Nursing Paper Example on Leprosy [SOLVED]
/in Assignment Help, Assignment Help Nursing, Homework Help, Nursing Exam Help, Nursing Paper Help, Psychology assignment help, Solved Nursing Essays /by Aimee GraceNursing Paper Example on Leprosy [SOLVED]
Leprosy, also known as Hansen’s disease, has perplexed humanity for centuries, shrouded in stigma and fear. Despite significant advancements in medical science, leprosy remains a challenge in many parts of the world. This paper delves into the causes, symptoms, etiology, pathophysiology, DSM-5 diagnosis, treatment regimens, and patient education regarding leprosy. Leprosy, caused by Mycobacterium leprae, presents a spectrum of clinical manifestations, ranging from mild to severe, with pathognomonic signs such as hypopigmented skin patches and nerve thickening. Etiologically, genetic predisposition and environmental factors play significant roles, contributing to disease prevalence in endemic regions. Understanding the complex pathophysiology, immune evasion mechanisms, and host responses elucidates the disease’s intricate nature. Despite the absence of specific DSM-5 diagnostic criteria, clinical and laboratory assessments guide diagnosis and classification. Multi-drug therapy (MDT) stands as the gold standard treatment, emphasizing early diagnosis, adherence, and patient education to combat the disease’s social stigma and prevent transmission. (Nursing Paper Example on Leprosy [SOLVED])
Causes
Leprosy, caused by Mycobacterium leprae, has puzzled humanity for centuries, prevailing as a significant global health concern. The bacterium’s slow growth and unique cell wall composition contribute to its elusive nature, evading the host immune response and establishing chronic infection.
Transmission primarily occurs through respiratory droplets, often via prolonged close contact with untreated individuals. However, the exact mechanisms of transmission remain incompletely understood, with factors such as genetic susceptibility and environmental conditions playing pivotal roles.
Genetic predisposition significantly influences leprosy susceptibility, with certain populations exhibiting heightened vulnerability. Variations in immune response genes, such as those encoding human leukocyte antigens (HLAs), influence an individual’s ability to mount an effective immune response against M. leprae.
Environmental factors also contribute to disease prevalence, particularly in endemic regions characterized by poor living conditions and inadequate healthcare access. Socioeconomic disparities, overcrowding, and substandard sanitation facilitate disease transmission and hinder timely diagnosis and treatment.
Furthermore, socioeconomic factors intersect with cultural beliefs and stigma, exacerbating the burden of leprosy. Misconceptions surrounding the disease perpetuate social ostracism, discrimination, and delayed healthcare-seeking behavior, impeding effective disease management and control efforts.
In endemic areas, socio-cultural practices, such as religious and traditional beliefs, may influence disease transmission dynamics and healthcare-seeking behavior. Addressing these socio-cultural determinants is crucial for implementing culturally sensitive and effective leprosy control programs.
In summary, the causes of leprosy are multifaceted, encompassing both microbial and host factors, as well as social determinants. Comprehensive approaches addressing genetic susceptibility, environmental conditions, and socio-cultural factors are imperative for combating leprosy’s persistent burden and achieving global elimination goals. (Nursing Paper Example on Leprosy [SOLVED])
Signs and Symptoms
Leprosy manifests with a spectrum of clinical manifestations, varying in severity and presentation. The disease typically affects the skin, peripheral nerves, and mucous membranes, giving rise to diverse signs and symptoms.
One of the hallmark signs of leprosy is the appearance of hypopigmented or erythematous skin patches, often with altered sensation or numbness. These skin lesions may be solitary or multiple, with variable distribution across the body.
Peripheral nerve involvement is characteristic of leprosy, leading to sensory and motor deficits. Thickened and tender nerves, known as nerve enlargement or neuritis, are pathognomonic of leprosy and commonly affect peripheral nerves, such as the ulnar, radial, and common peroneal nerves.
Sensory impairment is a common feature of leprosy, ranging from hypoesthesia (reduced sensation) to anesthesia (loss of sensation) in affected areas. Patients may experience numbness, tingling, or burning sensations, particularly in the hands, feet, and face.
Motor impairment may occur secondary to nerve damage, leading to muscle weakness, atrophy, and deformities. Clawing of the hands and feet, as well as foot drop, are common motor deficits observed in leprosy patients.
In advanced cases, leprosy can cause debilitating complications, such as trophic ulcers, joint deformities, and eye involvement. Ocular manifestations, including lagophthalmos (incomplete closure of the eyelids) and blindness, may result from corneal anesthesia and subsequent exposure keratitis.
