Assignment
Chapter 12Knowledge Systems: Expert Systems, Recommenders, Chatbots, Virtual Personal Assistants, and Robo Advisors
Learning Objectives
· Describe recommendation systems
· Describe expert systems
· Describe chatbots
· Understand the drivers and capabilities of chatbots and their use
· Describe virtual personal assistants and their benefits
· Describe the use of chatbots as advisors
· Discuss the major issues related to the implementation of chatbots
Advancement in artificial intelligence (AI) technologies and especially natural language processing (NLP), machine and deep learning and knowledge systems, coupled with the increased quality and functionalities of other intelligent systems, and mobile devices and their apps, have driven the development of chatbots (bots) for inexpensive and fast execution of many tasks related to communication, collaboration, and information retrieval. The use of chatbots in business is increasing rapidly, partly because of their fit with mobile systems and devices. As a matter of fact, sending messages is probably the major activity in the mobile world.
In the last two to three years, many thousands of bots have been placed into service worldwide by both organizations (private and public) and individuals. Many people refer to these phenomena as the chatbot revolution. Chatbots today are much more sophisticated than those of the past. They are extensively used, for example, in marketing; customer, government, and financial services; healthcare; and in manufacturing. Chatbots make communication more personal than faceless computers and excel in data gathering. Chatbots can stand alone or be parts of other knowledge systems.
We divide the applications in this chapter into four categories: expert systems, chatbots for communication and collaboration, virtual personal assistants (native products, such as Alexa), and chatbots that are used as professional advisors. Some implementation topics of intelligent systems are described last.
This chapter has the following sections:
1. 12.1 Opening Vignette: Sephora Excels with Chatbots 649
2. 12.2 Expert Systems and Recommenders 650
3. 12.3 Concepts, Drivers, and Benefits of Chatbots 660
4. 12.4 Enterprise Chatbots 664
5. 12.5 Virtual Personal Assistants 672
6. 12.6 Chatbots as Professional Advisors (Robo Advisors) 676
7. 12.7 Implementation Issues 680
12.1 Opening Vignette: Sephora Excels with Chatbots
The problem
Sephora is a French-based cosmetics/beauty products company doing business globally. It has its own stores and sells its goods in cosmetic and department stores. In addition, Sephora sells online on Amazon and on its online store. The company sells hundreds of brands, including many of its own. It operates in a very competitive market where customer care and advertising are critical. Sephora sells some products for men, but most beauty products are targeted to women.
The Solution
Sephora’s first use of chatbots occurred through messaging services. The purpose of the first bot was to search for information for the company’s resources such as videos, images, tips, and so on. This bot operates in a question-and-answer (Q&A) mode. It recommends relevant content based on customers’ interests. The company aims to appeal to young customers messaging on Kik.
Sephora researchers found that customers conversing with the Kikbot were engaged deeply in the dialog. Then the bot encouraged them to explore new products. Sephora’s newer bot called Reservation Assistant was placed on Facebook Messenger. It enables customers to book or reschedule makeover appointments.
Another Sephora bot delivered on Kik is Shade-Matching. It matches lips colors to photos (face and lips) uploaded by users and recommends the best match to them. The bot also lets users try on photos of recommended colors, using Sephora Virtual Artist that runs on Facebook Messenger. Bots are deployed as mobile apps. If users like the recommendation, they are directed to the company’s Web store to buy the products. Users can upload photos taken with selfies so that the program can do the matching. Over 4 million visitors tried 90 million shades in the first year of Virtual Artist’s operation.
The Q&A collection of the knowledge base was built by connecting it with store experts. Knowledge acquisition techniques ( Chapter 2 ) were used for this purpose. The company’s bots use NLPs that were trained to understand the typical vocabulary of users.
The Results
The company’s customers loved the bots. In addition, Sephora learned the importance of providing assistance and guidance to users who are motivated to return (at a reasonable cost!), happier, and more engaged.
Sephora’s bot asks users questions to find their tastes and preferences. Then it acts like a recommendation system ( Section 12.2 ), offering products. Kik and Messenger users can purchase items without leaving the messaging service.
