Nursing Paper Example on Anemia
Nursing Paper Example on Anemia
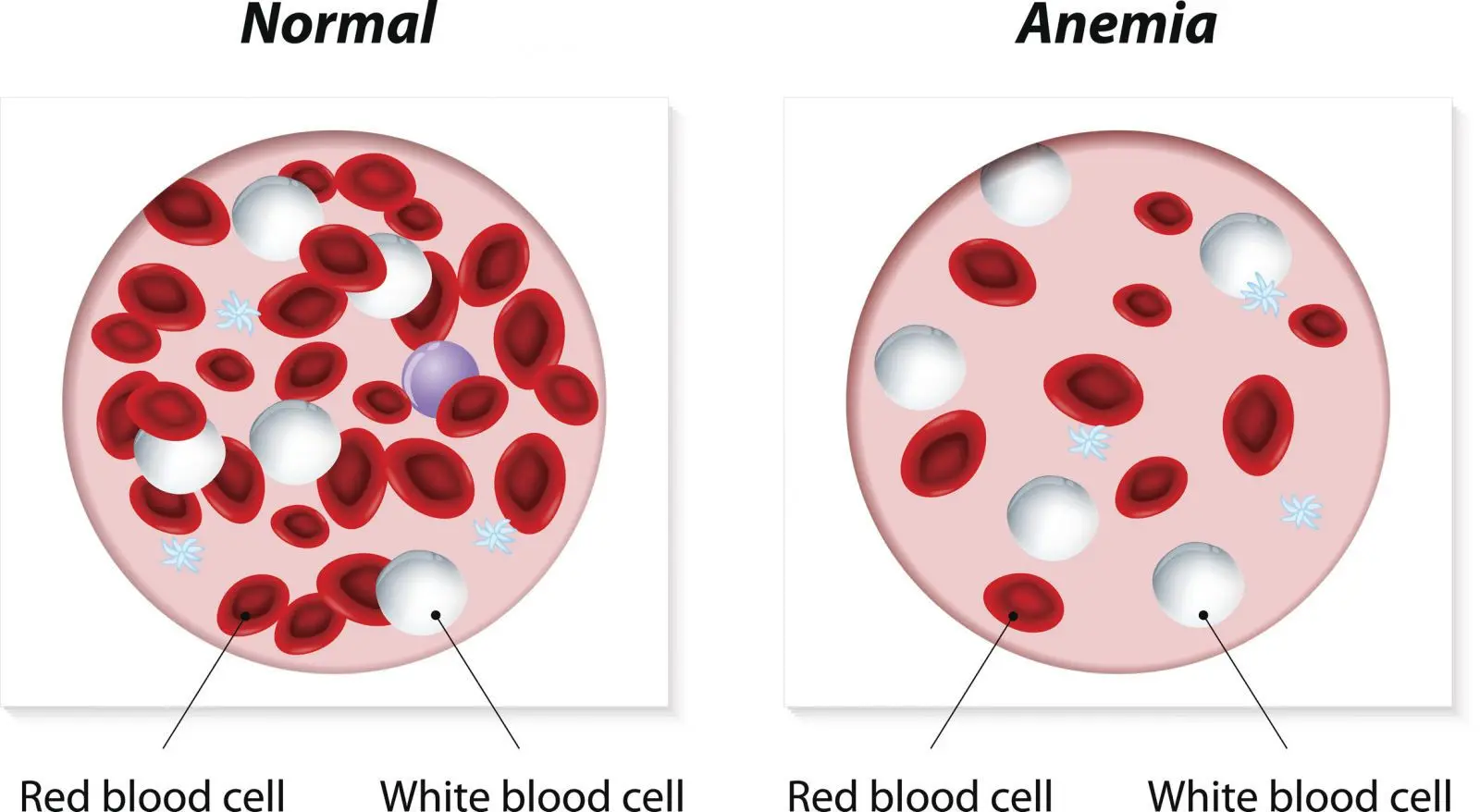
Anemia is a common condition defined by a reduction in the number or functionality of red blood cells or hemoglobin, resulting in insufficient oxygen transport to tissues. It can cause a range of symptoms, from mild fatigue to severe complications affecting multiple organ systems. Anemia is classified into several types based on underlying causes, such as iron deficiency, chronic diseases, and genetic conditions, each necessitating distinct approaches to diagnosis, management, and prevention.
Types of Anemia
- Iron Deficiency Anemia: The most prevalent form, caused by a lack of iron, which is necessary for hemoglobin synthesis. Common causes include inadequate dietary intake, blood loss (e.g., from menstruation or gastrointestinal bleeding), and malabsorption (Mayo Clinic, 2023).
- Vitamin Deficiency Anemias: Deficiencies in vitamins, particularly vitamin B12 and folate, affect red blood cell production. Pernicious anemia is a type of vitamin B12 deficiency caused by the immune system attacking cells in the stomach that help absorb B12.
- Anemia of Chronic Disease: Chronic conditions, including kidney disease, cancer, and autoimmune disorders, can reduce red blood cell lifespan or impair red blood cell production due to cytokine production and inflammatory responses.
