Nursing Paper Example on Teratoma
Nursing Paper Example on Teratoma
Teratomas are complex tumors derived from germ cells that can contain various types of tissue, such as hair, muscle, and even bone. These tumors often form in the ovaries, testicles, or sacrococcygeal area (base of the spine) but can also appear in other areas of the body. Teratomas are known for their unique ability to develop tissues from multiple germ layers—ectoderm, mesoderm, and endoderm—leading to a wide range of cellular components. They are most frequently observed in children and young adults and can range from benign (non-cancerous) to malignant (cancerous) forms.
Types of Teratomas
Mature Teratomas
Mature teratomas are typically benign and well-differentiated, meaning they contain fully formed tissue, such as hair or teeth, but do not exhibit aggressive or cancerous behavior. These are the most common form of teratoma in females and are often found in the ovaries.
Immature Teratomas
Immature teratomas are less common but more dangerous, as they contain immature, embryonic-like tissue. This type of teratoma has a higher potential for malignancy and may spread to other parts of the body. They are often diagnosed in children and young adults and require closer monitoring and sometimes more aggressive treatment.
Monodermal or Specialized Teratomas
Monodermal teratomas are rare forms of teratoma that contain predominantly one type of tissue. A common example is struma ovarii, where the tumor primarily consists of thyroid tissue.
Causes and Risk Factors
The exact cause of teratomas remains unknown, but they arise from germ cells, which are capable of differentiating into any cell type in the body. Teratomas are thought to develop due to errors during the migration and division of these germ cells. Key factors include:
- Germ Cell Origin: Germ cells, which normally develop into reproductive cells, sometimes migrate incorrectly during fetal development and can form tumors in atypical locations.
- Genetic Factors: Studies suggest that certain genetic mutations or predispositions may contribute to the formation of teratomas, particularly malignant variants (National Institutes of Health [NIH], 2022).
- Hormonal Influence: Some research indicates that hormonal changes, particularly during puberty, may stimulate teratoma growth (American Cancer Society [ACS], 2023).
Pathophysiology
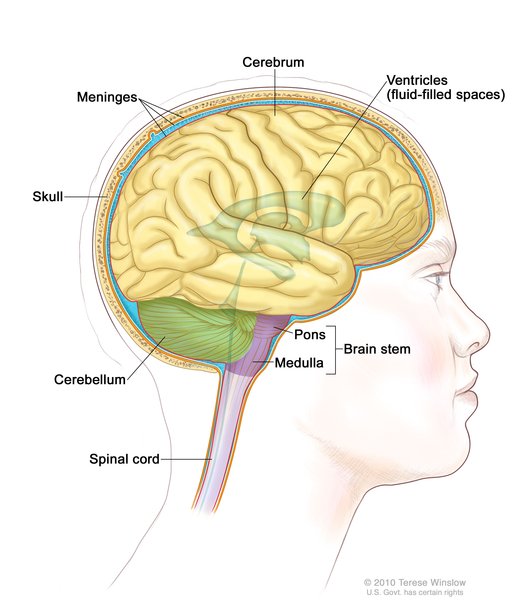
Teratomas arise from pluripotent germ cells that are unique because of their ability to differentiate into multiple cell types. This pluripotency explains why teratomas often contain tissue from multiple germ layers, such as skin, neural tissue, or muscle. These tumors are most common in the gonadal regions, where germ cells are concentrated. In certain cases, particularly with immature teratomas, embryonic-like cells predominate, leading to a higher risk of malignancy. The likelihood of malignancy generally depends on the degree of cellular differentiation and the presence of immature tissues (ACS, 2023).
Signs and Symptoms
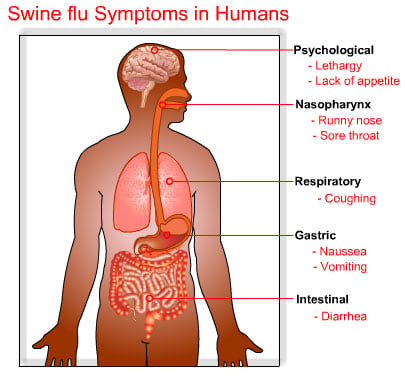
The symptoms of teratomas vary depending on their location, size, and type. Common symptoms include:
- Abdominal or Pelvic Pain: Teratomas in the ovaries or testicles may cause pain or discomfort in the abdomen or pelvis.
- Visible or Palpable Mass: Patients may notice or feel a lump, especially if the teratoma is located superficially.
- Complications from Compression: Larger teratomas can compress nearby organs, leading to digestive or urinary symptoms.
- Increased Thyroid Activity: In cases of struma ovarii, thyroid tissue in the teratoma may produce hormones, causing symptoms of hyperthyroidism (NIH, 2022).
