cortisol is essential for regulating metabolism, stress response, and immune function, while aldosterone helps control blood pressure and fluid balance. When these hormones are insufficient, various bodily functions can be compromised, leading to a range of symptoms. Addison’s disease can have a significant impact on the patient’s quality of life and, if left untreated, can lead to life-threatening complications.
Causes of Addison’s Disease
Addison’s disease is primarily caused by the destruction or dysfunction of the adrenal glands. The most common cause of primary adrenal insufficiency is autoimmune adrenalitis, a condition where the body’s immune system mistakenly attacks and damages the adrenal cortex. Other causes include:
- Infections: Tuberculosis (TB) and other infections such as fungal infections, HIV, and cytomegalovirus can damage the adrenal glands, leading to Addison’s disease.
- Adrenal hemorrhage: Bleeding in the adrenal glands, often due to trauma or blood clotting disorders, can impair adrenal function.
- Genetic conditions: Rare genetic mutations can result in congenital adrenal hyperplasia or other inherited conditions that affect adrenal hormone production.
- Metastatic cancer: Tumors that spread from other parts of the body to the adrenal glands can lead to adrenal insufficiency.
- Surgical removal of adrenal glands: In some cases, surgery to remove one or both adrenal glands due to other conditions can result in Addison’s disease.
Signs and Symptoms
The symptoms of Addison’s disease can be vague and develop gradually, making it difficult to diagnose in its early stages. Common signs and symptoms include:
- Fatigue and weakness: One of the most common and debilitating symptoms, fatigue can be persistent and worsening over time.
- Weight loss and decreased appetite: Individuals may experience unexplained weight loss, coupled with a lack of appetite.
- Hyperpigmentation: The skin may darken, especially in areas of the body exposed to friction, such as the elbows, knees, and knuckles, due to increased levels of adrenocorticotropic hormone (ACTH).
- Low blood pressure: Hypotension, particularly when standing up, is common and may result in dizziness or fainting.
- Salt cravings: Due to low aldosterone levels, patients may develop an intense craving for salty foods, as aldosterone plays a role in maintaining sodium balance.
- Nausea, vomiting, and diarrhea: Gastrointestinal disturbances are common and may contribute to dehydration and electrolyte imbalances.
- Irritability and depression: As cortisol levels drop, patients may experience mood changes, including irritability, anxiety, and depression.
Etiology
The primary etiology of Addison’s disease is autoimmune adrenalitis, which accounts for approximately 70-90% of cases in developed countries. In autoimmune adrenalitis, the body’s immune system targets the adrenal glands, leading to their progressive destruction. This condition may also be associated with other autoimmune disorders, such as type 1 diabetes, autoimmune thyroid disease, and vitiligo.
Other etiologies include infectious causes, particularly tuberculosis, which is responsible for a significant number of cases of Addison’s disease, especially in areas with a high prevalence of TB. Adrenal hemorrhage can occur due to trauma, anticoagulant therapy, or infections such as meningococcal disease, which can result in the Waterhouse-Friderichsen syndrome, a severe form of adrenal gland destruction.
Pathophysiology
The pathophysiology of Addison’s disease revolves around the insufficient production of cortisol and aldosterone by the adrenal cortex. These hormones are essential for various physiological functions:
- Cortisol: As a glucocorticoid hormone, cortisol helps regulate the body’s response to stress, metabolism, immune function, and inflammation. In Addison’s disease, the adrenal glands fail to produce adequate amounts of cortisol, leading to impaired stress response, hypoglycemia, and increased susceptibility to infections.
- Aldosterone: Aldosterone is a mineralocorticoid hormone that helps maintain sodium and potassium balance, as well as regulate blood pressure. In Addison’s disease, aldosterone deficiency leads to salt and water imbalances, hypotension, and dehydration.
