Nursing paper Example on Crohn’s Disease: A Comprehensive Overview
Nursing paper Example on Crohn’s Disease: A Comprehensive Overview
Introduction
Crohn’s disease, a chronic inflammatory disorder of the gastrointestinal tract, poses significant challenges to patients and healthcare providers alike. Characterized by its unpredictable nature and diverse range of symptoms, Crohn’s disease affects individuals of all ages, often leading to debilitating complications and decreased quality of life. Despite extensive research efforts, the precise cause of Crohn’s disease remains elusive, with genetic, environmental, and immunological factors all implicated in its development. This paper aims to provide a comprehensive overview of Crohn’s disease, covering its causes, signs and symptoms, etiology, pathophysiology, DSM-5 diagnosis criteria, treatment regimens, and the importance of patient education. By understanding the complexities of this condition, healthcare professionals can better support patients in managing their symptoms and improving their overall well-being. (Nursing paper Example on Crohn’s Disease: A Comprehensive Overview)
Causes
Crohn’s disease is a multifactorial condition influenced by various genetic, environmental, and immunological factors. While the exact cause remains uncertain, several key contributors have been identified.
- Genetic Predisposition: Genetic factors play a significant role in the development of Crohn’s disease. Studies have shown that individuals with a family history of the disease are at a higher risk of developing it themselves. Variations in specific genes related to the immune system, such as NOD2/CARD15, have been strongly associated with Crohn’s disease susceptibility. These genetic predispositions can influence immune responses, barrier function in the intestine, and microbial interactions, contributing to disease pathogenesis.
- Environmental Factors: Environmental influences, including diet, smoking, and microbial infections, are known to impact the risk of developing Crohn’s disease. Dietary factors, such as high intake of refined sugars and fats and low intake of fruits and vegetables, have been implicated in disease onset and progression. Smoking is another significant environmental risk factor, as it not only increases the likelihood of developing Crohn’s disease but also worsens disease outcomes. Additionally, certain microbial infections, particularly in genetically susceptible individuals, can trigger abnormal immune responses and inflammation in the gastrointestinal tract, contributing to the development of Crohn’s disease.
- Immune System Dysfunction: Dysregulation of the immune system plays a central role in the pathogenesis of Crohn’s disease. In individuals with the disease, the immune system mistakenly targets harmless substances in the gut, leading to chronic inflammation. Abnormalities in immune cell function, such as increased production of pro-inflammatory cytokines and impaired regulatory T cell activity, contribute to sustained intestinal inflammation and tissue damage. Moreover, defects in the intestinal epithelial barrier, which normally prevents the entry of harmful substances into the gut, can further exacerbate immune dysregulation and inflammation in Crohn’s disease.
- Microbial Dysbiosis: Alterations in the composition and function of the gut microbiota, known as dysbiosis, have been implicated in the pathogenesis of Crohn’s disease. Changes in microbial diversity, abundance of specific bacterial species, and microbial metabolites have been observed in individuals with the disease. Dysbiosis can disrupt immune homeostasis, alter intestinal barrier function, and promote inflammation in the gut, contributing to the development and progression of Crohn’s disease.
Crohn’s disease arises from a complex interplay of genetic susceptibility, environmental factors, immune system dysfunction, and microbial dysbiosis. Understanding these underlying causes is crucial for developing targeted therapeutic strategies and interventions to manage and treat Crohn’s disease effectively. (Nursing paper Example on Crohn’s Disease: A Comprehensive Overview)
Signs and Symptoms
Abdominal Pain: One of the hallmark symptoms of Crohn’s disease is abdominal pain, which can vary in intensity and location. The pain is often described as cramping or sharp and may be located in the lower right abdomen, although it can occur anywhere in the abdomen.

Diarrhea: Persistent diarrhea is a common symptom of Crohn’s disease, resulting from inflammation and ulceration in the intestines. The diarrhea may be watery or contain blood and mucus and can lead to dehydration and electrolyte imbalances if not adequately managed.
