Nursing Paper Example on Barrett’s Esophagus
Nursing Paper Example on Barrett’s Esophagus
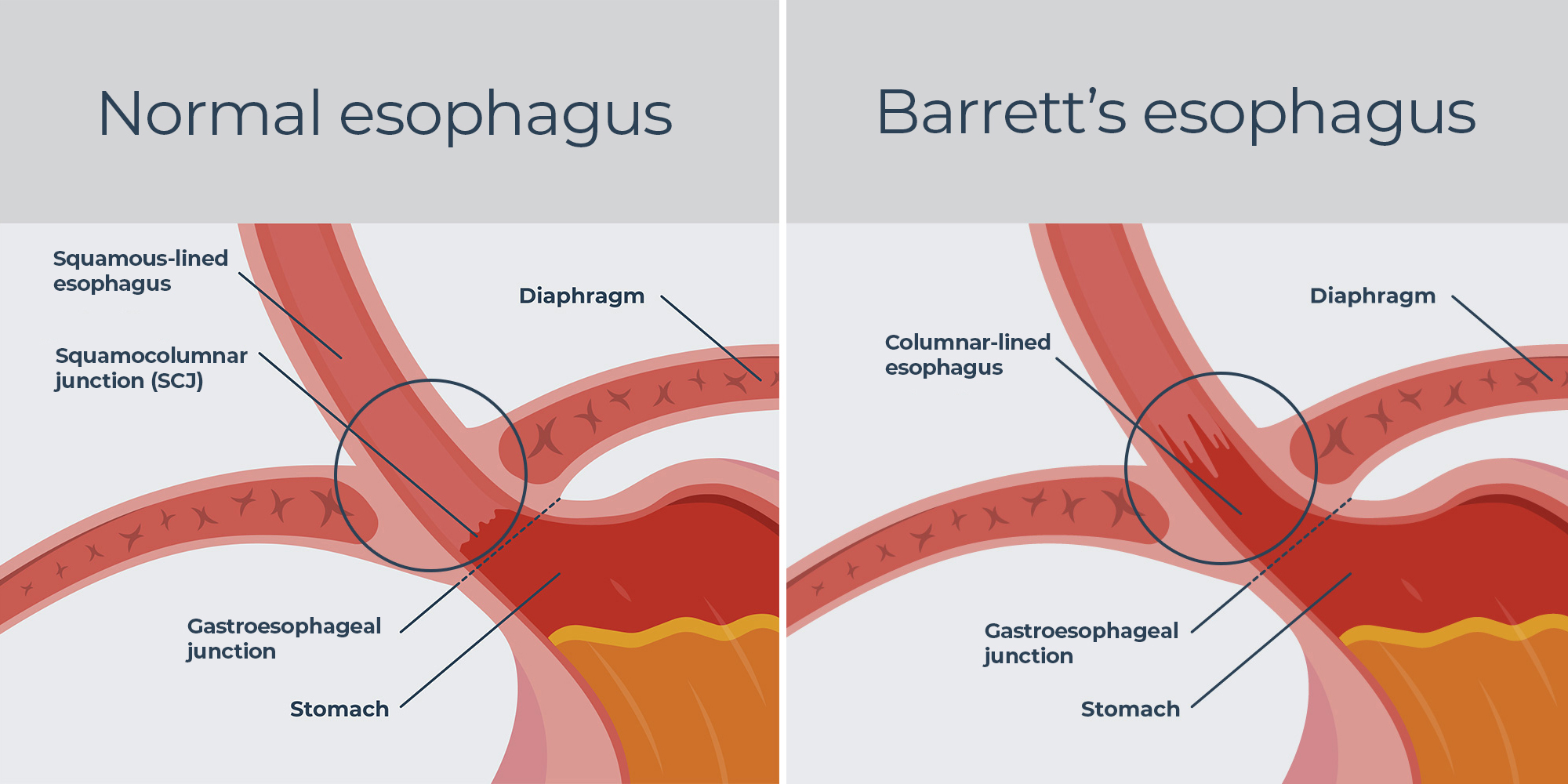
Barrett’s esophagus is a condition in which the normal squamous epithelium lining of the esophagus is replaced by specialized columnar epithelium, a process known as intestinal metaplasia. This change is considered a response to chronic gastroesophageal reflux disease (GERD) and increases the risk of developing esophageal adenocarcinoma, a potentially fatal cancer. It is most commonly diagnosed in individuals with longstanding GERD and is more prevalent in men than women. Early detection and management are critical to reducing the progression to esophageal cancer.
Causes of Barrett’s Esophagus
The primary cause of Barrett’s esophagus is chronic irritation of the esophageal lining due to acid reflux.
Gastroesophageal reflux disease (GERD): Persistent exposure of the esophageal lining to stomach acid leads to inflammation and cellular changes.
Lifestyle factors: Smoking, obesity, and excessive alcohol consumption exacerbate acid reflux, increasing the risk.
Hiatal hernia: This condition, which allows the stomach to push into the chest cavity, promotes acid reflux.
Genetics: Family history of GERD or esophageal cancer can predispose individuals to Barrett’s esophagus.
These risk factors highlight the complex interplay of environmental and genetic components in the disease.