The failure of the adrenal glands to produce sufficient cortisol and aldosterone leads to the systemic effects observed in Addison’s disease. Additionally, the increased secretion of ACTH by the pituitary gland in response to low cortisol levels can result in hyperpigmentation of the skin.
DSM-5 Diagnosis
Addison’s disease is not specifically addressed in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5), as it is a physical endocrine disorder rather than a psychiatric condition. However, a diagnosis is typically made through clinical evaluation, laboratory tests, and imaging studies.
- Clinical evaluation: The physician assesses the patient’s medical history, symptoms, and risk factors (e.g., autoimmune disorders, infections, family history of endocrine diseases).
- Laboratory tests: The key diagnostic test for Addison’s disease is the measurement of plasma cortisol levels. A low cortisol level in the morning, along with elevated ACTH levels, is indicative of primary adrenal insufficiency. A ACTH stimulation test can further confirm the diagnosis. In this test, the adrenal glands’ response to synthetic ACTH is measured; a failure to raise cortisol levels suggests Addison’s disease.
- Imaging: A CT scan or MRI may be performed to examine the size and structure of the adrenal glands, particularly if a tumor or infection is suspected.
Treatment Regimens
The treatment of Addison’s disease focuses on replacing the deficient hormones and managing symptoms. Key components of treatment include:
- Glucocorticoid replacement: The mainstay of treatment is replacing cortisol with synthetic glucocorticoids, such as hydrocortisone, prednisone, or dexamethasone. These medications must be adjusted according to stress levels, such as during illness or surgery.
- Mineralocorticoid replacement: Fludrocortisone is commonly prescribed to replace aldosterone, which helps maintain blood pressure and electrolyte balance.
- Managing salt intake: Patients with Addison’s disease often need to increase their dietary salt intake, especially in hot weather or during periods of physical stress.
- Emergency care: During acute illness or stress, patients may need intravenous administration of fluids, electrolytes, and glucocorticoids. This is vital to prevent an adrenal crisis, a life-threatening condition that can occur when cortisol levels fall too low.
Patient Education
Patient education is an essential component of managing Addison’s disease, as it empowers patients to manage their condition and avoid potentially dangerous situations. Key areas of education include:
- Understanding the disease: Patients should be educated about the nature of Addison’s disease, its symptoms, and the importance of lifelong hormone replacement therapy.
- Stress management: Patients should be instructed on how to adjust their medication doses during periods of increased stress, such as illness, surgery, or injury.
- Recognizing an adrenal crisis: Patients must understand the signs of an adrenal crisis, which include severe fatigue, confusion, dizziness, vomiting, and low blood pressure. Immediate medical intervention is crucial to prevent serious complications.
- Adherence to treatment: Regular follow-up appointments to monitor hormone levels and adjust medication doses are critical for managing Addison’s disease effectively.
Conclusion
Addison’s disease is a chronic condition that requires careful management to avoid life-threatening complications. With appropriate treatment, including hormone replacement therapy, individuals with Addison’s disease can lead normal lives. However, due to the complexity of the disease and its varied symptoms, early diagnosis and patient education are crucial for effective management.
References
- Arlt, W., & Allolio, B. (2003). Adrenal insufficiency. The Lancet, 361(9372), 1881-1893. https://doi.org/10.1016/S0140-6736(03)13416-7
- Husebye, E. S., & Kämpe, O. (2018). Addison’s disease: Pathophysiology, diagnosis and treatment. Endocrine Reviews, 39(6), 742-768. https://doi.org/10.1210/er.2018-00060
- Betterle, C., & Lazzarotto, F. (2014). Autoimmune Addison’s disease: Clinical aspects. Autoimmunity Reviews, 13(1), 37-43. https://doi.org/10.1016/j.autrev.2013.08.002
- Mantero, F., & Arnaldi, G. (2017). Addison’s disease: Clinical features and diagnostic approach. The Lancet Diabetes & Endocrinology, 5(4), 246-257. https://doi.org/10.1016/S2213-8587(16)30216-2