Rectal Bleeding: Bleeding from the rectum is another common symptom of Crohn’s disease, often accompanied by blood in the stool. The bleeding results from inflammation and ulceration in the rectum and colon and can vary in severity from mild to severe.
Weight Loss: Unintentional weight loss is frequently observed in individuals with Crohn’s disease, particularly during flare-ups. Chronic inflammation in the intestines can impair nutrient absorption and lead to reduced appetite, resulting in weight loss over time.
Fatigue: Chronic inflammation and ongoing symptoms of Crohn’s disease can lead to fatigue and weakness in affected individuals. Fatigue may be exacerbated by anemia, a common complication of Crohn’s disease resulting from chronic blood loss or impaired iron absorption.
Fever: Fever is a common systemic symptom of Crohn’s disease, particularly during flare-ups of inflammation. The fever is typically low-grade but can indicate active disease and may be accompanied by other systemic symptoms such as chills and sweats.
Loss of Appetite: Reduced appetite and decreased food intake are common symptoms of Crohn’s disease, often associated with abdominal pain, nausea, and diarrhea. Loss of appetite can contribute to weight loss and nutritional deficiencies if not adequately addressed.
Joint Pain: Some individuals with Crohn’s disease experience joint pain and stiffness, particularly in the large joints such as the knees and hips. Joint pain may be related to inflammation in the intestines or to systemic inflammation affecting other parts of the body.
Delayed Growth and Development (in Children): Crohn’s disease can affect children’s growth and development, leading to delays in physical growth and puberty. Chronic inflammation, malnutrition, and treatment with corticosteroids can all contribute to delayed growth in children with Crohn’s disease.
Skin Problems: Skin problems such as erythema nodosum, pyoderma gangrenosum, and psoriasis can occur in individuals with Crohn’s disease. These skin conditions may be related to the underlying inflammatory process or may result from immune system dysfunction associated with the disease.
Crohn’s disease manifests with a range of symptoms affecting the gastrointestinal tract as well as systemic symptoms that can impact overall health and well-being. Recognizing and managing these symptoms is essential for improving quality of life and preventing complications in individuals with Crohn’s disease. (Nursing paper Example on Crohn’s Disease: A Comprehensive Overview)
Etiology
Crohn’s disease is a complex disorder with a multifactorial etiology involving genetic, environmental, and immunological factors. While the precise cause of Crohn’s disease remains unknown, several key contributors have been identified, shedding light on its pathogenesis.
Genetic Predisposition: Genetic factors play a significant role in the development of Crohn’s disease, with studies indicating a strong familial clustering of the condition. Variations in specific genes related to the immune system, such as NOD2/CARD15, have been strongly associated with Crohn’s disease susceptibility. These genetic predispositions can influence immune responses, barrier function in the intestine, and microbial interactions, contributing to disease pathogenesis.
Environmental Triggers: Environmental factors are known to influence the risk of developing Crohn’s disease. Factors such as diet, smoking, and microbial infections have been implicated in disease onset and progression. Dietary factors, including high intake of refined sugars and fats and low intake of fruits and vegetables, have been associated with increased risk of Crohn’s disease. Smoking is another significant environmental risk factor, as it not only increases the likelihood of developing Crohn’s disease but also worsens disease outcomes. Additionally, certain microbial infections, particularly in genetically susceptible individuals, can trigger abnormal immune responses and inflammation in the gastrointestinal tract, contributing to the development of Crohn’s disease.
Immunological Dysregulation: Dysregulation of the immune system plays a central role in the pathogenesis of Crohn’s disease. In individuals with the disease, the immune system mistakenly targets harmless substances in the gut, leading to chronic inflammation. Abnormalities in immune cell function, such as increased production of pro-inflammatory cytokines and impaired regulatory T cell activity, contribute to sustained intestinal inflammation and tissue damage. Moreover, defects in the intestinal epithelial barrier, which normally prevents the entry of harmful substances into the gut, can further exacerbate immune dysregulation and inflammation in Crohn’s disease.