Overall, recognizing the diverse signs and symptoms of leprosy is crucial for early diagnosis and prompt initiation of treatment. Timely intervention can prevent disease progression, reduce disability, and mitigate the social stigma associated with leprosy, improving patients’ quality of life. (Nursing Paper Example on Leprosy [SOLVED])
Etiology
The etiology of leprosy is complex and multifactorial, involving interactions between microbial, host genetic, and environmental factors. Mycobacterium leprae, the causative agent of leprosy, is a slow-growing, acid-fast bacterium that primarily infects the skin and peripheral nerves.
Genetic predisposition plays a significant role in leprosy susceptibility, with certain individuals exhibiting increased vulnerability to infection. Variations in immune response genes, particularly those encoding human leukocyte antigens (HLAs), influence an individual’s ability to mount an effective immune response against M. leprae.
Studies have identified specific HLA alleles associated with susceptibility or resistance to leprosy, highlighting the importance of host genetic factors in disease pathogenesis. Additionally, polymorphisms in genes involved in innate and adaptive immunity, such as toll-like receptors and cytokines, contribute to interindividual variability in leprosy susceptibility and clinical outcomes.
Environmental factors also contribute to leprosy transmission and disease prevalence, particularly in endemic regions characterized by poor living conditions and inadequate healthcare access. Socioeconomic disparities, overcrowding, and substandard sanitation facilitate disease transmission and hinder timely diagnosis and treatment.
The geographical distribution of leprosy reflects the complex interplay between environmental factors and genetic susceptibility, with endemic regions clustered in areas with high population density, tropical climates, and socio-economic challenges. Furthermore, environmental changes, such as urbanization and migration, may influence leprosy epidemiology by altering disease transmission dynamics and access to healthcare services.
Understanding the multifaceted etiology of leprosy is essential for designing effective control strategies and targeted interventions aimed at reducing disease burden and transmission. Integrating genetic, environmental, and socio-economic approaches can help address the complex challenges posed by leprosy and pave the way towards its elimination. (Nursing Paper Example on Leprosy [SOLVED])
Pathophysiology
The pathophysiology of leprosy involves complex interactions between Mycobacterium leprae, the host immune response, and the peripheral nervous system. Upon entry into the body, M. leprae targets skin macrophages and Schwann cells, initiating a cascade of immune responses and tissue damage.
The unique cell wall composition of M. leprae enables it to evade the host immune system, facilitating chronic infection and disease progression. The bacterium’s slow growth rate further complicates immune clearance, allowing it to establish persistent infection within the host.
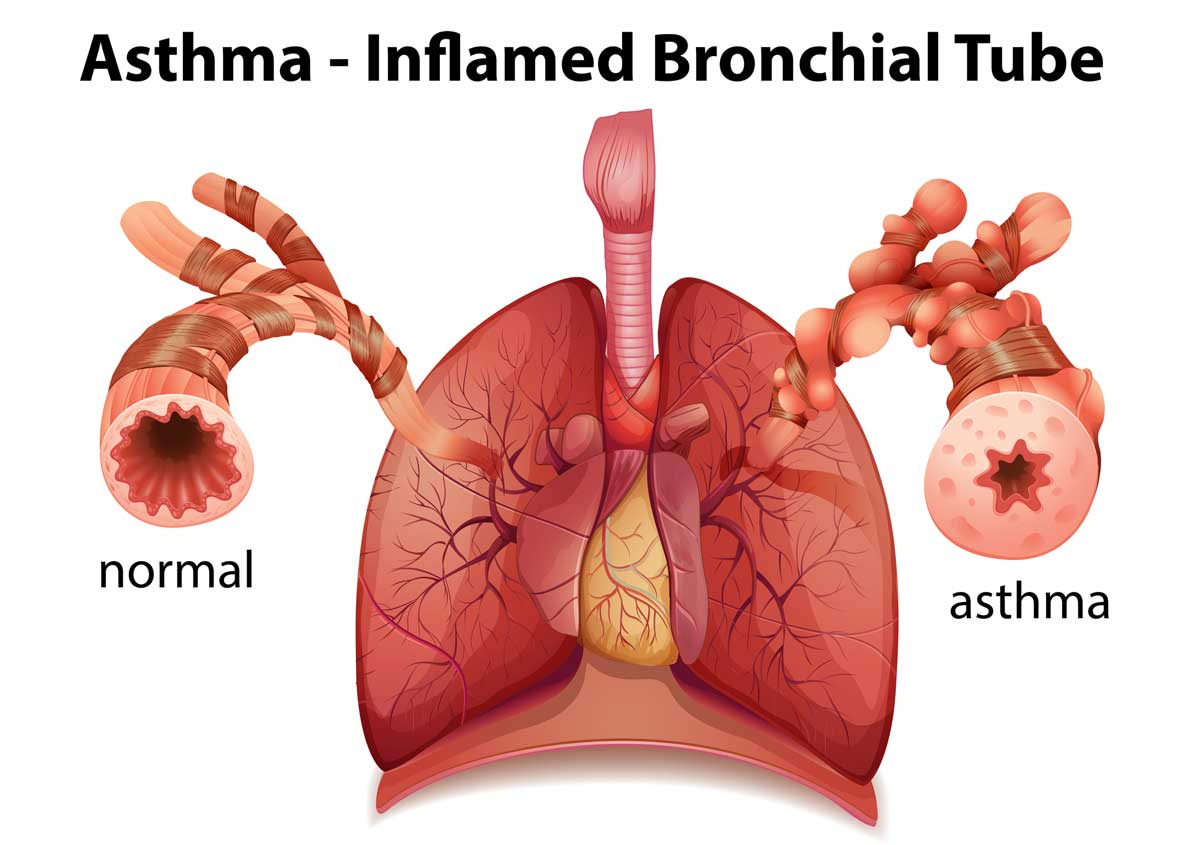