Finally, the company has improved the bots’ knowledge over time and plans new bots for additional tasks.
NOTE: Sephora was selected by Fast Company Magazine, March/April 2018, as one of the “World’s Most Innovative Companies.” Sephora is known for its digital transformation and innovation (Rayome, 2018). Also, Sephora’s bots are considered among the top marketing chatbots ( Quoc, 2017 ).
Sources: Compiled from Arthur (2016) , Rayome (2018), and Taylor (2016) , theverge.com/2017/3/16/14946086/sephora-virtual-assistant-ios-app-update-ar-makeup/ , and sephora.com/ .
Questions for the Opening Vignette
1. List and discuss the benefits of bots to the company.
2. List and discuss the benefits of bots to customers.
3. Why were the bots deployed via Messenger and Kik?
4. What would happen to Sephora if competitors use a similar approach?
What We Can Learn from This Vignette
In the highly competitive world of retail beauty products, customer care and marketing are critical. Using only live employees can be very expensive. In addition, customers are shopping 24/7,24/7, and physical stores are open during limited hours and days. In addition, there are large combinations of certain beauty products (e.g., many shades/colors) available. Sephora decided to use chatbots on Facebook Messenger and Kik to engage its customers. Chatbots, the subject of this chapter, are available 24/724/7 at a lower cost and are delivered via mobile devices. Bots deliver information to customers consistently and quickly direct customers to easy online shopping. Sephora placed its chatbots on messaging services. The logic was that people like to chat with friends on messaging services, and they may also like to chat with businesses.
In addition to several services to customers, using chatbots helps Sephora learn about customers. This type of chatbot is the most common type for customer care and marketing. In this chapter, we cover several other types of knowledge systems, including the pioneering expert systems, recommenders, virtual personal assistants offered by several large technology companies, and robo advisors.
12.2 Expert Systems and Recommenders
In Chapter 2 we introduced the reader to the concept of autonomous decision systems. An expert system is a category of autonomous decision systems and are considered the earliest applications of AI. Expert systems use started in research institutions in the early and mid-1960s (e.g., Stanford University, IBM) and was adopted commercially during the 1980s.
Basic Concepts of Expert Systems (ES)
The following are the major concepts related to ES technology.
Definitions
There are several definitions of expert systems. Our working definition is that an expert system is a computer-based system that emulates decision making and/or problem solving of human experts. These decisions and problems are in complex areas that require expertise to solve. The basic objective is to enable nonexperts to make decisions and solve problems that usually require expertise. This activity is usually performed in narrowly defined domains (e.g., making small loans, providing tax advice, analyzing reasons for machine failure). Classical ES use “what-if-then” rules for their reasoning.
Experts
An expert is a person who has the special knowledge, judgment, experience, and skills to provide sound advice and solve complex problems in a narrowly defined area. It is an expert’s job to provide the knowledge about how to perform a task so that a nonexpert will be able to do the same task assisted by ES. An expert knows which facts are important and understands and explains the dependent relationships among those facts. In diagnosing a problem with an automobile’s electrical system, for example, an expert car mechanic knows that a broken fan belt can be the cause for the battery to discharge.
There is no standard definition of expert, but decision performance and the level of knowledge a person has are typical criteria used to determine whether a particular person is an expert as related to ES. Typically, experts must be able to solve a problem and achieve a performance level that is significantly better than average. An expert at one time or in one region may not be an expert in another time or region. For example, a legal expert in New York may not be one in Beijing, China. A medical student may be an expert compared to the general public but not in making a diagnosis or performing surgery. Note that experts have expertise that can help solve problems and explain certain obscure phenomena only within a specific domain.
Typically, human experts are capable of doing the following:
· Recognizing and formulating a problem.
· Solving a problem quickly and correctly.
· Explaining a solution.
· Learning from experience.
· Restructuring knowledge.
· Breaking rules (i.e., going outside the general norms) if necessary.
· Determining relevance and associations.
Can a machine help a nonexpert perform like an expert? Can a machine make autonomous decisions that experts make? Let us see. But first, we need to explore what expertise is.