Microbial Dysbiosis: Alterations in the composition and function of the gut microbiota, known as dysbiosis, have been implicated in the pathogenesis of Crohn’s disease. Changes in microbial diversity, abundance of specific bacterial species, and microbial metabolites have been observed in individuals with the disease. Dysbiosis can disrupt immune homeostasis, alter intestinal barrier function, and promote inflammation in the gut, contributing to the development and progression of Crohn’s disease.
In summary, Crohn’s disease arises from a complex interplay of genetic susceptibility, environmental triggers, immunological dysregulation, and microbial dysbiosis. Understanding these underlying etiological factors is crucial for developing targeted therapeutic strategies and interventions to manage and treat Crohn’s disease effectively.
Pathophysiology
Crohn’s disease is characterized by chronic inflammation of the gastrointestinal tract, resulting from a complex interplay of genetic, environmental, immunological, and microbial factors. Understanding the pathophysiology of Crohn’s disease is essential for developing targeted therapeutic approaches and improving patient outcomes.
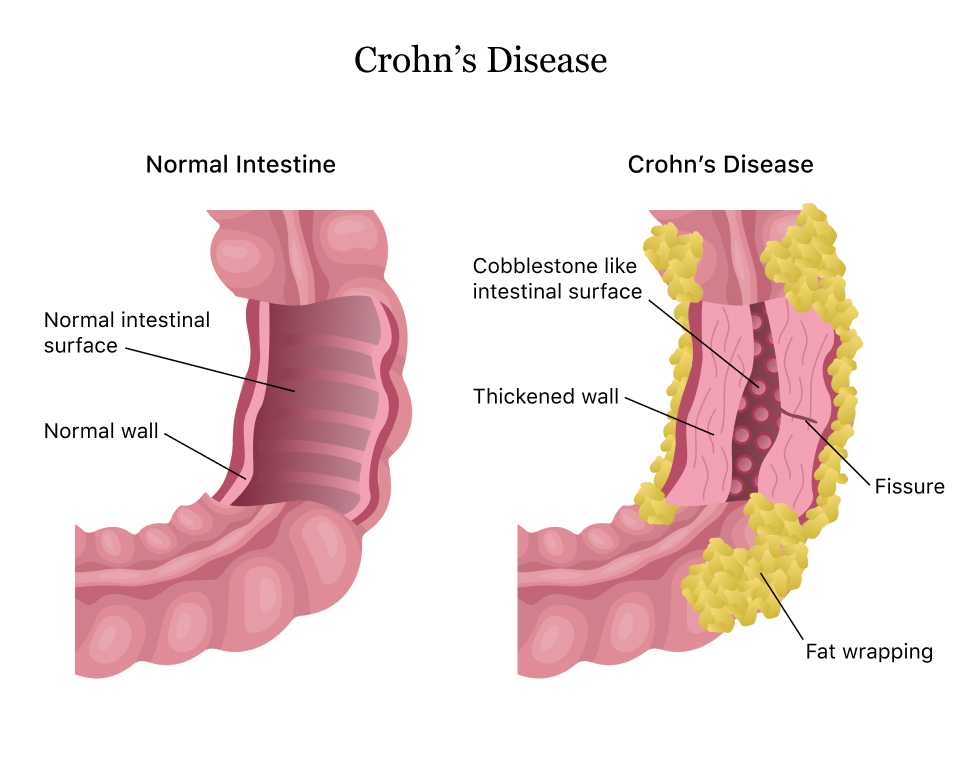
Intestinal Inflammation: Central to the pathophysiology of Crohn’s disease is chronic inflammation of the intestinal mucosa. This inflammation is characterized by the infiltration of immune cells, including T lymphocytes, macrophages, and neutrophils, into the intestinal wall. Pro-inflammatory cytokines such as tumor necrosis factor-alpha (TNF-α), interleukin-1 (IL-1), and interleukin-6 (IL-6) are released, perpetuating the inflammatory response and contributing to tissue damage.
Immune Dysregulation: Crohn’s disease is associated with dysregulated immune responses in the gastrointestinal tract. Abnormalities in immune cell function, including increased activation of T helper 1 (Th1) and Th17 cells and impaired regulatory T cell activity, contribute to sustained inflammation and tissue damage. Dysregulation of mucosal immune responses leads to the production of autoantibodies and inflammatory mediators, further exacerbating intestinal inflammation.