In the skin, M. leprae replicates within macrophages and infiltrates Schwann cells, leading to the formation of granulomas and nerve damage. Nerve involvement is a hallmark feature of leprosy, contributing to the diverse clinical manifestations observed in affected individuals.
As the infection progresses, immune-mediated inflammation exacerbates tissue damage, resulting in the characteristic skin lesions, nerve thickening, and sensory deficits associated with leprosy. The release of pro-inflammatory cytokines and chemokines further amplifies the immune response, perpetuating tissue destruction and nerve dysfunction.
Peripheral nerve damage in leprosy occurs through multiple mechanisms, including direct bacterial invasion, immune-mediated inflammation, and ischemic injury. Schwann cell damage and demyelination disrupt nerve conduction, leading to sensory and motor deficits characteristic of leprosy neuropathy.
In addition to peripheral nerve involvement, leprosy can affect other organ systems, including the eyes, mucous membranes, and bones. Ocular complications, such as lagophthalmos and blindness, may result from corneal anesthesia and exposure keratitis.
Overall, the pathophysiology of leprosy is characterized by a complex interplay between microbial virulence factors, host immune responses, and tissue damage mechanisms. Understanding these processes is essential for elucidating disease pathogenesis and developing targeted therapeutic interventions to mitigate the clinical manifestations of leprosy. (Nursing Paper Example on Leprosy [SOLVED])
DSM-5 Diagnosis
While the DSM-5 primarily focuses on psychiatric disorders, clinicians utilize clinical and laboratory findings to diagnose and classify leprosy according to standardized criteria. The DSM-5 does not provide specific diagnostic criteria for leprosy; however, clinical assessment and laboratory tests guide diagnosis and classification.
Clinical evaluation of suspected leprosy cases involves a comprehensive history and physical examination, focusing on skin lesions, nerve involvement, and systemic symptoms. Characteristic findings, such as hypopigmented or erythematous skin patches with sensory loss and nerve thickening, raise suspicion for leprosy.
Laboratory tests play a crucial role in confirming the diagnosis of leprosy and assessing disease severity. Skin biopsy, performed from an active skin lesion or thickened nerve, allows histopathological examination and acid-fast bacilli (AFB) staining to detect M. leprae.
Nerve involvement assessment, including sensory and motor testing, aids in determining disease extent and classification. Nerve conduction studies and electromyography may reveal abnormalities indicative of leprosy neuropathy, such as sensory loss and muscle weakness.
Leprosy classification follows the Ridley-Jopling system, which categorizes the disease into five subtypes based on clinical and histopathological criteria. These subtypes range from indeterminate and tuberculoid leprosy, characterized by limited skin lesions and strong cell-mediated immunity, to lepromatous leprosy, marked by widespread skin involvement and impaired cellular immunity.