Expertise
An expertise is the extensive, task-specific knowledge that experts possess. The level of expertise determines the success of a decision made by an expert. Expertise is often acquired through training, learning, and experience in practice. It includes explicit knowledge, such as theories learned from a textbook or a classroom and implicit knowledge gained from experience. The following is a list of possible knowledge types used in ES applications:
· Theories about the problem domain.
· Rules and procedures regarding the general problem domain.
· Heuristics about what to do in a given problem situation.
· Global strategies for solving of problems amenable to expert systems.
· Meta knowledge (i.e., knowledge about knowledge).
· Facts about the problem area.
These types of knowledge enable experts to make better and faster decisions than nonexperts.
Expertise often includes the following characteristics:
· It is usually associated with a high degree of intelligence, but it is not always associated with the smartest person.
· It is usually associated with a vast quantity of knowledge.
· It is based on learning from past successes and mistakes.
· It is based on knowledge that is well stored, organized, and quickly retrievable from an expert who has excellent recall of patterns from previous experiences.
Characteristics and Benefits of ES
ES were used during the period 1980 to 2010 by hundreds of companies worldwide. However, since 2011, their use has declined rapidly, mostly due to the emergence of better knowledge systems, three types of which are described in this chapter. It is important, however, to understand the major characteristics and benefits of expert systems since many of them evolved evidenced newer knowledge systems.
The major objective of ES is the transfer of expertise to a machine. The expertise will be used by nonexperts. A typical example is a diagnosis. For example, many of us can use self-diagnosis to find (and correct) problems in our computers. Even more than that, computers can find and correct problems by themselves. One field in which such ability is practiced is medicine, as described in the following example:
Example: Are You Crazy?
A Web-based ES was developed in Korea for people to self-check their mental health status. Anyone in the world can access it and get a free evaluation. The knowledge for the system was collected from a survey of 3,235 Korean immigrants. The results of the survey were analyzed and then reviewed by experts via focus group discussions. For more information, see Bae (2013).
Benefits of ES
Depending on the mission and structure of ES, the following are their capabilities and potential benefits:
· Perform routine tasks (e.g., diagnosis, candidate screening, credit analysis) that require expertise much faster than humans.
· Reduce the cost of operations.
· Improve consistency and quality of work (e.g., reduce human errors).
· Speed up decision making and make consistent decisions.
· May motivate employees to increase productivity.
· Preserve scarce expertise of retiring employees.
· Help transfer and reuse knowledge.
· Reduce employee training cost by using self-training.
· Solve complex problems without experts and solve them faster.
· See things that even experts sometimes miss.
· Combine expertise of several experts.
· Centralize decision making (e.g., by using the “cloud”).
· Facilitate knowledge sharing.
These benefits can provide a significant competitive advantage to companies that use ES. Indeed, some companies have saved considerable amounts of money using them.
Despite these benefits, the use of ES is on the decline. The reasons for this and the related limitations are discussed later in this section.
Typical Areas for ES Applications
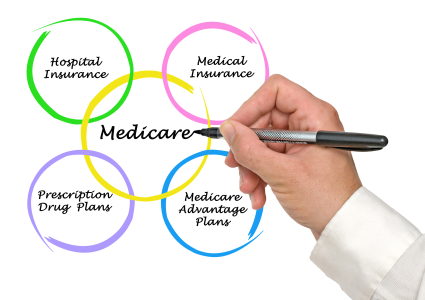
ES have been applied commercially in a number of areas, including the following:
· FINANCE. Finance ES include analysis of investments, credit, and financial reports; evaluation of insurance and performance; tax planning; fraud prevention; and financial planning.
· DATA PROCESSING. Data processing ES include system planning, equipment selection, equipment maintenance, vendor evaluation, and network management.
· MARKETING. Marketing ES include customer relationship management, market research and analysis, product planning, and market planning. Also, presale advice is provided for prospects.
· HUMAN RESOURCES. Examples of human resource ES are planning, performance evaluation, staff scheduling, pension management, regulatory advising, and design of questionnaires.
