Nursing Paper Example on Tonsillitis
Nursing Paper Example on Tonsillitis
Tonsillitis is an inflammation of the tonsils, two oval-shaped lymphoid tissues located at the back of the throat. This condition is common, particularly in children, but can affect individuals of all ages. Tonsillitis is generally caused by viral or bacterial infections, leading to painful swelling, difficulty swallowing, and other symptoms. While tonsillitis is usually self-limiting, it can sometimes lead to complications if left untreated.

Causes and Risk Factors
Tonsillitis can be caused by several types of pathogens, with varying risk factors associated with the condition.
- Viral Infections: Viral infections are the most common cause of tonsillitis. Viruses such as adenovirus, rhinovirus, influenza, and the Epstein-Barr virus can lead to tonsil inflammation. Viruses are responsible for up to 70% of tonsillitis cases in children (Centers for Disease Control and Prevention [CDC], 2023).
- Bacterial Infections: Streptococcus pyogenes, the bacterium responsible for strep throat, is the most common bacterial cause of tonsillitis. This bacterial form is often more severe than viral tonsillitis and requires antibiotic treatment to prevent complications (Mayo Clinic, 2023).
- Environmental and Lifestyle Factors: Tonsillitis can be aggravated by exposure to pollutants, such as smoke, which can irritate the throat and weaken immune response. Additionally, close contact with infected individuals in crowded environments increases transmission risk, especially in schools and daycare centers.
- Weakened Immune System: A weakened immune system, due to conditions like diabetes or immunodeficiency, increases susceptibility to tonsillitis by limiting the body’s ability to fight infections effectively.
Signs and Symptoms
Tonsillitis symptoms can range from mild to severe and may vary depending on the type of infection and the patient’s immune response. Common symptoms include:
- Sore Throat: A persistent sore throat is often the first symptom, accompanied by redness and swelling of the tonsils.
- Swollen Tonsils: The tonsils may appear red and swollen, sometimes with white or yellow patches if the infection is bacterial.
- Painful Swallowing: Inflammation of the tonsils makes swallowing painful and difficult, which may lead to reduced food and fluid intake.
- Fever and Chills: Fever often accompanies tonsillitis, particularly in bacterial cases, with temperatures potentially reaching high levels.
- Enlarged Lymph Nodes: Swelling in the lymph nodes around the neck area is also a common symptom of tonsillitis.
- Other Symptoms: These can include headache, fatigue, hoarseness, and in some cases, ear pain due to referred pain from the throat.
Pathophysiology
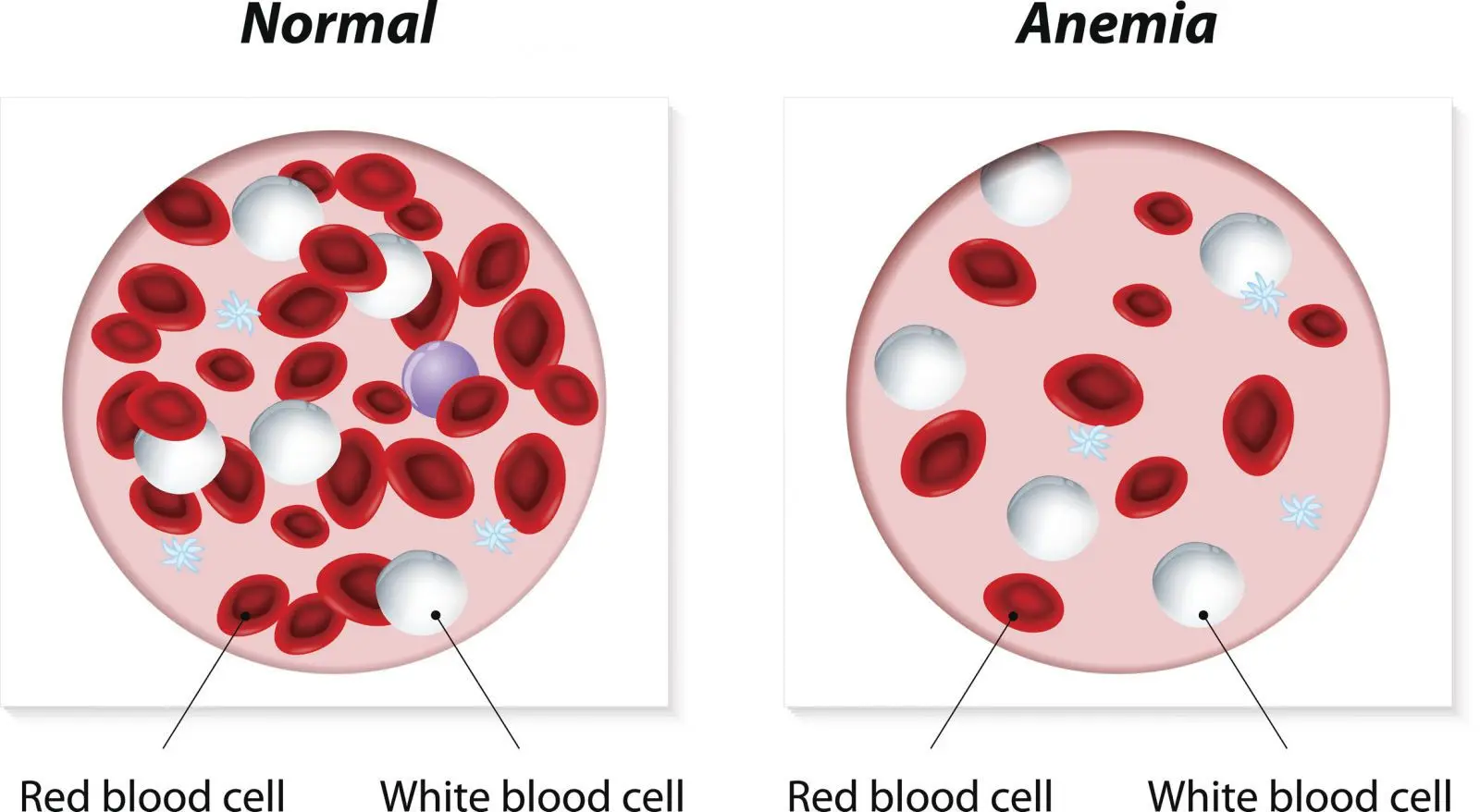
The tonsils play a critical role in immune defense by capturing pathogens entering the body through the mouth or nose. When a pathogen infects the tonsils, the immune system activates and produces white blood cells to fight off the infection. In the case of tonsillitis, this immune response causes inflammation and pain in the tonsils. Viral tonsillitis tends to be self-limiting, with the immune system clearing the infection within a few days. Bacterial tonsillitis, particularly due to Streptococcus pyogenes, requires antibiotic treatment to reduce inflammation and prevent further complications.
