Nursing Paper Example on Urinary Tract Infection (UTI)
Nursing Paper Example on Urinary Tract Infection (UTI)
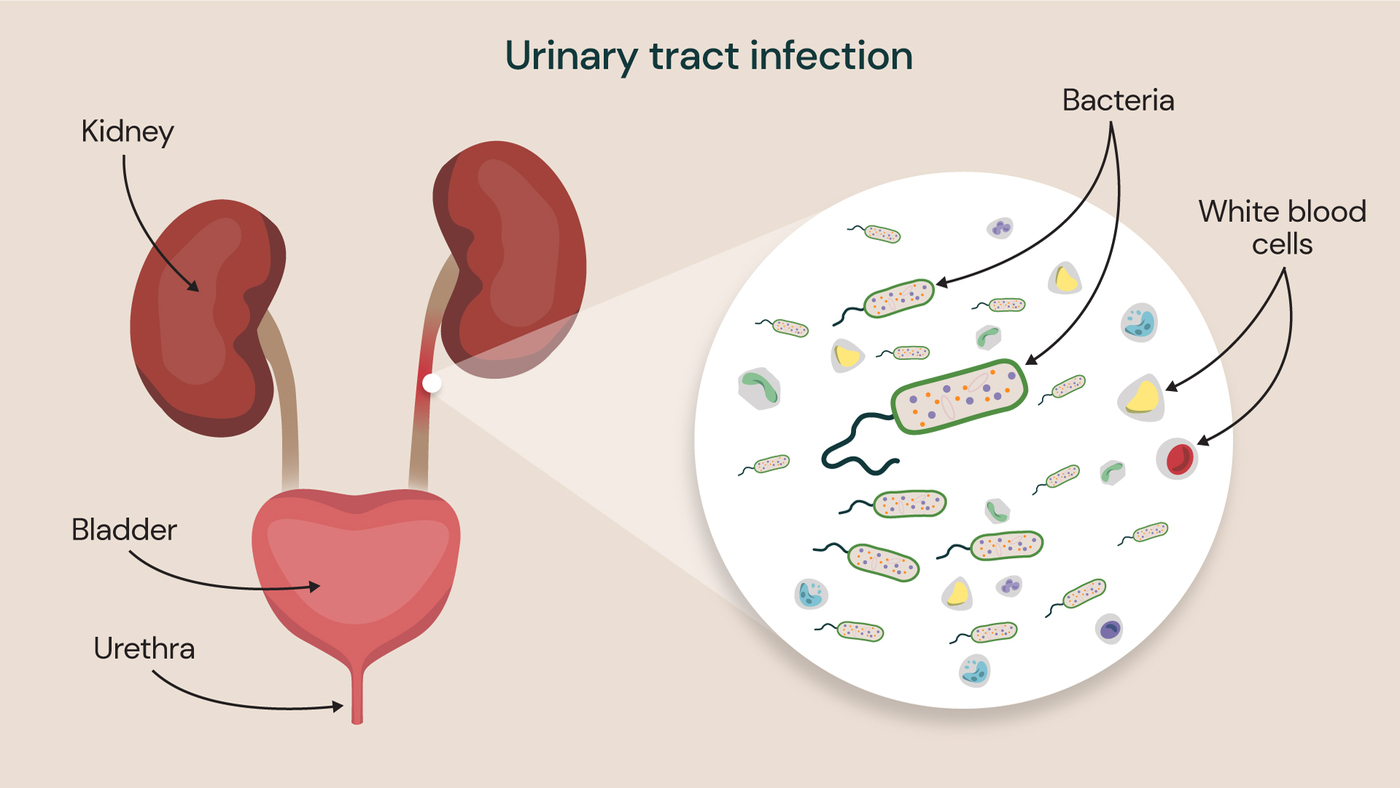
Urinary tract infections (UTIs) are among the most common infections affecting individuals globally, impacting millions each year. This paper addresses the causes, pathophysiology, types, symptoms, diagnosis, treatment, prevention, and potential complications of UTIs. By understanding these aspects, healthcare professionals can better manage and prevent UTIs, thereby reducing their impact on individuals’ health.
Causes of UTIs
UTIs are caused primarily by bacteria, with Escherichia coli accounting for about 80–90% of cases. Other pathogens include Klebsiella pneumoniae, Proteus mirabilis, Staphylococcus saprophyticus, and Enterococcus faecalis. These microorganisms can invade the urinary tract, typically via the urethra, and multiply in the bladder, causing an infection (Foxman, 2014).
The anatomical structure of the female urethra, which is shorter and closer to the anus, makes women more susceptible to UTIs than men. Other risk factors include sexual activity, pregnancy, menopause, urinary catheters, kidney stones, diabetes, and a weakened immune system (Gupta et al., 2011).
Pathophysiology of UTIs
When pathogenic bacteria enter the urethra, they can ascend into the bladder, where they colonize the uroepithelial cells. The immune system responds by triggering an inflammatory reaction, which produces classic UTI symptoms like pain and burning on urination. In severe cases, bacteria may travel up the ureters to infect the kidneys, leading to pyelonephritis. Uropathogens have various virulence factors, including adhesins, toxins, and iron-acquisition systems, which allow them to evade host defenses and persist within the urinary tract (Hannan et al., 2012).
Types of UTIs
Cystitis (Bladder Infection) – Cystitis refers to infection of the bladder, presenting with symptoms such as urgency, frequency, and dysuria. It is the most common form of UTI.