· MANUFACTURING. Manufacturing ES include production planning, complex product configuration, quality management, product design, plant site selection, and equipment maintenance and repair (including diagnosis).
· HOMELAND SECURITY. These ES include terrorist threat assessment and terrorist finance detection.
· BUSINESS PROCESS AUTOMATION. ES have been developed for desk automation, call center management, and regulation enforcement.
· HEALTHCARE MANAGEMENT. ES have been developed for bioinformatics and other healthcare management issues.
· REGULATORY AND COMPLIANCE REQUIREMENTS. Regulations can be complex. ES are using a stepwise process to ensure compliance.
· WEB SITE DESIGN. A good Web site design requires paying attention to many variables and ensures that performance is up to standard. ES can lead to a proper design process.
Now that you are familiar with the basic concepts of ES, it is time to look at the internal structure of ES and how their goals are achieved.
Structure and Process of ES
As you may recall from Section 2.5 and Figure 2.5, the process of knowledge extraction and its use is divided into two distinct parts. In ES we refer to these as the development environment and the consultation environment (see Figure 12.1). An ES builder builds the necessary ES components and loads the knowledge base with appropriate representation of expert knowledge in the development environment. A nonexpert uses the consultation environment to obtain advice and solve problems using the expert knowledge embedded into the system. These two environments are usually separated.
Major Components of ES
The major components in typical expert systems include:
· KNOWLEDGE ACQUISITION. Mostly from human experts, is usually obtained by knowledge engineers. This knowledge, which may derive from several sources, is integrated, validated, and verified.
· KNOWLEDGE BASE. This is a knowledge repository. The knowledge is divided into knowledge about the domain and knowledge about problem solving and solution procedures. Also, the input data provided by the users may be stored in the knowledge base.
· KNOWLEDGE REPRESENTATION. This is frequently organized as business rules (also known as production rules).
· INFERENCE ENGINE. Also known as the control structure or the rule interpreter, this is the “brain” of ES. It provides the reasoning capability, namely the ability to answer users’ questions, provide recommendations for solutions, generate predictions, and conduct other relevant tasks. The engine manipulates the rules by either forward chaining or backward chaining. In 1990s ES started to use other inference methods.
· USER INTERFACE. This component allows user inference engine interactions. In classical ES, this was done in writing or by using menus. In today’s knowledge systems, it is done by natural languages and voice.
These major components of ES generate useful solutions in many areas. Remember that these areas need to be well structured and in fairly narrow domains. Less common is a justifier/explanation subsystem that shows users of rule-based systems the chains of rules used to arrive at conclusions. Also, least common is a knowledge refining subsystem that helped to improve knowledge (e.g., rules) when new knowledge is added.
A major provider of expert systems technologies was Exsys Inc. While the company is no longer active in this business, its Web site (Exsys.com) is. It contains tutorials and a large number of cases related to its major software product, Exsys Corvid. Application Case 12.1 is one example.
Application Case 12.1 ES Aid in Identification of Chemical, Biological, and Radiological Agents
Terrorist attacks using chemical, biological, or radiological (CBR) agents are of great concern due to their potential for leading to large loss of life. The United States and other nations have spent billions of dollars on plans and protocols to defend against acts of terrorism that could involve CBR. However, CBR covers a wide range of input agents with many specific organisms that could be used in multiple ways. Timely response to such attacks requires rapid identification of the input agents involved. This can be a difficult process involving different methods and instruments.
The U.S. Environmental Protection Agency (EPA) along with Dr. Lawrence H. Keith, president of Instant Reference Sources Inc. and other consultants, have incorporated their knowledge, experience, and expertise as well as information in publicly available EPA documents to develop the CBR Advisor using Exsys Inc.’s Corvid software.
One of the most important parts of the CBR Advisor is providing advice in logical step-by-step procedures to determine the identity of a toxic agent when little or no information is available, which is typical at the beginning of a terrorist attack. The system helps response staff proceed according to a well-established action plan even in such a highly stressful environment. The system’s dual screens present three levels of information: (1) a top/executive level with brief answers, (2) an educational level with in-depth information, and (3) a research level with links to other documents, slide shows, forms, and Internet sites. CBR Advisor’s content includes:
· How to classify threat warnings.
