Nursing Paper Example on Babesiosis
Nursing Paper Example on Babesiosis
Babesiosis is a parasitic disease caused by protozoa of the Babesia genus. It is primarily transmitted through tick bites, particularly by the Ixodes scapularis tick, which also transmits Lyme disease. Human babesiosis is most commonly caused by Babesia microti in the United States. The infection is characterized by hemolytic anemia, fever, and other flu-like symptoms. Severe cases, especially in immunocompromised individuals, can lead to multi-organ failure and even death. The disease is endemic in certain regions, including the northeastern United States, but cases have been reported globally. Early recognition and treatment are crucial to prevent complications.
Causes of Babesiosis
The primary cause of babesiosis is infection with Babesia parasites.
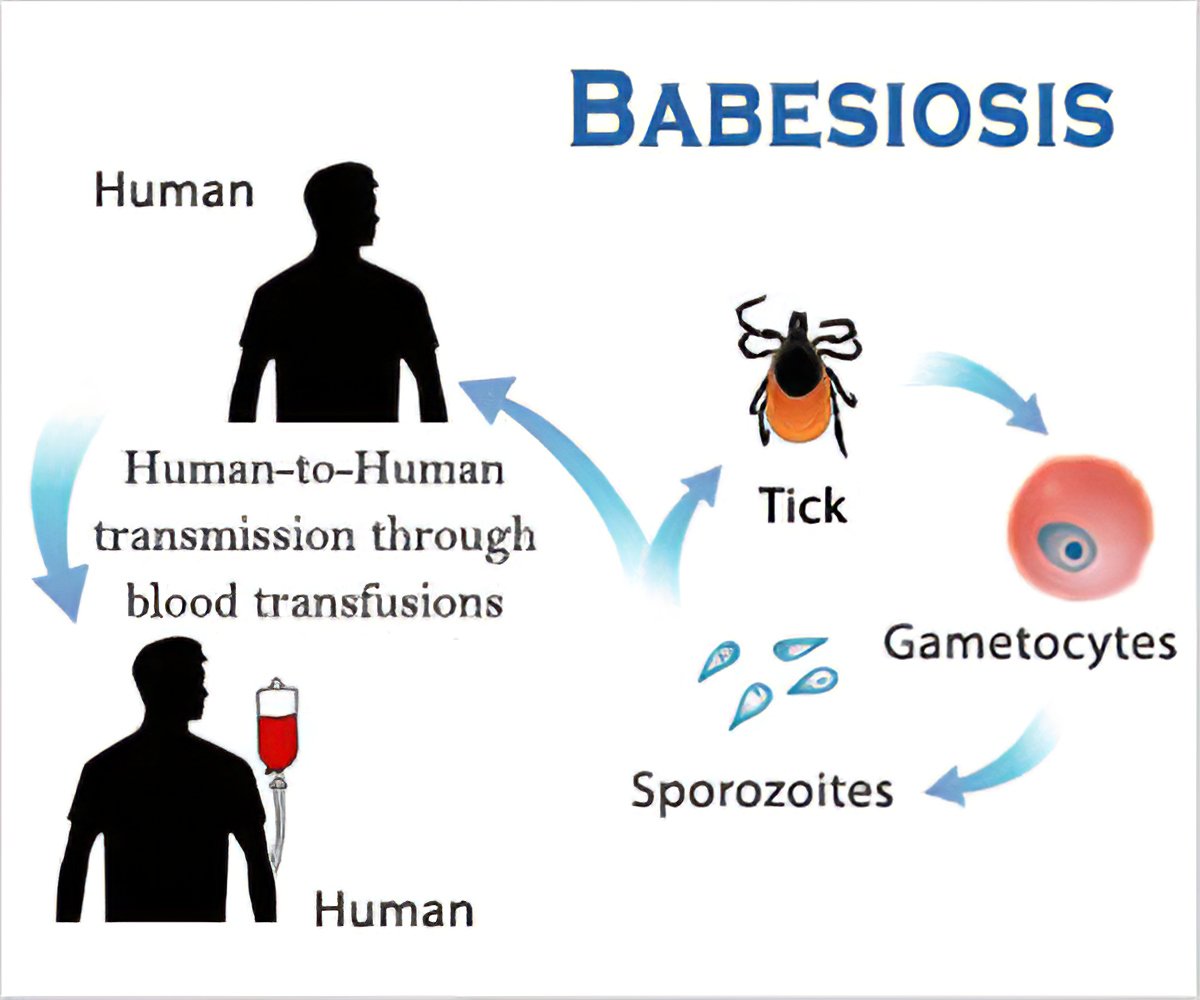
Tick bites: The most common mode of transmission is through the bite of infected Ixodes scapularis ticks.
Blood transfusion: Transmission can occur through contaminated blood transfusions, as Babesia parasites can survive in stored blood.
Congenital transmission: Rarely, the disease can be passed from an infected mother to her fetus.
Animal reservoirs: Small mammals like mice act as reservoirs for Babesia species, perpetuating the life cycle of the parasite.
