Nursing Paper Example on Lichen Planus
Nursing Paper Example on Lichen Planus
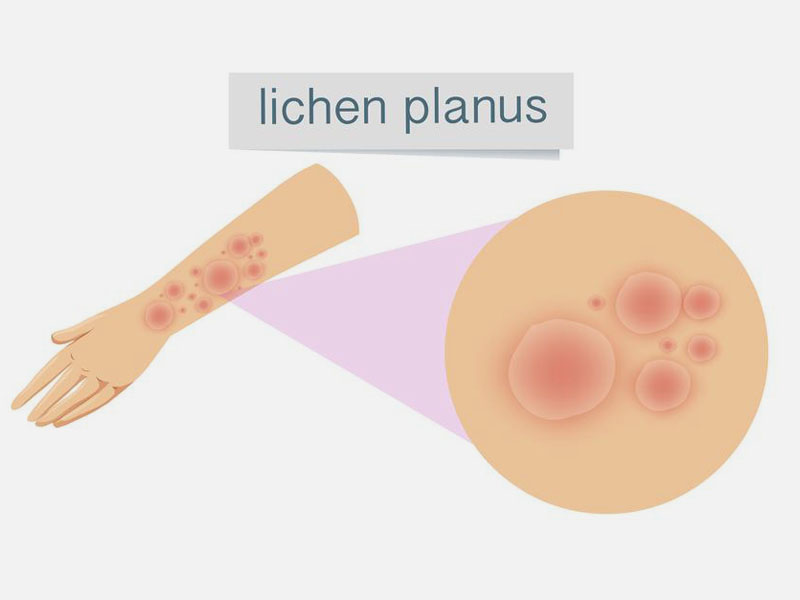
Lichen planus is a chronic inflammatory disease affecting the skin, mucous membranes, nails, and scalp. Characterized by pruritic, polygonal, purple papules and plaques, the condition is mediated by an abnormal immune response. Though the exact cause is unknown, it is linked to autoimmune disorders, viral infections, and certain medications. The disease predominantly affects adults aged 30–60 years and is more common in women. Early diagnosis and treatment are critical to managing symptoms and preventing complications, particularly when the oral or genital mucosa is involved.
Causes
The exact cause of lichen planus remains unclear, though it is believed to result from immune dysregulation.
Infections such as hepatitis C virus and Epstein-Barr virus are associated with the disease. These infections may trigger an immune response that attacks basal keratinocytes, leading to inflammation.
Certain medications, including nonsteroidal anti-inflammatory drugs, beta-blockers, and antimalarials, have been linked to drug-induced lichen planus. Stress and genetic predisposition may also contribute to the condition’s onset. Additionally, dental materials like amalgam fillings and contact allergens are recognized as potential triggers for oral lichen planus (Alrashdan et al., 2016).
While the disease is not contagious, identifying and addressing potential triggers can help in managing symptoms effectively.
(Nursing Paper Example on Lichen Planus)
Signs and Symptoms
Lichen planus presents with diverse symptoms, depending on the areas of involvement.
Cutaneous lichen planus manifests as pruritic, polygonal, purple papules with a characteristic Wickham’s striae—a network of fine white lines on the surface of the lesions. Commonly affected sites include the wrists, ankles, and lower back.
Oral lichen planus presents as white, lace-like patterns or painful erosions on the mucosa, often leading to difficulty eating or speaking. Genital involvement may result in painful ulcerations.
In scalp involvement, termed lichen planopilaris, patients experience hair loss and scarring. Nail lichen planus can cause ridges, thinning, or nail loss. The chronic and relapsing nature of the disease significantly impacts the quality of life (Lodi et al., 2020).
Etiology
Lichen planus is believed to have a multifactorial etiology, involving genetic, immunological, and environmental factors.
The disease results from an immune-mediated response targeting basal keratinocytes in the epidermis and mucosa. Genetic predisposition plays a role, as family clustering has been observed in some cases.
Hepatitis C virus infection and other viral triggers are strongly associated with lichen planus, suggesting an infectious component. Stress and trauma can exacerbate symptoms, a phenomenon known as the Koebner effect. Drug-induced lichen planus arises from hypersensitivity to specific medications (Alrashdan et al., 2016).
Understanding the interplay between these factors is crucial for tailoring treatment strategies and improving patient outcomes.