Types
Tonsillitis can be categorized based on the frequency and duration of episodes:
- Acute Tonsillitis: This is a short-term inflammation, lasting up to 10 days, and is most commonly due to viral infections. Symptoms generally resolve with or without medical intervention.
- Recurrent Tonsillitis: Individuals experiencing multiple episodes of tonsillitis within a year are classified as having recurrent tonsillitis. This often requires careful monitoring and, in some cases, surgical intervention.
- Chronic Tonsillitis: Chronic tonsillitis is marked by persistent sore throat, bad breath, and tonsil stones, and it may last for weeks. Chronic tonsillitis often results in surgical removal of the tonsils (tonsillectomy).
(Nursing Paper Example on Tonsillitis)
Diagnosis
Diagnosis typically involves a physical examination and may include additional tests to identify the cause of infection.
- Physical Examination: A healthcare provider examines the throat and neck to check for swollen tonsils, white patches, or enlarged lymph nodes.
- Throat Swab Test: A throat swab can help determine if Streptococcus pyogenes or other bacteria are present, which is particularly useful in differentiating bacterial from viral tonsillitis.
- Complete Blood Count (CBC): In some cases, a blood test may be performed to identify any unusual white blood cell counts, which may help in distinguishing between viral and bacterial infections.
Treatment and Management
Treatment for tonsillitis varies based on whether the infection is viral or bacterial, as well as the severity and frequency of episodes.
- Viral Tonsillitis: Viral tonsillitis usually resolves on its own within 7-10 days. Symptomatic treatments include rest, hydration, over-the-counter pain relievers like acetaminophen or ibuprofen, and throat lozenges for comfort.
- Bacterial Tonsillitis: If bacterial tonsillitis is confirmed, antibiotics, most commonly penicillin or amoxicillin, are prescribed to prevent complications such as rheumatic fever (NICE, 2023). Patients are encouraged to complete the entire antibiotic course, even if symptoms improve, to ensure full recovery.
- Surgical Management: In recurrent or chronic cases where tonsillitis significantly impacts quality of life, a tonsillectomy may be recommended. Tonsillectomy has shown to reduce the recurrence of infection and alleviate chronic symptoms (American Academy of Otolaryngology-Head and Neck Surgery, 2022).
(Nursing Paper Example on Tonsillitis)
Complications
Complications from untreated or severe tonsillitis can lead to additional health issues:
- Peritonsillar Abscess: Also known as quinsy, this is an accumulation of pus behind the tonsils, which can cause severe pain, difficulty swallowing, and even breathing problems.
- Obstructive Sleep Apnea: Enlarged tonsils can obstruct the airway during sleep, leading to sleep apnea, particularly in children.
- Rheumatic Fever: If streptococcal tonsillitis is left untreated, it may lead to rheumatic fever, which can affect the heart, joints, and nervous system.
- Glomerulonephritis: A rare complication where the kidneys become inflamed, potentially leading to kidney damage.
Prevention
Prevention methods focus on reducing exposure to infectious agents and maintaining a strong immune system:
- Good Hygiene Practices: Regular handwashing, avoiding close contact with infected individuals, and not sharing eating utensils can reduce the risk of contracting tonsillitis.
- Strengthening the Immune System: A healthy diet, regular exercise, and sufficient sleep can improve immune response and decrease the likelihood of infections.
- Vaccination: Annual flu vaccinations and timely immunizations, such as the diphtheria vaccine, help protect against some pathogens that may lead to tonsillitis.
Conclusion
Tonsillitis is a common yet potentially painful condition affecting individuals across all age groups. While it is often self-limiting, bacterial tonsillitis requires appropriate antibiotic treatment to prevent complications. Effective prevention, early diagnosis, and timely intervention can reduce the severity and frequency of episodes. In cases of chronic or recurrent tonsillitis, surgical options provide relief and improve the quality of life.
References
American Academy of Otolaryngology-Head and Neck Surgery. (2022). Tonsillectomy and adenoidectomy. https://www.entnet.org
Centers for Disease Control and Prevention. (2023). Tonsillitis and pharyngitis. https://www.cdc.gov
Mayo Clinic. (2023). Tonsillitis: Symptoms and causes. https://www.mayoclinic.org