- Aplastic Anemia: A rare condition resulting from bone marrow failure, where the body’s bone marrow fails to produce sufficient blood cells, often due to autoimmune responses or environmental factors.
- Hemolytic Anemia: Occurs when red blood cells are destroyed faster than they can be produced. Causes include autoimmune reactions, genetic conditions like sickle cell disease, and certain infections (National Heart, Lung, and Blood Institute [NHLBI], 2023).
- Sickle Cell Anemia: An inherited form of hemolytic anemia, sickle cell anemia causes red blood cells to assume an abnormal crescent shape. These cells can block blood flow, causing severe pain and organ damage.
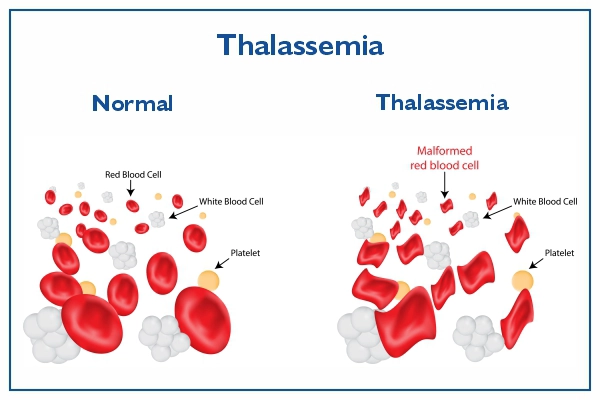
- Thalassemia: A genetic disorder leading to abnormal hemoglobin production, which can result in severe anemia and requires long-term management, including blood transfusions and iron chelation.
Pathophysiology
The pathology of anemia varies based on the specific type. Generally, anemia involves either a reduction in the production of red blood cells, an increase in red blood cell destruction, or significant blood loss.
- Iron Deficiency: Leads to microcytic (small-sized) and hypochromic (pale) red blood cells due to a lack of iron needed for hemoglobin synthesis.
- Vitamin Deficiency: Causes macrocytic (large-sized) red blood cells due to DNA synthesis impairment in the bone marrow.
- Hemolytic Anemias: The immune system or inherited conditions, such as enzyme deficiencies, destroy red blood cells prematurely, overwhelming the body’s ability to replace them.
- Anemia of Chronic Disease: Inflammatory cytokines inhibit red blood cell production by reducing iron availability and decreasing erythropoietin response (American Society of Hematology [ASH], 2022).
Signs and Symptoms
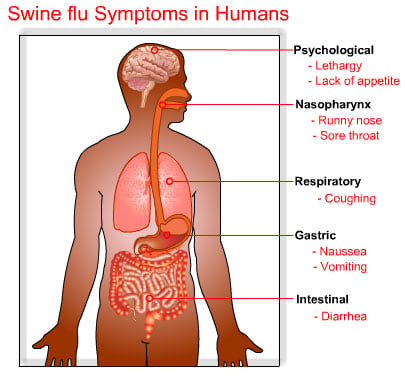
Symptoms of anemia vary depending on severity and type but often include:
- Fatigue and Weakness: Due to insufficient oxygen in the muscles and tissues.
- Pallor: Caused by reduced red blood cells, often evident in the skin and mucous membranes.
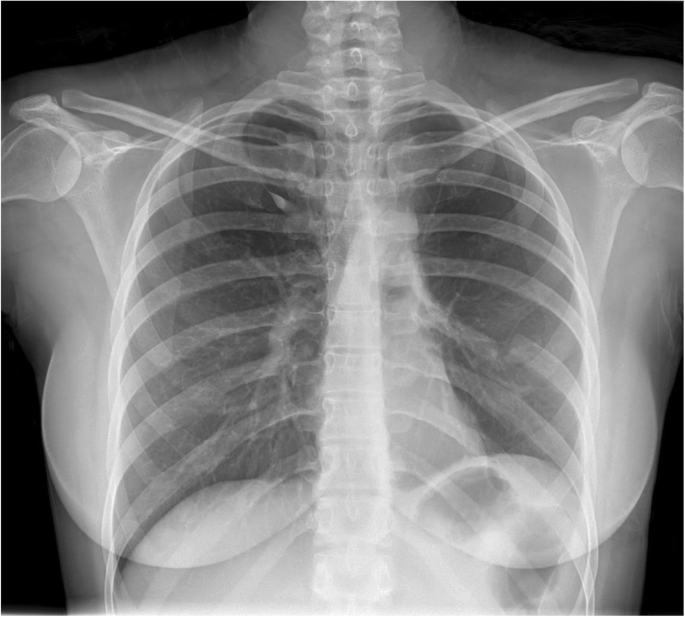
- Shortness of Breath: Especially during exertion, due to low oxygen levels.
