Nursing Paper Example on Diabetic Ketoacidosis
Nursing Paper Example on Diabetic Ketoacidosis
Diabetic ketoacidosis (DKA) is a life-threatening complication of diabetes mellitus, predominantly type 1 diabetes, but it may also occur in type 2 diabetes. It is characterized by hyperglycemia, ketosis, and metabolic acidosis. DKA results from a severe insulin deficiency that leads to the accumulation of ketone bodies and a subsequent acidic environment. Early recognition and treatment are essential to prevent serious complications, including cerebral edema and multi-organ failure.
Causes of Diabetic Ketoacidosis
DKA results from insufficient insulin levels, combined with triggering factors.
Insufficient Insulin
In type 1 diabetes, autoimmune destruction of pancreatic beta cells results in absolute insulin deficiency.
In type 2 diabetes, severe stress or illness can precipitate a relative insulin deficiency.
Common Triggers
Infections: Pneumonia and urinary tract infections are the leading precipitating factors.
Non-compliance: Failure to adhere to insulin therapy or poor diabetes management.
New-onset diabetes: DKA is a common presentation in undiagnosed type 1 diabetes.
Acute illness: Myocardial infarction, stroke, or trauma can precipitate DKA.
Medications: Steroids and atypical antipsychotics can exacerbate hyperglycemia.
Signs and Symptoms
Early Symptoms
Polyuria, polydipsia, and dehydration due to osmotic diuresis.
Fatigue, malaise, and weight loss.
Advanced Symptoms
Abdominal pain, nausea, and vomiting from ketosis.
Kussmaul respiration: Deep, rapid breathing to compensate for metabolic acidosis.
Fruity-smelling breath due to acetone production.
Severe Symptoms
Altered mental status: Confusion, drowsiness, or coma in severe cases.
Hypotension and tachycardia due to severe dehydration and shock.
Etiology
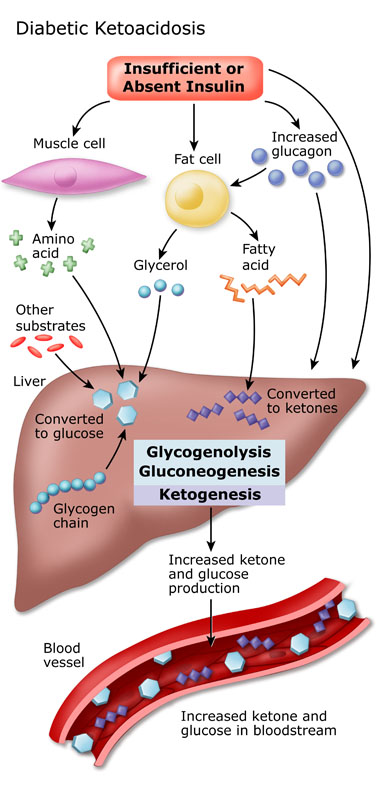
The etiology of DKA lies in the interplay between insulin deficiency and counter-regulatory hormone excess.
Pathological Insulin Deficiency
Insufficient insulin prevents glucose uptake by cells, leading to hyperglycemia.
Lipolysis occurs, producing free fatty acids that are converted to ketone bodies in the liver.
Hormonal Imbalance
Excess glucagon, cortisol, and catecholamines amplify glucose production and ketogenesis.
Pathophysiology
DKA develops through several interconnected metabolic pathways.
Hyperglycemia and Osmotic Diuresis
Reduced cellular glucose uptake causes hyperglycemia.
Hyperglycemia increases plasma osmolality, causing osmotic diuresis and electrolyte loss.
Ketogenesis and Acidosis
Free fatty acids undergo beta-oxidation in the liver, forming acetoacetate and beta-hydroxybutyrate.
Accumulated ketone bodies lead to metabolic acidosis, reducing blood pH.
Electrolyte Imbalance
Potassium shifts extracellularly in acidosis, causing apparent hyperkalemia despite total body potassium depletion.
Sodium and chloride losses exacerbate dehydration and acid-base imbalances.
