Nursing Paper Example on Porphyria
Nursing Paper Example on Porphyria
Porphyria is a rare group of inherited or acquired disorders affecting the production of heme, a vital component of hemoglobin. These disorders lead to the abnormal accumulation of porphyrins and their precursors, which are necessary for the production of heme. Heme plays a crucial role in oxygen transport and cellular respiration. Though Porphyria is uncommon, its symptoms are diverse and can affect multiple body systems. Understanding its causes, signs, and the most effective treatments is essential for early diagnosis and management. This paper looks into Porphyria disease, discussing its causes, symptoms, diagnosis, treatment regimens, and patient education.
Causes
Signs and Symptoms
The signs and symptoms of Porphyria vary depending on the type of Porphyria, but they generally fall into two categories: acute and cutaneous. Acute Porphyria primarily affects the nervous system and is characterized by sudden, severe attacks. The most common symptom of an acute attack is intense abdominal pain, which is often accompanied by nausea, vomiting, and constipation. Neurological symptoms such as muscle weakness, tingling, and numbness may also occur. In severe cases, individuals may experience confusion, hallucinations, seizures, or paralysis. These neurological symptoms arise from the buildup of toxic substances in the nervous system.
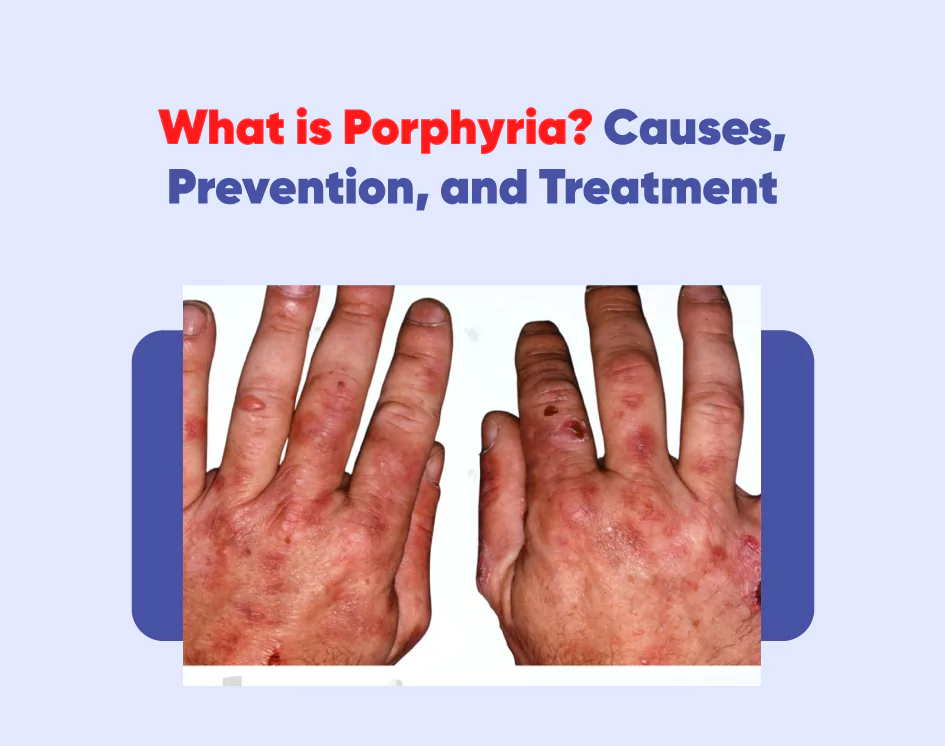
Cutaneous Porphyria, on the other hand, affects the skin. Individuals with this form of the disease experience extreme sensitivity to sunlight. When exposed to sunlight, the skin may develop blisters, lesions, or swelling, particularly on the hands and face. Over time, these areas may become discolored or scarred. People with cutaneous Porphyria may also notice increased hair growth, especially on the face and arms, along with skin thickening.
Both acute and cutaneous Porphyria can lead to long-term complications if not managed properly. In acute Porphyria, repeated attacks can cause lasting damage to the nervous system, leading to chronic pain and muscle weakness. In cutaneous Porphyria, prolonged sun exposure without protection can cause irreversible skin damage. Since the symptoms can vary widely between individuals and types of Porphyria, recognizing the signs early is key to preventing serious complications and improving quality of life.
Etiology
Porphyria arises from a combination of genetic and environmental factors that disrupt the heme biosynthesis pathway. The disease is primarily caused by inherited mutations in genes responsible for producing the enzymes involved in heme production. Each form of Porphyria is linked to a deficiency in one of these enzymes. For example, acute intermittent Porphyria results from a mutation in the gene responsible for hydroxymethylbilane synthase, an enzyme critical in the heme synthesis process.