· How to conduct an initial threat evaluation.
· What immediate response actions to take.
· How to perform site characterization.
· How to evaluate the initial site and safe entry to it.
· Where and how to best collect samples.
· How to package and ship samples for analysis.
Restricted content includes CBR agents and methods for analyzing them. The CBR Advisor can be used for incident response and/or training. It has two different menus, one for emergency response and another, longer menu for training. It is a restricted software program and is not publicly available.
Questions for Case 12.1
1. How can the CBR Advisor assist in making quick decisions?
2. What characteristics of the CBR Advisor make it an expert system?
3. What could be other situations in which similar expert systems can be employed?
Expert systems are also used in high-pressure situations in which human decision makers often need to take split-second actions involving both subjective as well as objective knowledge in responding to emergency situations.
Sources: www.exsys.com “Identification of Chemical, Biological and Radiological Agents” http://www.exsyssoftware.com/CaseStudySelector/casestudies.html. April 2018. (Publicly available information.) Used with permission.
Why the Classical Type of ES Is Disappearing
The large benefits described earlier drove the implementation of many ES worldwide. However, like many other technologies, the classical ES have been replaced by better systems. Let us first look at some of the limitations of ES that contributed to its declining use.
1. The acquisition of knowledge from human experts has proven to be very expensive due to the shortage of good knowledge engineers as well as the possible need to interview several experts for one application.
2. Any acquired knowledge needed to be updated frequently at a high cost.
1. The rule-based foundation was frequently not robust and not too reliable or flexible and could have too many exceptions to the rules. Improved knowledge systems use data-driven and statistical approaches to make the inferences with better success. In addition, case-based reasoning could work better only if a sufficient number of similar cases were available. So, usually it cannot support ES.
2. The rule-based user-interface needed to be supplemented (e.g., by voice communication, image maps). This could make ES too cumbersome.
3. The reasoning capability of rule-based technology is limited compared to use of newer mechanisms such as those used in machine learning.
New Generation of Expert SYSTEMS
Instead of using the old knowledge acquisition and representation system, newer ES based on machine learning algorithms and other AI technologies are deployed to create better systems. An example is provided in Application Case 12.2.
Application Case 12.2 VisiRule
VisiRule is an older ES company that remodeled its business over time. VisiRule (of the United Kingdom) provides easy-to-use diagramming tools to facilitate the construction of ES. Diagramming allows easier extraction and use of knowledge in expert systems.
The process of building the knowledge base can be seen on the left side of Figure 12.2. On the left-hand side, you can see the hybrid creation. Using a decision tree, the domain experts can create additional rules directly from relevant data (e.g., historical). In addition, rules can be created by machine learning (lower left side).
n). Using interactive questions and answers the system can generate advice. In addition, rules can be used to process data remotely and update the data repository. Note that the dual delivery option is based on machine learning’s ability to discover hidden patterns in data that can be used to form predictive decision models.
VisiRule also provides chatbots for improving the interactive part of the process and supplies an interactive map. According to the company’s Web site visirule.co.uk/, the major benefits of the product are:
· It is code-free; no programming is needed.
· The diagrams are drawn by human experts or induced automatically from data.
· It contains self-assessment tools with report generation and document production.
· The generated knowledge can be easily executed as XML code.
· It provides explanation and justification.
· The interactive expert advice attracts new customers.
· It can be used for training and advising employees.
· Companies can easily access the corporate knowledge repository.
· The charts to use VisiRule authoring tools are created with ease using flowcharting and decision trees.
· The charts allow creation of models that can be immediately executed and validated.
All-in-all, VisiRule provides a comprehensive AI-based expert system.
Source: Courtesy of VisiRule Corp. UK. Used with permission.
Questions for Case 12.2
1. Which of the limitations of early ES have been solved by the VisiRule system?
2. Compare Figures 12.2 and 12.1. What are the differences between the creation (Fig. 12.2) and the development (Fig. 12.1) subsystems?