Signs and Symptoms
Barrett’s esophagus itself is asymptomatic but often presents with symptoms of GERD.
Heartburn: A burning sensation in the chest or throat due to acid reflux.
Regurgitation: Acid or food may backflow into the throat or mouth.
Difficulty swallowing (dysphagia): Associated with inflammation or narrowing of the esophagus.
Chest pain: Non-cardiac chest pain may occur in some cases.
Silent reflux: Some patients experience no symptoms despite significant esophageal changes.
Persistent GERD symptoms warrant evaluation for Barrett’s esophagus, particularly in high-risk individuals.
Etiology
The etiology of Barrett’s esophagus revolves around chronic inflammation and cellular adaptation:
Prolonged acid exposure: Stomach acid and bile induce chronic esophagitis, promoting metaplastic changes.
Cellular response: Squamous epithelial cells transform into columnar cells with intestinal features to withstand acidic conditions.
Environmental triggers: Lifestyle factors such as poor diet, smoking, and obesity contribute to the disease’s onset and progression.
This transformation represents the body’s attempt to protect the esophagus, albeit at a cost.
Pathophysiology
Barrett’s esophagus progresses through distinct stages:
Metaplasia: Normal squamous epithelium is replaced by columnar epithelium with goblet cells.
Dysplasia: Low-grade dysplasia involves precancerous changes in the new epithelial cells. High-grade dysplasia features more significant cellular atypia, often preceding adenocarcinoma.
Esophageal adenocarcinoma: Dysplasia may advance to invasive cancer if untreated.
This progression underscores the importance of surveillance and early intervention in high-risk patients.
DSM-5 Diagnosis
Barrett’s esophagus is a medical condition and not addressed in the DSM-5. However, the psychological burden of living with a precancerous condition can contribute to anxiety or depression.
Diagnosis
Diagnosing Barrett’s esophagus requires a combination of clinical evaluation and diagnostic procedures.
Endoscopy: Visualization of the esophagus reveals abnormal reddish columnar lining replacing pale squamous epithelium.
Biopsy: Histological examination confirms the presence of intestinal metaplasia and assesses for dysplasia.
pH monitoring: Measures acid exposure in the esophagus to confirm GERD.
Imaging: Advanced imaging techniques like narrow-band imaging may enhance detection of dysplastic changes.
Regular surveillance endoscopy is recommended for patients with confirmed Barrett’s esophagus to detect progression.
Treatment Regimens
Treatment for Barrett’s esophagus focuses on controlling GERD, managing symptoms, and preventing progression to cancer.
- Lifestyle modifications: Weight loss, dietary changes, and avoiding tobacco or alcohol reduce acid reflux.
- Medications: Proton pump inhibitors (PPIs) are the mainstay treatment to suppress acid production. H2 receptor antagonists and antacids may provide additional relief.
- Endoscopic therapies:
Radiofrequency ablation (RFA): Heat energy removes dysplastic tissue.
Endoscopic mucosal resection (EMR): Dysplastic or early cancerous areas are removed.
- Surgical intervention:
Fundoplication: Surgical tightening of the lower esophageal sphincter prevents acid reflux.
Esophagectomy: Reserved for severe dysplasia or cancer.
These treatment modalities aim to reduce symptoms, reverse dysplasia, and minimize cancer risk.
Patient Education
Educating patients about Barrett’s esophagus and its implications is critical.
Diet and lifestyle: Advise a low-acid diet and avoidance of reflux-inducing foods.
Symptom monitoring: Encourage patients to report worsening symptoms or new swallowing difficulties.
Endoscopic surveillance: Explain the importance of regular endoscopies to monitor for dysplasia.
Medication adherence: Stress the need for consistent use of PPIs to control acid reflux.
Providing patients with knowledge and resources promotes proactive disease management.
Additional Considerations
Complications: Potential complications include esophageal ulcers, strictures, and progression to adenocarcinoma.
Epidemiology: Barrett’s esophagus affects approximately 1–2% of the population, with increased prevalence in older adults and males.
Prognosis: With regular monitoring and treatment, the risk of progression to cancer remains low in most patients.
Conclusion
Barrett’s esophagus is a condition with significant implications due to its association with esophageal adenocarcinoma. Early diagnosis, effective management of GERD, and diligent surveillance are key to mitigating risks and improving patient outcomes. Empowering patients through education and access to healthcare resources is equally vital for managing this chronic condition.
References
American College of Gastroenterology. (2021). Barrett’s esophagus: Guidelines for management. https://gi.org/guideline/barretts-esophagus/
Falk, G. W., & Sampliner, R. E. (2020). Barrett’s esophagus and risk of esophageal cancer. New England Journal of Medicine, 383(5), 469–481. https://doi.org/10.1056/NEJMra2005430
Katz, P. O., & Gerson, L. B. (2013). Barrett’s esophagus: Clinical implications and treatment. Journal of Clinical Gastroenterology, 47(9), 781–787. https://doi.org/10.1097/MCG.0b013e3182845b5b
Spechler, S. J., & Souza, R. F. (2014). Barrett’s esophagus. New England Journal of Medicine, 371(9), 836–845. https://doi.org/10.1056/NEJMra1314704



