Nursing Paper Example on Tularemia
Nursing Paper Example on Tularemia
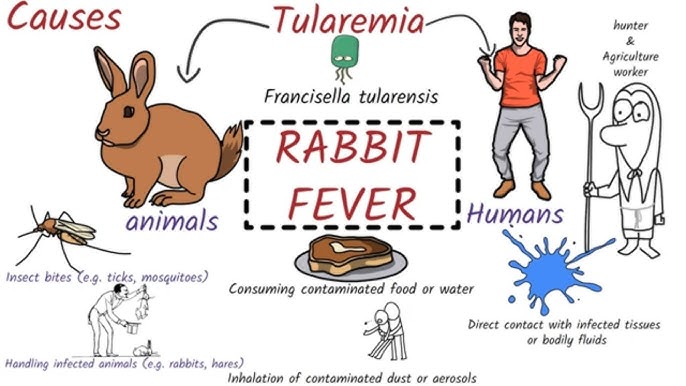
(Nursing Paper Example on Tularemia) Tularemia, also known as “rabbit fever” or “deer fly fever,” is a zoonotic infection caused by the bacterium Francisella tularensis. This infectious disease can affect humans and animals, with transmission occurring through contact with infected animals, insect bites, or contaminated environments. Tularemia is prevalent in North America, Europe, and parts of Asia, with a notable seasonal incidence due to its association with vector populations like ticks and flies.
Causes and Transmission of Tularemia
The bacterium Francisella tularensis, a gram-negative intracellular pathogen, is the causative agent of tularemia. Its highly infectious nature allows it to spread through various transmission routes, including vector bites, ingestion, and direct contact.
- Bacterial Cause:
- Francisella tularensis: This bacterium exists in multiple subspecies, with F. tularensis tularensis (Type A) common in North America and associated with severe cases, while F. tularensis holarctica (Type B) is found more widely and often causes milder disease (Centers for Disease Control and Prevention [CDC], 2023).
- Modes of Transmission:
- Vector Bites: Ticks, mosquitoes, and deer flies are common vectors, especially in endemic regions.
- Contact with Infected Animals: Exposure to infected animals, particularly rabbits and rodents, increases risk, especially through handling or skinning.
- Ingestion and Inhalation: Consuming contaminated water, food, or inhaling aerosolized particles from soil or animal tissues also transmits the bacteria (World Health Organization [WHO], 2023).
Signs and Symptoms of Tularemia
The symptoms of tularemia vary based on the route of infection and the specific form of the disease. The six primary forms of tularemia are ulceroglandular, glandular, oculoglandular, oropharyngeal, pneumonic, and typhoidal, each with its own symptom profile.
- Ulceroglandular Tularemia:
- Skin Ulcers: A skin ulcer forms at the site of infection, often accompanied by regional lymphadenopathy.
- Fever and Chills: These systemic symptoms are common in tularemia cases.
- Glandular Tularemia:
- Swollen Lymph Nodes: This form presents without skin ulcers but includes significant lymph node swelling.
- Oculoglandular Tularemia:
- Eye Pain and Redness: Infection occurs through the eye, causing conjunctivitis and swollen eye-associated lymph nodes (Mayo Clinic, 2023).
- Pneumonic Tularemia:
- Cough and Chest Pain: Inhalation of the bacterium results in respiratory symptoms, which can be life-threatening without treatment.
- Oropharyngeal Tularemia:
- Sore Throat and Mouth Ulcers: This form results from ingesting contaminated food or water, presenting with throat pain and gastrointestinal symptoms.
- Typhoidal Tularemia:
- Systemic Illness: The rarest and most severe form, causing high fever, systemic infection, and potentially leading to sepsis (Johns Hopkins Medicine, 2023).
Pathophysiology of Tularemia
Upon entry into the body, Francisella tularensis targets the reticuloendothelial system, particularly macrophages. The bacterium has several mechanisms to evade immune detection, survive within host cells, and trigger a strong inflammatory response.
- Intracellular Survival:
- After being phagocytosed by macrophages, the bacterium escapes into the cytoplasm, where it replicates, avoiding lysosomal destruction and triggering granuloma formation to contain the infection (National Institutes of Health [NIH], 2023).
- Spread and Immune Response:
- F. tularensis spreads from the initial infection site to lymph nodes and can enter the bloodstream, leading to systemic infection. The host immune response, while vigorous, may lead to significant inflammation and tissue damage, particularly in cases of pneumonic or typhoidal tularemia (CDC, 2023).
