Soap Note Psychiatric Evaluation
Soap Note Psychiatric Evaluation
(Soap Note Psychiatric Evaluation) This is the temple for a Psych Soap note, please follow the template and complete, need less than 20% plagiarism, I have completed Bipolar Disorder, and Generalized Anxiety Disorder, pick a different diagnosis on an adult patient. Thank you!
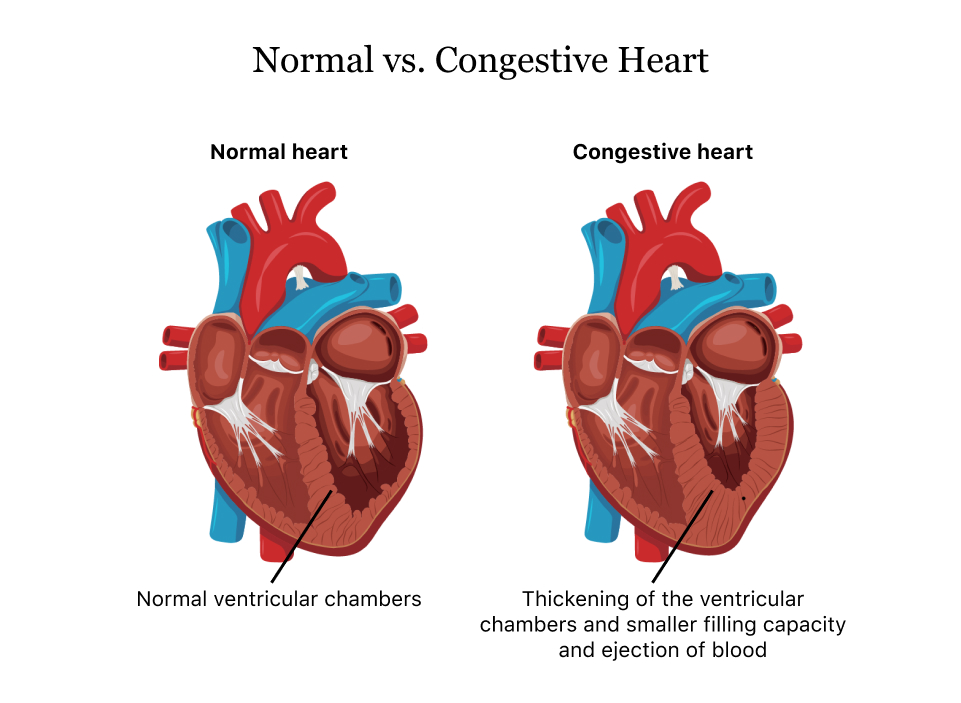
Congestive heart failure (CHF)
A 41-year-old obese male patient is diagnosed with congestive heart failure (CHF). He is told to begin a moderate exercise routine with a healthy diet and is prescribed several medications — including a diuretic. Based on your knowledge of the kidney and the disease of CHF, what factors would be important in selecting a specific diuretic? How would you explain to this patient how it works? If this patient developed a disease that caused the renal blood flow to be diminished, how might this impact the medication he is taking for his congestive heart failure? As his health care provider, how would you change his treatment in this situation?
Instructions: One to 1 page and a half is enough its a discussion post. APA style. Must have at least 3 references.
(Soap Note Psychiatric Evaluation)
Reduce drug costs
Post your cost comparison document from Unit 2. Assuming you might prescribe this drug for your patient, how would you minimize cost or assist the patient in getting the medication at the lowest cost possible. What resources are available to reduce drug costs? Find at least 2 resources for free or reduced cost medications. Respond to two other student posts as per the discussion board rubric.
Instructions: APA format discussion. 1 page length is fine. 3 references at least. nothing less. I posted the assignment from unit 2 below.
Shadow Health Digital Clinical Experience Health History Documentation
(Soap Note Psychiatric Evaluation)
Chief Complaint (CC), HPI, Current Medications, Allergies, Past Medical History, Family History, Social History and Review of Systems (ROS)
Rubric for grading
Subjective Documentation in Provider Note Template:
Subjective narrative documentation in Provider Note Template is detailed and organized and includes: Chief Complaint (CC), HPI, Current Medications, Allergies, Past Medical History, Family History, Social History and Review of Systems (ROS)
ROS: covers all body systems that may help you formulate a list of differential diagnoses.
You should list each system as follows: General: Head: EENT: etc. You should list these in bullet format and document the systems in order from head to toe.
(Soap Note Psychiatric Evaluation)


