Nursing Paper Example on Costochondritis
Nursing Paper Example on Costochondritis
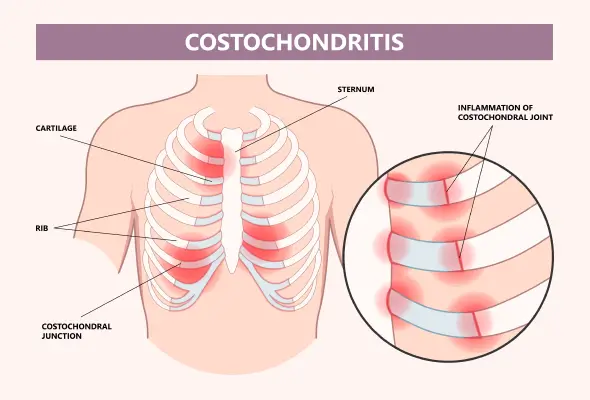
Costochondritis is a common musculoskeletal condition that involves inflammation of the costochondral, costosternal, or costovertebral joints. These are the points where the ribs attach to the sternum or spine. While it is not life-threatening, it can mimic more serious conditions, such as cardiac-related chest pain, leading to significant patient distress. Understanding its causes, clinical presentation, and management strategies is essential to ensure effective treatment and reassurance for affected individuals.
Causes of Costochondritis
Mechanical Stress
Repetitive physical activity, such as heavy lifting, coughing, or trauma, can strain the chest wall, leading to inflammation.
Infections
Though rare, viral or bacterial infections can affect the costochondral joints, especially after surgical procedures or thoracic trauma.
Arthritic Conditions
Underlying systemic inflammatory diseases such as rheumatoid arthritis, ankylosing spondylitis, or psoriatic arthritis may contribute to costochondral inflammation.
Idiopathic
In many cases, the exact cause remains unknown. These idiopathic cases are generally self-limiting and resolve without significant intervention.
Signs and Symptoms
Chest Pain
Sharp, stabbing, or aching pain localized to the costochondral or costosternal joints.
Pain often worsens with movement, deep breathing, or palpation of the affected joints.
Tenderness
Physical examination reveals tenderness at one or more costochondral junctions, typically in the second to fifth ribs.
Non-Radiating Pain
Unlike cardiac pain, costochondritis pain does not radiate to other areas such as the arms or jaw.
Absence of Systemic Symptoms
Fever, fatigue, and other systemic symptoms are generally absent, distinguishing costochondritis from infections or inflammatory diseases.
Etiology
Costochondritis is considered a benign condition, with several potential etiologies:
Trauma or Overuse: Often seen in athletes or individuals engaging in repetitive chest wall movements.
Infections: Rarely, organisms such as Staphylococcus aureus or Mycobacterium tuberculosis can affect the costochondral joints.
Post-Surgical Inflammation: Procedures involving the sternum, such as coronary artery bypass grafting, can predispose individuals to localized inflammation.
Pathophysiology
The pathophysiology of costochondritis involves localized inflammation of the cartilage that connects the ribs to the sternum.
Inflammatory Response
Mechanical stress or microtrauma triggers an inflammatory cascade, leading to swelling and increased sensitivity of nerve endings in the region.
Chronic Irritation
In recurrent cases, prolonged inflammation may result in fibrosis or cartilage degradation, contributing to persistent discomfort.
Diagnosis
Clinical Examination
Diagnosis is primarily clinical, based on history and physical findings such as tenderness over the costochondral junctions.
Pain reproduction upon palpation is a key diagnostic feature.
Exclusion of Cardiac Causes
Electrocardiogram and cardiac biomarkers may be necessary to rule out myocardial infarction or angina.
Imaging studies, such as chest X-rays, are often unremarkable but help exclude other causes of chest pain.
Advanced Imaging
MRI or ultrasound may be considered in atypical or refractory cases to assess soft tissue inflammation.
Bone scans can help differentiate costochondritis from conditions like Tietze syndrome, which involves visible swelling of the affected joints.
Treatment Regimens
Non-Pharmacological Treatments
Rest and Activity Modification: Avoid activities that exacerbate chest pain.
Heat or Cold Therapy: Alternating applications can reduce inflammation and pain.
Physical Therapy: Stretching and strengthening exercises improve posture and reduce chest wall strain.
Pharmacological Treatments
Nonsteroidal Anti-Inflammatory Drugs (NSAIDs): Ibuprofen or naproxen is commonly prescribed to reduce pain and inflammation.
Topical Analgesics: Lidocaine patches or diclofenac gel may provide localized relief.
Corticosteroid Injections: In refractory cases, local steroid injections can provide rapid symptom relief.
Surgical Interventions
Rarely required, surgery may be considered in chronic cases with persistent symptoms unresponsive to conservative treatments.
Patient Education
Understanding the Condition
Reassure patients that costochondritis is benign and self-limiting in most cases.
Emphasize that the condition is unrelated to cardiac or life-threatening causes of chest pain.
Self-Care Strategies
Encourage the use of proper ergonomics and body mechanics during activities to minimize strain.
Teach patients to recognize and avoid activities that trigger symptoms.
When to Seek Help
Advise patients to seek medical evaluation if chest pain is associated with symptoms such as shortness of breath, dizziness, or radiating pain, as these may indicate a cardiac origin.
Additional Considerations
Prognosis
The prognosis for costochondritis is excellent, with most cases resolving within weeks to months.
Chronic cases may require ongoing management to prevent recurrence.
Complications
While rare, untreated costochondritis may result in chronic pain or overlapping symptoms with other musculoskeletal disorders.
Differentiating from Tietze Syndrome
Unlike costochondritis, Tietze syndrome is characterized by visible swelling at the costochondral junctions. Proper differentiation is important for accurate management.
Conclusion
Costochondritis is a common, non-life-threatening condition that can cause significant discomfort and anxiety due to its similarity to cardiac chest pain. Early diagnosis, effective symptom management, and reassurance are key to improving patient outcomes. With appropriate care, most patients experience full resolution of symptoms and return to normal activities.
References
Clark, S., & Kruse, R. J. (2018). Costochondritis: Diagnosis and treatment. American Family Physician, 97(8), 485-490. https://www.aafp.org/pubs/afp/issues/2018/0415/p485.html
Gaitini, D., & Be’ery, I. (2019). Imaging of chest wall pain: Ultrasound as a first-line diagnostic tool. Clinical Radiology, 74(1), 11-20. https://www.clinicalradiologyonline.net/article/S0009-9260(18)30164-2/fulltext
Jansen, C. H., et al. (2020). Differentiation between costochondritis and Tietze syndrome: A clinical perspective. Pain Medicine, 21(5), 1010-1016. https://academic.oup.com/painmedicine/article/21/5/1010/5824253
Mayo Clinic. (2023). Costochondritis. https://www.mayoclinic.org/diseases-conditions/costochondritis/symptoms-causes/syc-20371175
Medscape. (2023). Costochondritis: Overview and treatment. https://emedicine.medscape.com/article/93326-overview