Pathophysiology
The pathophysiology of lichen planus involves T-cell-mediated destruction of basal keratinocytes.
In the affected tissues, cytotoxic CD8+ T-cells attack basal keratinocytes, leading to apoptosis and inflammation. This immune response is triggered by antigens expressed on keratinocytes, which may result from infection, drugs, or other environmental factors.
Histopathological examination reveals hyperkeratosis, a thickened granular layer, and a dense band-like lymphocytic infiltrate at the dermoepidermal junction. Civatte bodies, representing apoptotic keratinocytes, are another characteristic feature.
Oxidative stress and cytokine dysregulation also contribute to disease progression. Chronic inflammation may lead to scarring and tissue damage, especially in lichen planopilaris and erosive oral lichen planus (Lodi et al., 2020).
(Nursing Paper Example on Lichen Planus)
Diagnosis
Diagnosing lichen planus involves clinical evaluation, histopathological analysis, and laboratory tests.
Clinicians assess skin or mucosal lesions for their characteristic appearance and distribution. Dermoscopy aids in identifying Wickham’s striae, a diagnostic hallmark of the disease.
A skin or mucosal biopsy is often performed to confirm the diagnosis. Histological findings include hyperkeratosis, basal cell degeneration, and a band-like lymphocytic infiltrate at the dermoepidermal junction.
Laboratory tests may be used to rule out differential diagnoses such as lupus erythematosus or pemphigus. Hepatitis C screening is recommended for patients with suspected lichen planus due to the strong association between the two conditions (Alrashdan et al., 2016).
Treatment Regimens
Treatment of lichen planus focuses on symptom control, as there is no definitive cure.
Topical corticosteroids are the first-line treatment for cutaneous and oral lesions. Intralesional steroid injections may be used for localized, resistant lesions.
For severe or widespread cases, systemic therapies such as oral corticosteroids, retinoids, or immunosuppressants like methotrexate or cyclosporine are effective.
Phototherapy, particularly narrowband UVB or PUVA, is an option for extensive skin involvement.
Adjunctive treatments include antihistamines for pruritus and topical anesthetics for pain relief in oral lichen planus. Patients with drug-induced lichen planus should discontinue the offending medication under medical guidance. Regular monitoring and tailored treatment plans are essential for managing this chronic disease (Lodi et al., 2020).
Patient Education
Educating patients about lichen planus is vital for effective management and improved quality of life.
Patients should be informed about the chronic nature of the disease and the potential for relapses. Stress management techniques, such as mindfulness or counseling, may help reduce exacerbations.
For oral lichen planus, maintaining good oral hygiene and avoiding irritants like spicy foods or tobacco are crucial. Patients should report any changes in lesion appearance, as malignant transformation, although rare, can occur in oral forms.
Healthcare providers should emphasize adherence to treatment regimens and the importance of follow-up visits. Patients on immunosuppressive therapy require regular monitoring to minimize adverse effects. Empowering patients with knowledge fosters active participation in their care (Alrashdan et al., 2016).
Conclusion
Lichen planus is a complex autoimmune disease with variable clinical presentations and significant impacts on quality of life. While the exact etiology remains uncertain, factors such as chronic inflammation, viral infections, and drug hypersensitivity are implicated. Early diagnosis through clinical evaluation and histopathology is critical for effective management. Treatment focuses on alleviating symptoms and minimizing relapses, with corticosteroids being the mainstay therapy. Patient education plays a pivotal role in disease management, encouraging adherence to treatment and lifestyle modifications. Continued research is essential to unravel the disease’s mechanisms and develop targeted therapies.
References
Alrashdan, M. S., Cirillo, N., & McCullough, M. (2016). Oral lichen planus: A literature review and update. Archives of Dermatological Research, 308(8), 539-551. https://doi.org/10.1007/s00403-016-1675-9
Lodi, G., Scully, C., Carrozzo, M., Griffiths, M., Sugerman, P. B., & Thongprasom, K. (2020). Current controversies in oral lichen planus: Report of an international consensus meeting. Journal of Oral Pathology & Medicine, 49(6), 482-488. https://doi.org/10.1111/jop.13024
Sugerman, P. B., Savage, N. W., Walsh, L. J., & Seymour, G. J. (2020). Disease mechanisms in oral lichen planus. International Journal of Oral and Maxillofacial Surgery, 47(8), 857-871. https://doi.org/10.1016/j.ijom.2019.03.001