Diagnosis
Imaging Techniques
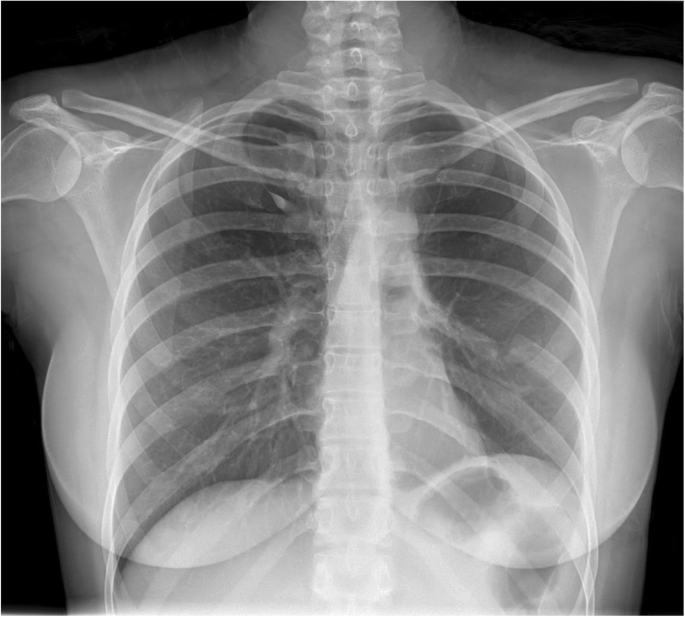
Ultrasound is often the initial imaging technique for detecting ovarian or testicular teratomas, providing insight into the composition of the mass. Computed Tomography (CT) or Magnetic Resonance Imaging (MRI) scans can help visualize the tumor’s size, location, and tissue composition. These scans help differentiate teratomas from other types of tumors.
(Nursing Paper Example on Teratoma)
Biopsy and Histopathology
Biopsies are generally avoided due to the risk of spreading cells, but surgical removal of the tumor followed by histopathological analysis is the standard. Microscopic examination can confirm the presence of different tissue types and establish whether the tumor is mature or immature, thus determining its potential malignancy (Mayo Clinic, 2022).
Treatment Regimens
Surgical Removal
Surgery is the primary treatment for teratomas. For benign, mature teratomas, a straightforward surgical excision often leads to a full recovery. In ovarian cases, minimally invasive techniques like laparoscopy are frequently used to remove the tumor.
Chemotherapy and Radiation
In cases of malignant or metastatic teratomas, chemotherapy or radiation may be required. Chemotherapy is especially useful in immature teratomas with malignant potential, as it targets rapidly dividing cells. Common chemotherapy drugs include cisplatin and bleomycin, especially in testicular teratomas, which respond well to these agents.
Hormonal Therapy
Hormonal therapy may be considered in cases of hormone-producing teratomas, such as those that contain thyroid tissue (struma ovarii). This approach is rare and tailored based on the tumor’s effects on the patient’s hormone levels (NIH, 2022).
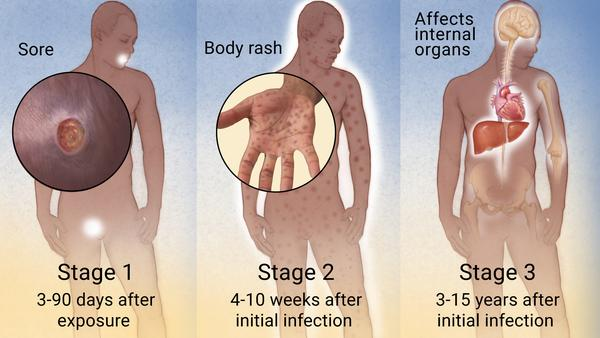
Complications
Complications can arise due to the tumor’s size, location, or malignancy potential. Key complications include:
- Rupture and Infection: Large ovarian teratomas can rupture, leading to inflammation and infection in the surrounding tissues.
- Metastasis: Immature teratomas, especially in the testicles, have the potential to metastasize, spreading malignant cells to other parts of the body.
- Paraneoplastic Syndromes: Some teratomas can cause paraneoplastic syndromes, where the tumor produces substances leading to symptoms unrelated to its size or location, such as hormone imbalances.
Prevention
Since the exact causes of teratomas are not fully understood, specific preventive measures are not established. However, early detection can improve outcomes, particularly in the case of immature teratomas with malignant potential. Regular medical check-ups and imaging, especially for individuals with family histories of germ cell tumors, may help detect teratomas early.
(Nursing Paper Example on Teratoma)
Prognosis
The prognosis for teratoma patients depends on several factors, including tumor type (mature vs. immature), location, and malignancy. Mature teratomas are typically benign with an excellent prognosis following surgical removal. In contrast, immature teratomas, particularly those with malignant cells, may have a variable prognosis, depending on the stage at diagnosis and the effectiveness of treatment. Early intervention and appropriate therapy lead to a high cure rate in localized cases (ACS, 2023).
Conclusion
Teratomas are fascinating but complex tumors, known for their unique tissue composition. They range from benign forms with an excellent prognosis to malignant cases requiring aggressive treatment. Early diagnosis and treatment are essential to minimize complications, especially in malignant teratomas. Further research into the genetic and molecular basis of teratomas may provide insights into potential preventive and therapeutic approaches, offering hope for those affected by these tumors.
References
American Cancer Society (ACS). (2023). Types of teratomas and their treatment. https://www.cancer.org/teratomas
Mayo Clinic. (2022). Teratoma diagnosis and treatment. https://www.mayoclinic.org/teratoma