Nursing Paper Example on Ulcerative Colitis
/in Assignment Help, Homework Help, Nursing Paper Help /by Aimee GraceNursing Paper Example on Ulcerative Colitis
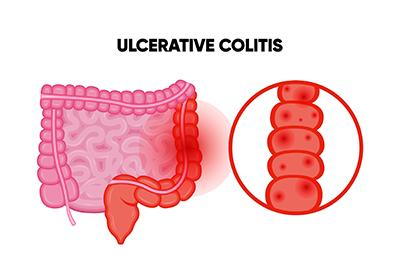
(Nursing Paper Example on Ulcerative Colitis) Ulcerative colitis is a chronic inflammatory bowel disease that affects the colon and rectum. This disease results in inflammation and ulcers in the innermost lining of the large intestine, leading to symptoms like abdominal pain, diarrhea, and rectal bleeding. Ulcerative colitis differs from other inflammatory bowel diseases, such as Crohn’s disease, as it is restricted to the colon and rectum.
Types of Ulcerative Colitis
Ulcerative colitis varies in severity and location within the colon. The disease is classified into several types:
Ulcerative Proctitis:
This type is limited to the rectum and usually presents with mild symptoms. Common symptoms include rectal bleeding and a sense of urgency to defecate.
Proctosigmoiditis:
Proctosigmoiditis affects the rectum and the sigmoid colon (the lower part of the colon). Symptoms include bloody diarrhea, abdominal pain, and tenesmus (a constant feeling of needing to defecate).
Left-Sided Colitis:
Left-sided colitis extends from the rectum up through the descending colon. Patients may experience weight loss, pain on the left side of the abdomen, and frequent bloody diarrhea.
Pancolitis:
Pancolitis affects the entire colon, resulting in severe symptoms such as weight loss, fatigue, and severe abdominal cramping.
Acute Severe Ulcerative Colitis:
This is a rare and potentially life-threatening form of ulcerative colitis that affects the entire colon. It is characterized by severe pain, profuse bleeding, and frequent diarrhea (Ordás et al., 2012).
(Nursing Paper Example on Ulcerative Colitis)
Causes and Risk Factors of Ulcerative Colitis
The exact cause of ulcerative colitis remains unknown, though a combination of genetic, environmental, and immunological factors contributes to its development.
Genetics:
Studies show that people with a family history of inflammatory bowel disease are at higher risk of developing ulcerative colitis, suggesting a genetic predisposition. Several gene mutations, including those in the IL23R gene, are associated with a heightened risk (Jostins et al., 2012).
Immune System Dysregulation:
Ulcerative colitis is thought to be an autoimmune disease where the immune system mistakenly attacks the cells of the colon, causing inflammation. This abnormal immune response is a significant factor in the pathogenesis of the disease (Ananthakrishnan, 2015).
Environmental Factors:
Diet, lifestyle, and geographic location also influence the risk of ulcerative colitis. High-fat diets, smoking, and living in urbanized and industrialized areas are associated with an increased risk. Some studies suggest a link between vitamin D deficiency and an increased likelihood of developing inflammatory bowel diseases, including ulcerative colitis (Ng et al., 2012).
Pathophysiology of Ulcerative Colitis
Ulcerative colitis primarily affects the mucosa, the innermost layer of the colon.
Inflammation and Ulceration:
The disease begins with inflammation in the mucosal lining, particularly in the rectum, which can extend proximally to other parts of the colon. Over time, the inflammation causes ulcer formation, resulting in bleeding and loss of the epithelial barrier in the colon (Ordás et al., 2012).
Immune Response and Cytokines:
The inflammatory process involves various immune cells, such as T-helper cells, which release cytokines like tumor necrosis factor-alpha (TNF-α), interleukin-1 (IL-1), and interleukin-6 (IL-6). These cytokines further drive inflammation and tissue damage within the colon (Atreya & Neurath, 2015).
Dysbiosis:
A disruption in the balance of gut bacteria, known as dysbiosis, is also observed in ulcerative colitis. The altered microbiome may contribute to inflammation and exacerbate symptoms, though the exact role remains under investigation (Kostic et al., 2014).
Signs and Symptoms of Ulcerative Colitis
The symptoms of ulcerative colitis vary according to the extent and severity of the inflammation.
Gastrointestinal Symptoms:
Patients commonly experience diarrhea, often accompanied by blood or pus, and abdominal pain. Tenesmus and rectal bleeding are typical for ulcerative proctitis, whereas more extensive disease may cause frequent diarrhea and weight loss.
Extraintestinal Manifestations:
Ulcerative colitis can cause symptoms outside the gastrointestinal tract, such as joint pain, eye inflammation (uveitis), skin lesions, and liver complications like primary sclerosing cholangitis (Ananthakrishnan, 2015).
Systemic Symptoms:
Fatigue, fever, and weight loss are common, especially during disease flare-ups. Anemia may result from chronic blood loss, leading to fatigue and pallor (Ordás et al., 2012).