Intestinal Barrier Dysfunction: Disruption of the intestinal epithelial barrier is another key feature of Crohn’s disease pathophysiology. Genetic and environmental factors, along with dysbiosis of the gut microbiota, compromise the integrity of the intestinal epithelium, allowing the entry of luminal antigens and bacteria into the mucosa. This breach in the epithelial barrier triggers an abnormal immune response, leading to chronic inflammation and tissue damage.
Microbial Dysbiosis: Alterations in the composition and function of the gut microbiota, known as dysbiosis, play a significant role in the pathogenesis of Crohn’s disease. Dysbiosis disrupts the balance between commensal and pathogenic bacteria in the gut, leading to aberrant immune activation and inflammation. Changes in microbial diversity, abundance of specific bacterial species, and microbial metabolites contribute to intestinal inflammation and disease progression.
Tissue Remodeling and Fibrosis: Chronic inflammation in Crohn’s disease can lead to tissue remodeling and fibrosis in the gastrointestinal tract. Fibroblasts are activated, leading to excessive deposition of extracellular matrix proteins such as collagen and fibronectin. This fibrotic response results in the formation of strictures, fistulas, and other complications, contributing to the chronicity and progressive nature of the disease.
Crohn’s disease is characterized by chronic inflammation, immune dysregulation, intestinal barrier dysfunction, microbial dysbiosis, and tissue remodeling. A comprehensive understanding of the pathophysiology of Crohn’s disease is essential for developing targeted therapies aimed at modulating the immune response, restoring intestinal barrier function, and restoring microbial balance to improve patient outcomes.
DSM-5 Diagnosis
The diagnosis of Crohn’s disease, a chronic inflammatory disorder of the gastrointestinal tract, is primarily based on a combination of clinical symptoms, endoscopic findings, radiological imaging, and histopathological examination of biopsy samples. According to the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5), the following criteria are considered for the diagnosis of Crohn’s disease:
Characteristic Symptoms: The DSM-5 criteria require the presence of characteristic symptoms of Crohn’s disease, including abdominal pain, diarrhea, rectal bleeding, weight loss, fatigue, and fever. These symptoms may vary in severity and duration and may fluctuate over time, often leading to impairment of quality of life.