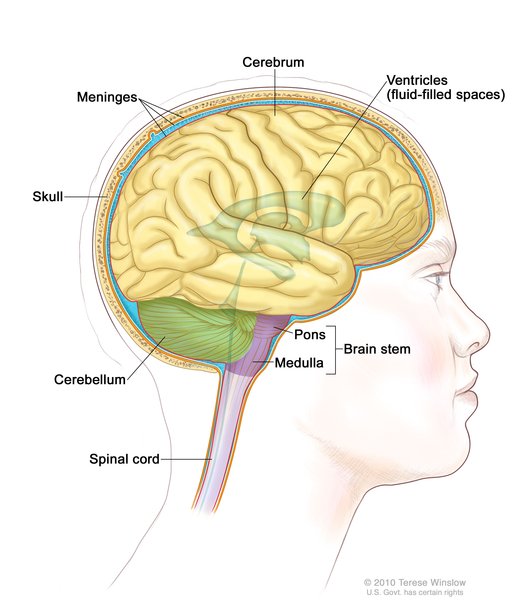
- Dizziness or Light-headedness: Related to decreased oxygen delivery to the brain.
- Chest Pain and Palpitations: Severe cases can cause cardiac strain, especially in individuals with underlying heart conditions (World Health Organization [WHO], 2023).
(Nursing Paper Example on Anemia)
Diagnosis
The diagnosis of anemia involves a thorough clinical assessment and laboratory investigations.
- Complete Blood Count (CBC): Determines hemoglobin levels, hematocrit, and red blood cell indices like mean corpuscular volume (MCV) to help identify the type of anemia.
- Peripheral Blood Smear: Examines the size, shape, and color of red blood cells, providing further insight into specific types of anemia.
- Iron Studies: Includes serum iron, ferritin, total iron-binding capacity, and transferrin saturation, useful for diagnosing iron deficiency anemia.
- Vitamin B12 and Folate Levels: Assesses for deficiencies associated with macrocytic anemia.
- Bone Marrow Biopsy: Rarely performed, mainly to investigate unexplained anemia and assess for marrow production issues, such as aplastic anemia (Mayo Clinic, 2023).
Treatment Regimens
Treatment approaches vary by type and cause, with a focus on addressing underlying conditions and restoring adequate red blood cell levels.
- Iron Supplementation: The standard treatment for iron deficiency anemia, using oral or intravenous iron based on severity.
- Vitamin B12 and Folate Replacement: For individuals with vitamin deficiency anemia, treatment may involve dietary modifications or injections, especially in cases of pernicious anemia.
- Erythropoiesis-Stimulating Agents: These medications stimulate red blood cell production, especially useful in anemia of chronic disease or kidney disease.
- Blood Transfusions: Used in severe cases to immediately restore red blood cell levels, especially for aplastic anemia, hemolytic anemia, and severe thalassemia.
- Bone Marrow Transplant: May be indicated for patients with aplastic anemia or other severe inherited anemias, providing a potential cure (American Society of Hematology [ASH], 2022).
(Nursing Paper Example on Anemia)
Complications
Without proper management, anemia can lead to severe complications:
- Heart and Lung Strain: Chronic anemia can lead to heart failure or angina, as the heart must work harder to supply oxygen to tissues.
- Pregnancy Complications: Anemia during pregnancy increases the risk of premature birth and low birth weight.
- Organ Damage: Severe anemia, particularly from sickle cell disease or hemolytic anemia, may lead to organ damage due to chronic oxygen deprivation.
- Cognitive Impairment: In children, untreated anemia can impact cognitive development and performance in school (World Health Organization [WHO], 2023).
Prevention
Many types of anemia can be prevented through:
- Dietary Modifications: Iron-rich foods (red meat, beans), vitamin B12 (fish, eggs), and folate (leafy greens, beans) help maintain healthy red blood cell production.
- Iron Supplementation in High-Risk Groups: Women of childbearing age, pregnant individuals, and young children may benefit from iron supplements.
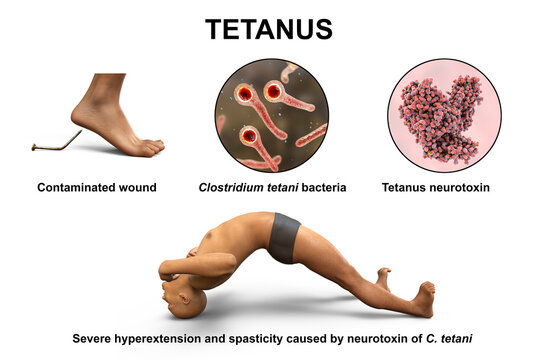
- Vaccination: Prevention of infections that can lead to anemia, such as malaria in endemic regions.
- Genetic Counseling: For inherited forms like sickle cell disease and thalassemia, genetic counseling offers important family planning guidance (NHLBI, 2023).
Conclusion
Anemia is a multifaceted condition with diverse causes, ranging from nutritional deficiencies to genetic disorders. Early diagnosis and targeted interventions are essential to prevent complications and improve outcomes, especially in populations at higher risk. Understanding anemia types and implementing tailored treatments allow for effective management of this condition, contributing to improved quality of life for affected individuals.
References
American Society of Hematology (ASH). (2022). Anemia Overview. https://www.hematology.org
Centers for Disease Control and Prevention (CDC). (2023). Anemia Information for Patients and Public. https://www.cdc.gov/hematology