Diagnosis of Tularemia
Early diagnosis of tularemia is critical but challenging due to its non-specific symptoms. A combination of clinical, laboratory, and serological tests helps confirm the presence of F. tularensis.
- Clinical Assessment:
- Symptom Review and Exposure History: Physicians consider symptom patterns, possible exposure to vectors or infected animals, and any recent outdoor activities in endemic regions (WHO, 2023).
- Laboratory Tests:
- Culture: Blood or tissue samples are cultured in specialized laboratories due to the biohazardous nature of F. tularensis.
- Serology: Enzyme-linked immunosorbent assay (ELISA) and agglutination tests detect antibodies against F. tularensis in patient serum, confirming infection.
- Polymerase Chain Reaction (PCR): PCR testing identifies bacterial DNA quickly, making it useful in clinical settings (Mayo Clinic, 2023).
(Nursing Paper Example on Tularemia)
Treatment and Management of Tularemia
Early and appropriate antibiotic treatment is essential for tularemia recovery. The standard treatment duration varies depending on the disease severity and the antibiotics used.
- Antibiotic Therapy:
- Streptomycin and Gentamicin: Aminoglycosides are the primary drugs for tularemia treatment, with streptomycin being the preferred choice for severe cases.
- Doxycycline and Ciprofloxacin: For milder cases, tetracyclines and fluoroquinolones provide effective oral treatment options. Treatment generally lasts 10 to 21 days, depending on the drug and patient’s response (CDC, 2023).
- Supportive Care:
- Hydration and Symptom Management: Fever, pain, and inflammation management are important, especially for patients with respiratory symptoms or severe systemic illness.
- Infection Control: Due to its potential as a biohazard, infected patients should be handled carefully to avoid secondary transmission (Johns Hopkins Medicine, 2023).
Prevention and Control of Tularemia
Preventing tularemia centers on reducing exposure to the vectors and reservoirs that spread the bacterium. Personal protection measures and public health interventions play vital roles.
- Personal Protection:
- Protective Clothing: Wearing long sleeves and pants in wooded or grassy areas can reduce tick and fly bites.
- Insect Repellents: Applying repellents containing DEET to skin and clothing offers added protection against insect vectors.
- Public Health Measures:
- Tick and Fly Control: Efforts to reduce tick and fly populations in endemic areas, particularly during peak seasons, lower the risk of exposure.
- Avoiding Contact with Sick or Dead Animals: People should avoid handling wild animals, particularly in tularemia-endemic areas, or use gloves and protective gear when necessary (NIH, 2023).
- Awareness and Education:
- Educating communities in high-risk areas about tularemia transmission and prevention improves awareness and reduces infection rates, especially among outdoor workers, hunters, and recreational hikers.
Complications Associated with Tularemia
Tularemia, if left untreated or inadequately managed, can lead to severe complications, particularly in individuals with weakened immune systems.
- Pneumonia: Respiratory tularemia may progress to severe pneumonia, leading to complications such as lung abscesses or pleural effusion.
- Sepsis: Untreated or typhoidal forms of tularemia can lead to systemic infection and sepsis, which is life-threatening without prompt treatment.
- Long-term Effects: Chronic lymphadenopathy and ongoing fatigue may persist, especially after severe infections (WHO, 2023).
Conclusion
Tularemia remains a significant zoonotic disease in endemic regions, particularly affecting those who frequently interact with wildlife or live in rural areas. Given its potential as a bioterrorism agent due to its high infectivity, tularemia warrants vigilance in both public health and clinical contexts. Through preventive measures, prompt diagnosis, and effective antibiotic treatment, the impacts of tularemia can be minimized, protecting both individual health and public safety.
References
Centers for Disease Control and Prevention. (2023). Tularemia (Francisella tularensis) – Causes, Transmission, and Prevention. https://www.cdc.gov
Johns Hopkins Medicine. (2023). Tularemia: Symptoms, Diagnosis, and Treatment. https://www.hopkinsmedicine.org
Mayo Clinic. (2023). Tularemia: An Overview of Symptoms and Care Options. https://www.mayoclinic.org
National Institutes of Health. (2023). Understanding Tularemia: Pathophysiology and Public Health Implications. https://www.nih.gov
World Health Organization. (2023). Tularemia – Global Health Risks and Management. https://www.who.int