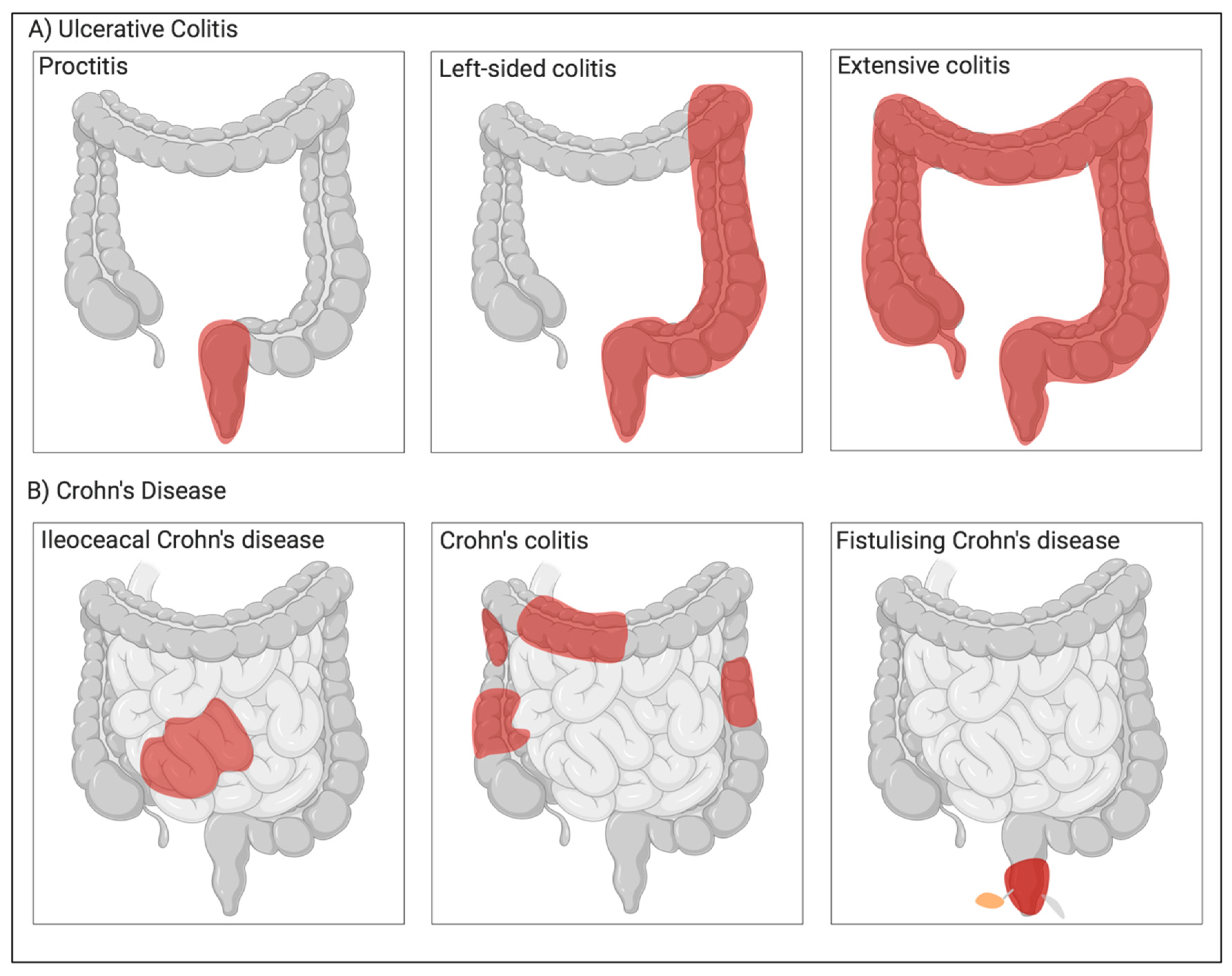
Endoscopic Findings: Endoscopic evaluation of the gastrointestinal tract is essential for diagnosing Crohn’s disease. Endoscopic findings typically include mucosal inflammation, ulceration, and skip lesions affecting various segments of the intestine. These findings are indicative of chronic inflammation and are consistent with the diagnosis of Crohn’s disease.
Radiological Imaging: Radiological imaging studies, such as computed tomography (CT) scans, magnetic resonance imaging (MRI), and small bowel series, are often used to assess the extent and severity of Crohn’s disease. Radiological findings may include bowel wall thickening, strictures, fistulas, abscesses, and mesenteric lymphadenopathy, providing additional evidence supporting the diagnosis.
Histopathological Examination: Histopathological examination of biopsy samples obtained during endoscopy is crucial for confirming the diagnosis of Crohn’s disease. Histological features of Crohn’s disease include transmural inflammation, granulomas, crypt distortion, and architectural distortion of the intestinal mucosa. These histopathological changes are characteristic of Crohn’s disease and help differentiate it from other gastrointestinal disorders.
Exclusion of Other Conditions: The DSM-5 criteria also emphasize the importance of excluding other conditions that may mimic the symptoms of Crohn’s disease, such as ulcerative colitis, infectious colitis, celiac disease, and gastrointestinal malignancies. A comprehensive evaluation, including laboratory tests, imaging studies, and endoscopic evaluation, is necessary to rule out alternative diagnoses.
The DSM-5 diagnosis of Crohn’s disease requires the presence of characteristic symptoms, supported by endoscopic, radiological, and histopathological findings, and the exclusion of other gastrointestinal disorders. A multidisciplinary approach involving gastroenterologists, radiologists, pathologists, and other healthcare providers is essential for accurate diagnosis and optimal management of Crohn’s disease. (Nursing paper Example on Crohn’s Disease: A Comprehensive Overview)
Treatment Regimens and Patient Education for Crohn’s Disease
Effective management of Crohn’s disease requires a comprehensive approach that includes medical therapy, dietary modifications, lifestyle changes, and patient education. The goals of treatment are to induce and maintain remission, alleviate symptoms, prevent complications, and improve the overall quality of life for patients with Crohn’s disease.
