Nursing Paper Example on Ecthyma
Nursing Paper Example on Ecthyma
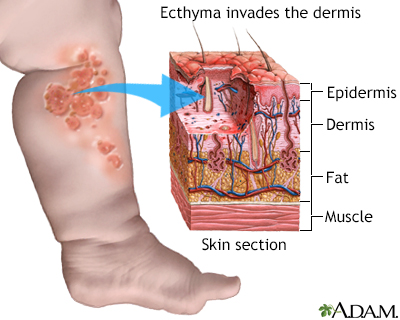
(Nursing Paper Example on Ecthyma) Ecthyma is a deeper skin infection characterized by ulcerative lesions that penetrate the epidermis and reach the dermis. Often regarded as a severe form of impetigo, ecthyma is most commonly caused by bacterial infections and typically affects individuals with poor hygiene or compromised immune systems. This paper provides a comprehensive overview of ecthyma, covering its causes, clinical presentation, pathophysiology, diagnostic criteria, treatment options, and preventive measures.
Causes of Ecthyma
Ecthyma is primarily caused by bacterial infections. The main causative agents are:
- Streptococcus pyogenes:
A beta-hemolytic bacterium often implicated in skin infections.
- Staphylococcus aureus:
Frequently associated with ecthyma, especially strains resistant to methicillin (MRSA).
- Secondary Factors:
Poor hygiene.
Trauma to the skin that provides entry points for bacteria.
Coexisting skin conditions such as eczema or insect bites.
Individuals with immune deficiencies, malnutrition, or systemic illnesses such as diabetes are at higher risk.
Signs and Symptoms of Ecthyma
Ecthyma lesions typically present as:
- Initial Lesions:
Small, erythematous, and pustular sores that progress into vesicles.
- Ulceration:
Vesicles rupture, forming round or oval ulcers with thick, adherent crusts.
Crusts are often yellowish-gray with erythematous, indurated margins.
- Pain and Tenderness:
Lesions may cause discomfort and are tender to the touch.
- Location:
Commonly affects the lower extremities but can appear on any part of the body.
If untreated, ecthyma may cause systemic symptoms, such as fever or lymphadenopathy, due to bacterial spread.
Pathophysiology of Ecthyma
Ecthyma begins with superficial bacterial colonization of damaged skin. If untreated, the infection spreads deeper into the dermis. Key factors include:
Host Immune Response: Inflammatory reactions to bacterial toxins result in tissue damage.
Enzymatic Breakdown: Bacterial enzymes, such as hyaluronidase, degrade dermal structures, facilitating deeper penetration.
Crust Formation: Exudates from necrotic tissues form the characteristic crust.
In severe or prolonged cases, secondary infections may develop, leading to cellulitis or systemic complications.
Diagnosis of Ecthyma
Diagnosing ecthyma involves a combination of clinical examination and laboratory investigations. Key diagnostic steps include:
Clinical Examination: Identification of ulcerative lesions with characteristic crusts.
Microbial Culture: Swabs from lesions help isolate causative bacteria and determine antibiotic sensitivity.
Histopathology: Rarely performed but may reveal dermal inflammation and necrosis.
Differential Diagnosis: Conditions such as impetigo, pyoderma gangrenosum, and cutaneous anthrax must be ruled out.
A thorough patient history, including hygiene practices and comorbidities, aids in diagnosis.
Treatment Regimens for Ecthyma
The primary goals of treatment are to eradicate the infection, promote healing, and prevent complications.
Topical Therapies
Antibacterial Ointments: Mupirocin or fusidic acid applied directly to lesions after cleaning.
Wound Care: Soaking the affected area with saline and debriding crusts promotes recovery.
Systemic Antibiotics
Indicated for extensive lesions or systemic symptoms.
First-Line Agents: Oral antibiotics such as penicillin or cephalexin targeting Streptococcus pyogenes.
MRSA Coverage: Clindamycin, doxycycline, or trimethoprim-sulfamethoxazole for suspected resistant strains.
Supportive Care
Maintaining hygiene and addressing underlying conditions such as diabetes or malnutrition is essential.
Complications of Ecthyma
If untreated, ecthyma can lead to severe complications, including:
Cellulitis: Bacterial spread into deeper tissues.
Post-Streptococcal Glomerulonephritis: Rare but serious immune-mediated kidney damage following Streptococcus pyogenes infections.
Scarring: Lesions may leave permanent scars due to dermal involvement.
Systemic Infections: Bacteremia and septicemia in immunocompromised individuals.
Prompt treatment minimizes the risk of these complications.
Prevention of Ecthyma
Preventive measures focus on reducing bacterial colonization and maintaining skin integrity. These include:
Personal Hygiene: Regular bathing and appropriate wound care.
Injury Management: Immediate cleaning and dressing of cuts or abrasions.
Addressing Underlying Conditions: Managing systemic illnesses like diabetes.
Prophylactic Measures: In high-risk groups, antibacterial soaps or preventive antibiotics may be recommended.
Education on hygiene practices is critical, especially in communities with limited resources.
Prognosis
With timely and appropriate treatment, ecthyma generally resolves without long-term consequences. However, severe or neglected cases may result in scarring or systemic complications.
Patient Education
Patients should be educated about:
Recognizing early signs of ecthyma to seek prompt treatment.
Maintaining hygiene and avoiding practices that damage the skin, such as excessive scratching.
Adhering to prescribed treatments and follow-ups to ensure complete resolution of the infection.
Support from healthcare providers, including detailed explanations and demonstrations of wound care, fosters adherence and better outcomes.
Conclusion
Ecthyma is a significant skin infection that can cause considerable discomfort and complications if untreated. Early diagnosis, targeted antibiotic therapy, and proper wound care are crucial for successful management. Preventive measures and patient education play vital roles in reducing the incidence of ecthyma, particularly in vulnerable populations.
References
American Academy of Dermatology Association. (2023). Ecthyma: Causes, symptoms, and treatments.
https://www.aad.org
Centers for Disease Control and Prevention (CDC). (2023). Group A Streptococcal (GAS) diseases.
https://www.cdc.gov
National Library of Medicine. (2023). Ecthyma: A bacterial skin infection.
https://www.ncbi.nlm.nih.gov
Mayo Clinic. (2023). Ecthyma: Diagnosis and management.
https://www.mayoclinic.org