These transmission routes highlight the zoonotic nature of babesiosis and its dependence on vector and reservoir dynamics.
Signs and Symptoms
The clinical presentation of babesiosis ranges from asymptomatic to severe.
- Mild to moderate symptoms:
Fever, chills, and fatigue.
Sweats, headache, and muscle aches.
Nausea and loss of appetite.
- Severe symptoms:
Hemolytic anemia causing jaundice and dark-colored urine.
Shortness of breath, chest pain, and organ dysfunction.
Splenomegaly or hepatomegaly in some cases.
The severity of symptoms is often greater in immunocompromised individuals, the elderly, and those without a spleen.
Etiology
The etiology of babesiosis involves the life cycle of Babesia parasites:
Tick infection: Ticks become infected when feeding on animals carrying Babesia parasites.
Human infection: Infected ticks transmit sporozoites into the human bloodstream.
Parasite replication: Inside red blood cells, sporozoites multiply, leading to cell rupture and further infection.
The cyclical replication and red blood cell destruction underlie the clinical manifestations of babesiosis.
Pathophysiology
The pathophysiology of babesiosis centers on the destruction of red blood cells and systemic inflammation.
Hemolysis: The parasite invades red blood cells, causing their rupture. This leads to anemia, jaundice, and hemoglobinuria.
Immune response: The body mounts an immune response, causing fever and inflammation.
Organ damage: Severe cases may involve microvascular occlusion, leading to ischemia and organ failure.
Splenic function: The spleen plays a vital role in clearing infected red blood cells, so individuals without a spleen are at greater risk of severe disease.
This cascade of events explains the wide spectrum of disease severity observed in affected individuals.
DSM-5 Diagnosis
Babesiosis is a parasitic infection and is not classified under the DSM-5. However, chronic disease and prolonged recovery may lead to psychological stress, depression, or anxiety in some patients.
Diagnosis
Diagnosing babesiosis involves a combination of clinical evaluation and laboratory tests.
Microscopic examination: A blood smear stained with Giemsa or Wright’s stain reveals the characteristic intraerythrocytic ring forms or tetrads (Maltese cross).
Polymerase chain reaction (PCR): PCR detects Babesia DNA with high sensitivity and specificity.
Serological tests: Detect antibodies against Babesia.
Complete blood count (CBC): Shows hemolytic anemia, thrombocytopenia, and leukopenia.
Liver function tests (LFTs): May show elevated liver enzymes in severe cases.
Early and accurate diagnosis is essential for initiating appropriate therapy.
Treatment Regimens
Treatment for babesiosis depends on the severity of the disease:
- Mild to moderate cases:
Antimicrobial therapy: Atovaquone combined with azithromycin is the first-line treatment. Treatment duration is usually 7-10 days.
- Severe cases:
Antimicrobial therapy: Clindamycin and quinine are used in severe cases.
Exchange transfusion: In cases of severe hemolysis or high parasitemia, exchange transfusion is performed to remove infected red blood cells.
Adjunctive therapies such as hydration and symptom management may also be necessary.
Patient Education
Educating patients about babesiosis is key to its prevention and management.
Tick prevention: Encourage the use of insect repellents containing DEET and protective clothing in tick-endemic areas.
Prompt tick removal: Teach patients how to properly remove ticks to minimize infection risk.
Blood donation precautions: Individuals diagnosed with babesiosis should avoid donating blood until cleared by a healthcare provider.
Symptom awareness: Patients should seek medical attention for unexplained fever or fatigue, especially after tick exposure.
Empowering patients with knowledge reduces disease incidence and severity.
Additional Considerations
Complications: Severe hemolysis, multi-organ failure, and relapsing infections may occur, particularly in high-risk groups.
Prognosis: Prognosis is excellent with timely treatment, but delayed diagnosis may result in prolonged recovery or fatality.
Epidemiology: While most cases occur in the United States, international travel and changing tick habitats may increase global cases.
Conclusion
Babesiosis is a significant vector-borne parasitic disease with variable clinical outcomes. Early recognition, accurate diagnosis, and prompt treatment are crucial for managing the disease effectively. Public health measures and patient education remain essential in controlling its spread and preventing severe complications, particularly in vulnerable populations.
References
Centers for Disease Control and Prevention. (2023). Babesiosis: Epidemiology and risk factors. https://www.cdc.gov/parasites/babesiosis/epi.html
Krause, P. J., & Wormser, G. P. (2021). Babesiosis: Clinical manifestations and diagnosis. Infectious Disease Clinics of North America, 35(2), 215–232. https://doi.org/10.1016/j.idc.2020.12.005
Vannier, E., & Krause, P. J. (2012). Human babesiosis. New England Journal of Medicine, 366(25), 2397–2407. https://doi.org/10.1056/NEJMra1202018
Bloch, E. M., & Patel, E. U. (2020). Babesia and blood transfusion: A hidden threat. Current Opinion in Hematology, 27(6), 416–423. https://doi.org/10.1097/MOH.0000000000000622