3. Compare Figures 12.2 and 12.1. What are the differences between the delivery (Fig. 12.2) and the consultation (Fig. 12.1) subsystems?
4. Identify all AI technologies and list their contribution to the VisiRule system.
5. List some benefits of this ES to users.
Three major AI types of applications that overcome the earlier discussed limitations of RS are chatbots, virtual personal assistants, and robo advisors, which are presented next in this chapter. Other AI technologies that perform similar activities are presented in Chapters 4 to 9. Most notable is IBM Watson (Chapter 6); some of its advising capabilities are similar to those of ES but are much superior.
Another similar AI technology, the recommendation system, is presented next. Its newer variations use machine learning and IBM Watson Analytics.
Recommendation Systems
A heavily used knowledge system for recommending one-to-one targeted products or services is the recommendation system , also known as recommender system or recommendation engine. Such a system tries to predict the importance (rating or preference) that a user will attach to a product or service. Once the rating is known, a vendor knows users’ tastes and preferences and can match and recommend a product or service to the user. For comprehensive coverage, see Aggarwal (2016). For a comprehensive tutorial and case study, see analyticsvidhya.com/blood/2015/10/recommendation-engines/.
Recommendation systems are very common and are used in many areas. Top applications include movies, music, and books. However, there are also systems for travel, restaurants, insurance, and online dating. The recommendations are typically given in rank order. Online recommendations are preferred by many people over regular searches, which are less personalized, slower, and sometimes less accurate.
Benefits of Recommendation Systems
Using these systems may result in substantial benefits both to buyers and sellers (see Makadia, 2018).
Benefits to customers are:
· PERSONALIZATION. They receive recommendations that are very close to fulfilling what they like or need. This depends, of course, on the quality of the method used.
· DISCOVERY. They may receive recommendations for products that they did not even know existed but were what they really need.
· CUSTOMER SATISFACTION. With repeated recommendations tends to increase.
· REPORTS. Some recommenders provide reports and others provide explanations about the selected products.
· INCREASED DIALOG WITH SELLERS. Because recommendations may come with explanations, buyers may want more interactions with the sellers.
Benefits to sellers are:
· HIGHER CONVERSION RATE. With personalized product recommendations, buyers tend to buy more.
· INCREASED CROSS-SELL. Recommendation systems can suggest additional products. Amazon.com, for example, shows other products that “people bought together with the product you ordered.”
· INCREASED CUSTOMER LOYALTY. As benefits to customers increase, their loyalty to the seller increases.
· ENABLING OF MASS CUSTOMIZATION. This provides more information on potential customized orders.
Several methods are (or were) used for building recommendation systems. Two classic methods are collaborative filtering and content-based filtering.
Collaborative Filtering
This method builds a model that summarizes the past behavior of shoppers, how they surf the Internet, what they were looking for, what they have purchased, and how much they like (rate) the products. Furthermore, collaborative filtering considers what shoppers with similar profiles bought and how they rated their purchases. From this, the method uses AI algorithms to predict the preference of both old and new customers. Then, the computer program makes a recommendation.
Content-Based Filtering
This technique allows vendors to identify preferences by the attributes of the product(s) that customers have bought or intend to buy. Knowing these preferences, the vendor recommends to customers products with similar attributes. For instance, the system may recommend a text-mining book to a customer who has shown interest in data mining, or action movies after a consumer has rented one in this category.
Each of these types has advantages and limitations (see example at en.wikipedia.org/wiki/Recommender_system). Sometimes the two are combined into a unified method.
Several other filtering methods exist. Examples include rule-based filtering and activity-based filtering. Newer methods include machine learning and other AI technologies, as illustrated in Application Case 12.3.
Application Case 12.3 Netflix Recommender: A Critical Success Factor
According to ir.netflix.com, Netflix is (Spring 2018 data) the world’s leading Internet television network with more than 118 million members in over 190 countries enjoying more than 150 million hours of TV shows and movies per day, including original series, documentaries, and feature films. Members can view unlimited shows without commercials for a monthly fee.