Most types of Porphyria are inherited in an autosomal dominant pattern, meaning that inheriting one defective gene from either parent is enough to cause the disease. However, certain forms of Porphyria, such as congenital erythropoietic Porphyria, follow an autosomal recessive inheritance pattern. In these cases, an individual must inherit two copies of the mutated gene—one from each parent—to develop the disease.
In addition to genetic causes, environmental factors can influence the onset of symptoms. Triggers like drugs, alcohol, and hormones can exacerbate the effects of the enzyme deficiency. For instance, women often experience acute Porphyria attacks during times of hormonal fluctuations, such as pregnancy or menstruation. Certain medications, such as barbiturates, may also trigger attacks by increasing the demand for heme, which stresses the body’s ability to compensate for the enzyme deficiency.
Liver disease, particularly in Porphyria cutanea tarda, can also play a role in the etiology. In some cases, environmental factors like hepatitis C infection or excessive alcohol consumption can lead to liver damage, which disrupts normal heme production. Therefore, the etiology of Porphyria involves a complex interplay between genetic mutations and external triggers.
(Nursing Paper Example on Porphyria )
Pathophysiology
DSM-5 Diagnosis
Porphyria is not explicitly classified within the DSM-5 (Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition) as a psychiatric disorder. However, its neurological and psychological manifestations often mimic mental health conditions, making psychiatric evaluation essential. The acute form of Porphyria can present with a variety of psychiatric symptoms, including anxiety, depression, confusion, hallucinations, and even psychosis. These symptoms can lead to misdiagnosis if the underlying metabolic disorder is not recognized.
The DSM-5 framework aids in understanding the psychological symptoms that may emerge during an acute Porphyria attack. Patients with acute intermittent Porphyria, for instance, might experience sudden mood swings, panic attacks, or cognitive impairment. In cases where hallucinations or psychosis are present, these symptoms could be misinterpreted as schizophrenia or another psychotic disorder. Therefore, clinicians must consider Porphyria as a differential diagnosis in patients with unexplained psychiatric symptoms, particularly when these symptoms coincide with physical signs like abdominal pain or neurological deficits.
Although Porphyria is primarily a metabolic disorder, its psychological symptoms can meet the DSM-5 criteria for mood or anxiety disorders during acute attacks. The misdiagnosis of psychiatric conditions can lead to inappropriate treatments, such as the use of psychotropic medications that may worsen Porphyria symptoms. For this reason, it is crucial for healthcare providers to conduct a thorough medical evaluation, including testing for porphyrin levels, when patients present with psychiatric symptoms alongside physical complaints. Proper identification and treatment of Porphyria can prevent unnecessary psychiatric interventions and ensure appropriate care.
Treatment Regimens
The treatment of Porphyria depends on the type and severity of the condition. Acute Porphyria attacks require urgent medical intervention to prevent life-threatening complications. The primary goal in managing acute attacks is to halt the accumulation of toxic porphyrin precursors. Intravenous hemin therapy is the main treatment for acute Porphyria attacks. Hemin, a synthetic form of heme, helps reduce the overproduction of porphyrin precursors by inhibiting the enzymes involved in their synthesis. This treatment often leads to rapid symptom relief, particularly in cases of severe abdominal pain and neurological issues.
In mild cases of acute Porphyria, glucose therapy may be used. Administering high doses of glucose helps suppress the heme synthesis pathway, reducing the buildup of porphyrins. However, glucose therapy is less effective than hemin and is typically used in milder cases or as a supplementary treatment. Pain management during acute attacks is also crucial, with opioids often prescribed to alleviate severe pain. Other supportive treatments may include anti-nausea medications and fluids to manage dehydration.
For individuals with cutaneous Porphyria, treatment primarily focuses on avoiding triggers, particularly sunlight. Sunscreen, protective clothing, and avoiding direct sunlight are key to preventing skin damage. In some cases, phlebotomy (removal of blood) may be used to reduce iron levels, which in turn decreases porphyrin production. Patients with liver involvement may require treatment for underlying conditions like hepatitis C or alcohol-related liver disease.
(Nursing Paper Example on Porphyria )
Patient Education
Education is vital in managing Porphyria, as many attacks are preventable with lifestyle modifications. Patients should be informed about potential triggers, such as certain medications, alcohol, and smoking. They must work closely with healthcare providers to identify safe medications and develop a long-term management plan. Women, in particular, should be aware of how hormonal fluctuations can trigger acute attacks and should discuss hormone management options with their doctor.
Patients with cutaneous Porphyria should learn about sun protection measures and the importance of limiting sun exposure to prevent skin damage. Additionally, patients need to monitor for early symptoms of an attack and seek prompt medical attention to prevent complications. Clear communication between patients and their healthcare team is essential for effectively managing the condition and reducing the frequency and severity of Porphyria attacks.