Medical Therapy: Medical therapy for Crohn’s disease aims to control inflammation, suppress the immune response, and alleviate symptoms. The choice of medication depends on the severity and location of the disease, as well as individual patient factors. Commonly used medications include:
- Anti-inflammatory Drugs: Aminosalicylates such as mesalamine and sulfasalazine are often used to reduce inflammation in the gastrointestinal tract, particularly in mild to moderate cases of Crohn’s disease affecting the colon and rectum.
- Corticosteroids: Corticosteroids such as prednisone and budesonide are used to rapidly control inflammation and relieve symptoms during flare-ups of Crohn’s disease. However, long-term use is associated with significant side effects and is generally avoided.
- Immunosuppressants: Thiopurines (azathioprine, 6-mercaptopurine) and methotrexate are immunosuppressive medications used to suppress the abnormal immune response in Crohn’s disease and maintain remission.
- Biologic Therapies: Biologic agents such as tumor necrosis factor-alpha (TNF-α) inhibitors (infliximab, adalimumab, certolizumab) and other targeted therapies (vedolizumab, ustekinumab) are used for moderate to severe cases of Crohn’s disease that are refractory to conventional treatments. These medications target specific molecules involved in the inflammatory process, providing effective disease control.
- Antibiotics: Antibiotics such as metronidazole and ciprofloxacin may be used to treat bacterial overgrowth and perianal complications in Crohn’s disease.
Surgical Intervention: In some cases, surgical intervention may be necessary to manage complications of Crohn’s disease, such as strictures, fistulas, abscesses, and bowel obstructions. Surgical options include strictureplasty, bowel resection, fistulotomy, and ostomy formation.
Dietary Modifications: Dietary modifications can help alleviate symptoms and improve nutritional status in patients with Crohn’s disease. While there is no one-size-fits-all diet for Crohn’s disease, some general dietary recommendations include:
- Avoiding trigger foods that worsen symptoms, such as high-fiber foods, dairy products, spicy foods, and caffeine.
- Following a low-residue diet during flare-ups, consisting of easily digestible foods such as cooked vegetables, lean proteins, and refined grains.
- Incorporating anti-inflammatory foods rich in omega-3 fatty acids, antioxidants, and probiotics, such as fatty fish, fruits, vegetables, and fermented foods.
Lifestyle Changes: Lifestyle modifications can also help manage Crohn’s disease and improve overall well-being. Patients are encouraged to:
- Quit smoking, as smoking can worsen symptoms and disease outcomes in Crohn’s disease.
- Engage in regular physical activity to improve digestion, reduce stress, and maintain overall health.
- Practice stress management techniques such as yoga, meditation, and deep breathing exercises to alleviate stress, which can exacerbate symptoms of Crohn’s disease.
Patient Education: Patient education is essential for empowering patients to actively participate in the management of their Crohn’s disease. Key aspects of patient education include:
- Understanding the nature of Crohn’s disease, including its chronicity, variability in symptoms, and potential complications.
- Recognizing and monitoring symptoms of Crohn’s disease, such as abdominal pain, diarrhea, rectal bleeding, and weight loss.
- Adhering to prescribed medication regimens, including proper dosing, timing, and potential side effects.
- Following dietary recommendations tailored to individual needs and preferences, with guidance from healthcare providers or registered dietitians.
- Engaging in regular monitoring and follow-up with healthcare providers to assess disease activity, adjust treatment plans, and address any concerns or questions.
Effective management of Crohn’s disease requires a multidisciplinary approach that includes medical therapy, dietary modifications, lifestyle changes, and patient education. By addressing the complex needs of patients with Crohn’s disease, healthcare providers can optimize treatment outcomes and improve the overall quality of life for individuals living with this chronic condition.