DSM-5 diagnosis of leprosy encompasses a multidisciplinary approach, integrating clinical assessment, laboratory tests, and histopathological findings to establish the diagnosis and classify the disease subtype. Timely diagnosis enables prompt initiation of treatment, reducing disease transmission and preventing complications associated with leprosy neuropathy. (Nursing Paper Example on Leprosy [SOLVED])
Treatment Regimens and Patient Education
Multi-drug therapy (MDT) stands as the cornerstone of leprosy treatment, aiming to eliminate M. leprae and prevent disease progression and transmission. The World Health Organization (WHO) recommends standard MDT regimens, consisting of rifampicin, dapsone, and clofazimine, tailored to the disease subtype and severity.
Early diagnosis and prompt initiation of treatment are essential to prevent irreversible nerve damage and disability associated with leprosy. Treatment regimens vary depending on disease classification, with paucibacillary (PB) and multibacillary (MB) forms requiring different durations of therapy.
Paucibacillary leprosy, characterized by a limited number of skin lesions and low bacterial load, typically requires six months of rifampicin and dapsone combination therapy. Multibacillary leprosy, presenting with numerous skin lesions and higher bacterial burden, necessitates twelve months of rifampicin, dapsone, and clofazimine combination therapy.
In addition to pharmacological treatment, comprehensive management of leprosy includes wound care, rehabilitation, and social support services. Physiotherapy and occupational therapy may help mitigate disability and improve functional outcomes in patients with leprosy neuropathy and deformities.
Patient education plays a crucial role in leprosy treatment adherence and stigma reduction, empowering individuals to actively participate in their care. Education initiatives focus on dispelling myths and misconceptions surrounding leprosy, promoting early healthcare-seeking behavior, and addressing social stigma and discrimination.
Patients receive information on the importance of completing the prescribed treatment regimen, emphasizing the role of medication adherence in achieving cure and preventing relapse. Healthcare providers educate patients on potential side effects of MDT, encouraging early reporting and management of adverse reactions to optimize treatment outcomes.
Furthermore, patient education programs emphasize self-care practices, including skin hygiene, wound care, and protective measures to prevent secondary infections and injury. Patients learn to recognize signs of nerve damage and disability, empowering them to seek timely medical attention and access rehabilitation services.
Community-based education initiatives engage local leaders, schools, and religious institutions to raise awareness about leprosy and promote inclusive attitudes towards affected individuals. By fostering supportive environments and advocating for social inclusion, patient education efforts contribute to reducing the burden of leprosy and improving the quality of life for affected individuals. (Nursing Paper Example on Leprosy [SOLVED])
Conclusion
Leprosy remains a challenging global health issue, characterized by complex interactions between microbial, genetic, environmental, and socio-cultural factors. Through understanding its causes, signs, and treatment modalities, strides can be made toward its eradication. The paper has explored the multifaceted nature of leprosy, delving into its etiology, pathophysiology, DSM-5 diagnosis, treatment regimens, and patient education. By highlighting the importance of early diagnosis, prompt treatment initiation, and comprehensive patient education, healthcare providers can mitigate disease progression, prevent disability, and address social stigma. Integrated approaches that combine medical interventions with community-based education initiatives are crucial for reducing the burden of leprosy and promoting inclusive attitudes toward affected individuals. Moving forward, continued research, advocacy, and public health efforts are essential to achieving the ultimate goal of eliminating leprosy as a public health concern. (Nursing Paper Example on Leprosy [SOLVED])

![Nursing Paper Example on Leprosy [SOLVED]](https://www.ncbi.nlm.nih.gov/books/NBK559307/bin/LeprosyBT.__SV1.jpg)

![Nursing Paper Example on Leptospirosis [SOLVED]](https://i.ytimg.com/vi/bUGHwww_KkQ/maxresdefault.jpg)

![Nursing Paper Example on Listeriosis [SOLVED]](https://microbenotes.com/wp-content/uploads/2021/11/Food-poisoning-by-Listeria-monocytogenes-Listeriosis.jpeg)
![Nursing Paper Example on Leukemia [SOLVED]](https://my.clevelandclinic.org/-/scassets/images/org/health/articles/4365-leukemia) Nursing Paper Example on Leukemia [SOLVED]
Nursing Paper Example on Leukemia [SOLVED]![Nursing paper Example on Lice [SOLVED]](https://www.recordonline.com/gcdn/authoring/2019/10/29/NTHR/ghows-TH-957f6d80-fe05-234c-e053-0100007fb823-917436b1.jpeg?crop=1554,879,x0,y371&width=1554&height=777&format=pjpg&auto=webp)