The Challenges
Netflix has several million titles and now produces its own shows. The large titles inventory often creates a problem for customers who have difficulty determining which offerings they want to watch. An additional challenge is that Netflix expanded its business from the United States and Canada to 190 other countries. Netflix operates in a very competitive environment in which large players such as Apple, Amazon.com, and Google operate. Netflix was looking for a way to distinguish itself from the competition by making useful recommendations to its customers.
The Original Recommendation Engine
Netflix originally was solely a mail-order business for DVDs. At that time, it encountered inventory problems due to its customers’ difficulties in determining which DVDs to rent. The solution was to develop a recommendation engine (called Cinematch) that told subscribers which titles they probably would like. Cinematch used data mining tools to sift through a database of billions of film ratings and customers’ rental histories. Using proprietary algorithms, it recommended rentals to customers. The recommendation was accomplished by comparing an individual’s likes, dislikes, and preferences against those of people with similar tastes, using a variant of collaborative filtering. Cinematch was like the geeky clerk at a small movie store who sets aside titles he knows you will like and suggests them to you when you visit the store.
To improve Cinematch’s accuracy, Netflix began a contest in October 2016, offering $1$1 million to the first person or team that will write a program that would increase Cinematch’s prediction accuracy by at least 10 percent. The company understood that this would take quite some time; therefore, it offered a $50,000$50,000 Progress Prize each year in which the contest was conducted. After more than two years of competition, the grand prize went to Bellkor’s Pragmatic Chaos team, a combination of two runner-up teams.
To learn how the movie recommendation algorithms work, see quora.com/How-does-the-Netflix-movie-recommendation-algorithm-work/.
The New Era
As time passed, Netflix moved to the streaming business and then to Internet TV. Also, the spread of cloud technology enabled improvement in the recommendation system. The new system stopped making recommendations based on what people have seen in the past. Instead, it is using Amazon’s cloud to mimic the human brain in order to find what people really like in their favorite movies and shows. The system is based on AI and its technology of deep learning. The company can now visualize Big Data and draw insights for the recommendations. The analysis is also used in creating the company’s productions. Another major change dealt with the transformation to the global arena. In the past, recommendations had been based on information collected in the country (or region) where users live. The recommendations were based on what other people in the same country enjoyed. This approach did not work well in the global environment due to cultural, political, and social differences. The modified system considers what people who live in many countries view and their viewing habits and likes.
Implementation of the new system was difficult, especially when a new country or region was added. Recommendations were initially made without knowing much about the new customers. It took 70 engineers and a year of work to modify the recommendation system. For details, see Popper (2016).
The Results
As a result of implementing its recommender system, Netflix has seen very fast growth in sales and membership. The benefits include the following:
· EFFECTIVE RECOMMENDATIONS. Many Netflix members select their movies based on recommendations tailored to their individual tastes.
· CUSTOMER SATISFACTION. More than 90 percent of Netflix members say they are so satisfied with the Netflix service that they recommend it to family members and friends.
· FINANCE. The number of Netflix members has grown from 10 million10 million in 2008 to 118 million in 2018. Its sales and profits are climbing steadily. In spring 2018, Netflix stock sold for over $400$400 per share compared with $140$140 a year earlier.
Sources: Based on Popper (2016), Arora (2016), and StartUp (2016).
Questions for Case 12.3
1. Why is the recommender system useful? (Relate it to one-to-one targeted marketing.)
2. Explain how recommendations are generated.
3. Amazon disclosed its recommendation algorithms to the public but Netflix did not. Why?
4. Research the research activities that attempt to “mimic the human brain.”
5. Explain the changes due to the globalization of the company.
Section 12.2 Review Questions
1. Define expert systems.
2. What is the major objective of ES?
3. Describe experts.
4. What is expertise?
5. List some areas especially amenable to ES.
6. List the major components of ES and describe each briefly.
7. Why is ES usage on the decline?
8. Define recommendation systems and describe their operations and benefits.
9. How do recommendation systems relate to AI?