Diagnosis
Clinical Presentation
Diagnosis begins with identifying hallmark symptoms: polyuria, polydipsia, nausea, and altered consciousness.
Laboratory Criteria
Blood glucose: ≥250 mg/dL.
Arterial pH: <7.3 indicates acidosis.
Serum bicarbonate: <18 mEq/L confirms metabolic acidosis.
Ketones: Elevated in serum and urine.
Differential Diagnosis
Hyperosmolar hyperglycemic state (HHS) lacks significant ketoacidosis.
Lactic acidosis and alcoholic ketoacidosis may mimic DKA.
Treatment Regimens
Fluid Replacement
Initial Resuscitation: Normal saline is used to restore intravascular volume.
Maintenance Fluids: Switch to half-normal saline or dextrose-containing fluids based on blood glucose levels.
Insulin Therapy
Continuous intravenous insulin infusion corrects hyperglycemia and suppresses ketogenesis.
Transition to subcutaneous insulin is made once the patient stabilizes.
Electrolyte Management
Potassium supplementation is critical to prevent hypokalemia as acidosis resolves.
Monitor and correct magnesium and phosphate levels if needed.
Acidosis Correction
Bicarbonate therapy is controversial and reserved for severe acidosis (pH <6.9).
Monitoring
Regular assessment of blood glucose, electrolytes, and acid-base status is essential during treatment.
Patient Education
Diabetes Management
Stress the importance of insulin adherence and blood glucose monitoring.
Teach patients how to adjust insulin doses during illness or stress.
Recognizing Early Signs
Educate patients on the symptoms of hyperglycemia and ketosis.
Encourage early medical consultation to prevent DKA progression.
Sick-Day Guidelines
Maintain hydration and carbohydrate intake during illnesses.
Check blood glucose and ketones frequently during periods of stress or infection.
Complications of Diabetic Ketoacidosis
Short-Term Complications
Cerebral Edema: Most common in children, resulting from rapid fluid shifts.
Severe Hypokalemia: Can cause life-threatening arrhythmias.
Long-Term Complications
Recurrent DKA episodes may accelerate diabetes-related complications.
Mortality
Mortality rates are higher in elderly patients and those with comorbidities.
Prognosis
The prognosis of DKA depends on timely intervention and effective diabetes management. Mortality rates are low in patients receiving prompt care, but recurrent episodes may indicate poor disease control and require intensive education.
Conclusion
Diabetic ketoacidosis is a critical medical condition requiring immediate attention. Effective treatment and patient education significantly improve outcomes. Healthcare providers must focus on identifying precipitating factors, delivering comprehensive care, and preventing recurrence through personalized diabetes management.
References
Kitabchi, A. E., Umpierrez, G. E., Miles, J. M., & Fisher, J. N. (2009). Hyperglycemic Crises in Adult Patients with Diabetes. Diabetes Care, 32(7), 1335-1343. https://diabetesjournals.org/care/article/32/7/1335/29956/Hyperglycemic-Crises-in-Adult-Patients-With
Dhatariya, K. K., et al. (2020). Management of Diabetic Ketoacidosis in Adults. Endocrine Reviews, 41(5), 756-773. https://academic.oup.com/edrv/article/41/5/756/5857546
Umpierrez, G. E., & Korytkowski, M. (2016). Diabetic Emergencies: Ketoacidosis, Hyperglycemic Hyperosmolar State, and Hypoglycemia. Endocrinology and Metabolism Clinics of North America, 45(3), 689-710. https://www.endocrinology.theclinics.com/article/S0889-8529(16)30038-4/fulltext
UpToDate. (2023). Management of Diabetic Ketoacidosis. https://www.uptodate.com/contents/diabetic-ketoacidosis-management
Wolfsdorf, J. I., et al. (2018). ISPAD Clinical Practice Consensus Guidelines 2018: Diabetic Ketoacidosis and Hyperglycemic Hyperosmolar State. Pediatric Diabetes, 19(27), 155-177. https://onlinelibrary.wiley.com/doi/full/10.1111/pedi.12701