Pyelonephritis (Kidney Infection) – Pyelonephritis is a more severe form of UTI, characterized by flank pain, fever, and systemic symptoms. It results from bacterial spread to the kidneys and requires prompt treatment.
Urethritis – Urethritis involves infection or inflammation of the urethra and may result from sexually transmitted infections or bacteria from the intestinal flora.
Recurrent UTI – Defined as three or more episodes of UTI within a year, recurrent UTIs often require preventive strategies to avoid frequent antibiotic use.
Signs and Symptoms
The common symptoms of UTIs vary depending on the infection’s location:
Lower UTI (Cystitis):
- Urgency to urinate
- Increased frequency of urination
- Dysuria (painful urination)
- Hematuria (blood in the urine)
- Suprapubic pain
Upper UTI (Pyelonephritis):
- High fever and chills
- Flank pain or lower back pain
- Nausea and vomiting
- General malaise and fatigue (Gupta et al., 2011).
Diagnosis of UTIs
Urinalysis – Urinalysis is commonly used to identify signs of infection, such as elevated white blood cells, nitrites, and bacteria. The presence of leukocyte esterase and nitrite in the urine can indicate a bacterial infection.
Urine Culture – A urine culture confirms the presence and type of bacteria, guiding appropriate antibiotic treatment. Cultures are particularly important for patients with complicated or recurrent UTIs.
Imaging Studies – In recurrent or complicated cases, imaging studies such as ultrasound or computed tomography (CT) scans may be conducted to check for anatomical abnormalities or obstructions.
Antibiotic Sensitivity Testing – Antibiotic sensitivity testing helps identify the most effective antibiotic, especially in cases where there is concern about antibiotic resistance (Hooton, 2012).
Treatment of UTIs
Antibiotics – Antibiotics are the primary treatment for bacterial UTIs. Common antibiotics include trimethoprim-sulfamethoxazole, nitrofurantoin, and fluoroquinolones. However, the choice depends on the type of UTI, bacterial resistance, and patient-specific factors.
Pain Relief – Nonsteroidal anti-inflammatory drugs (NSAIDs) and phenazopyridine may help relieve pain, burning, and urgency during urination.
Increased Fluid Intake – Staying hydrated helps flush bacteria out of the urinary tract, aiding in faster recovery.
Hospitalization for Severe Infections – Patients with severe infections, such as pyelonephritis, or those with compromised immune systems may require hospitalization for intravenous antibiotics and fluids (Gupta et al., 2011).
Complications of UTIs
Recurrent Infections – Women with a history of UTIs are more prone to recurrent infections, which can impact quality of life and lead to antibiotic resistance.
Kidney Damage – Untreated UTIs, particularly pyelonephritis, can cause permanent kidney damage and scarring, leading to chronic kidney disease.
Sepsis – Severe UTIs can lead to sepsis, especially in immunocompromised patients, older adults, or those with indwelling catheters.
Pregnancy Complications – UTIs during pregnancy are associated with preterm labor, low birth weight, and preeclampsia, necessitating careful monitoring and management (Foxman, 2014).
Prevention of UTIs
Hydration and Frequent Urination – Drinking plenty of fluids and urinating regularly helps flush bacteria from the urinary tract.
Hygiene Practices – Proper hygiene, especially wiping from front to back, can reduce the risk of introducing bacteria into the urethra.
Avoiding Certain Products – Avoiding irritants such as perfumed feminine products and douches can reduce irritation and the risk of infection.
Prophylactic Antibiotics – For patients with recurrent UTIs, low-dose antibiotics may be prescribed as a preventive measure.
Cranberry Supplements – Some studies suggest that cranberry supplements may reduce UTI recurrence, although more research is needed to confirm their efficacy (Jepson & Craig, 2008).
References
Foxman, B. (2014). Epidemiology of urinary tract infections: incidence, morbidity, and economic costs. Disease-a-Month, 51(2), 45-70. https://doi.org/10.1016/j.disamonth.2005.11.005
Gupta, K., Hooton, T. M., Naber, K. G., Wullt, B., Colgan, R., Miller, L. G., Moran, G. J., Nicolle, L. E., Raz, R., Schaeffer, A. J., & Soper, D. E. (2011). International clinical practice guidelines for the treatment of acute uncomplicated cystitis and pyelonephritis in women: A 2010 update by the Infectious Diseases Society of America and the European Society for Microbiology and Infectious Diseases. Clinical Infectious Diseases, 52(5), e103-e120. https://doi.org/10.1093/cid/ciq257
Hannan, T. J., Totsika, M., Mansfield, K. J., Moore, K. H., Schembri, M. A., & Hultgren, S. J. (2012). Host-pathogen checkpoints and population bottlenecks in persistent and intracellular uropathogenic Escherichia coli bladder infection. FEMS Microbiology Reviews, 36(3), 616-648. https://doi.org/10.1111/j.1574-6976.2012.00339.x
Hooton, T. M. (2012). Clinical practice. Uncomplicated urinary tract infection. New England Journal of Medicine, 366(11), 1028-1037. https://doi.org/10.1056/NEJMcp1104429
Jepson, R. G., & Craig, J. C. (2008). Cranberries for preventing urinary tract infections. Cochrane Database of Systematic Reviews, 2008(1), CD001321. https://doi.org/10.1002/14651858.CD001321.pub5