Diagnosis of Ulcerative Colitis
The diagnosis of ulcerative colitis is based on a combination of clinical symptoms, laboratory tests, imaging, and endoscopic evaluations.
Laboratory Tests:
Blood tests may reveal anemia, elevated inflammatory markers (e.g., C-reactive protein and erythrocyte sedimentation rate), and low albumin levels. Stool tests help exclude infections as the cause of diarrhea (Kostic et al., 2014).
Endoscopy:
Colonoscopy is the primary tool for diagnosing ulcerative colitis. It allows direct visualization of the colon lining, showing continuous inflammation that typically starts in the rectum and extends proximally. Biopsies taken during endoscopy reveal histological changes characteristic of ulcerative colitis, such as crypt abscesses and mucosal inflammation (Ordás et al., 2012).
Imaging:
In severe cases, imaging like CT or MRI scans can assess the extent of inflammation and identify complications, such as toxic megacolon.
Treatment Options for Ulcerative Colitis
Ulcerative colitis treatment focuses on reducing inflammation, managing symptoms, and inducing and maintaining remission.
Medications:
Aminosalicylates: Drugs like mesalamine and sulfasalazine are first-line treatments for mild to moderate disease, particularly effective in reducing inflammation.
Corticosteroids: Steroids are used to manage moderate to severe flare-ups. However, long-term use is limited due to side effects.
Immunomodulators: Medications like azathioprine and 6-mercaptopurine suppress the immune response and help maintain remission.
Biologic Therapies: Biologics, including TNF-α inhibitors (e.g., infliximab) and integrin blockers (e.g., vedolizumab), target specific molecules in the inflammatory process, making them effective for severe disease (Ordás et al., 2012).
Surgical Interventions:
Surgery may be required for patients who do not respond to medical treatments or develop complications like toxic megacolon or colorectal cancer. The most common surgery is a proctocolectomy, which removes the colon and rectum, sometimes followed by the creation of an ileal pouch-anal anastomosis to allow stool to pass without the need for a permanent ostomy (Ng et al., 2012).
Lifestyle and Dietary Adjustments:
Patients are advised to avoid foods that trigger symptoms during flare-ups, such as high-fiber foods, dairy products, and fatty foods. Proper hydration, stress management, and regular exercise can also help manage symptoms (Ananthakrishnan, 2015).
Complications of Ulcerative Colitis
Toxic Megacolon:
Toxic megacolon is a life-threatening complication characterized by rapid colon dilation and a high risk of perforation. It requires immediate medical attention and often surgery.
Increased Cancer Risk:
Long-term ulcerative colitis, especially pancolitis, increases the risk of colorectal cancer. Regular screenings through colonoscopy are recommended to detect precancerous changes.
Nutritional Deficiencies:
Chronic inflammation, malabsorption, and blood loss contribute to nutritional deficiencies in iron, vitamin D, and other essential nutrients (Kostic et al., 2014).
Patient Education and Management
Educating patients on ulcerative colitis is essential for effective management.
Understanding Triggers:
Patients should learn to identify and avoid dietary and environmental triggers that worsen symptoms. Keeping a food diary can help pinpoint triggers (Ananthakrishnan, 2015).
Adherence to Treatment:
Regular medication adherence is critical for disease management and preventing flare-ups. Patients should understand the importance of following prescribed treatments even when symptoms improve.
Mental Health Support:
Ulcerative colitis can impact quality of life, leading to anxiety and depression. Mental health support, including counseling or support groups, can provide significant benefits.
Conclusion
Ulcerative colitis is a complex, chronic disease requiring lifelong management and regular medical care. The disease’s etiology combines genetic, immunological, and environmental factors. Effective treatment strategies include a combination of medications, lifestyle changes, and sometimes surgery. Continued advancements in biologic therapies offer new hope for patients with severe or refractory ulcerative colitis.
References
Ananthakrishnan, A. N. (2015). Epidemiology and risk factors for IBD. Nature Reviews Gastroenterology & Hepatology, 12(4), 205-217. https://doi.org/10.1038/nrgastro.2015.36
Jostins, L., Ripke, S., Weersma, R. K., et al. (2012). Host–microbe interactions have shaped the genetic architecture of inflammatory bowel disease. Nature, 491(7422), 119–124. https://doi.org/10.1038/nature11582
Kostic, A. D., Gevers, D., & Knight, R. (2014). The microbiome in inflammatory bowel disease. The Journal of Clinical Investigation, 124(10), 4194-4201. https://doi.org/10.1172/JCI78142
Ng, S. C., Shi, H. Y., Hamidi, N., et al. (2012). Worldwide incidence and prevalence of inflammatory bowel disease in the 21st century: A systematic review of population-based studies. The Lancet, 390(10114), 2769-2778. https://doi.org/10.1016/S0140-6736(17)32448-0
Ordás, I., Eckmann, L., Talamini, M., et al. (2012). Ulcerative colitis. The Lancet, 380(9853), 1606-1619. https://doi.org/10.1016/S0140-6736(12)60150-0


