Assignment Help on Hiatal Hernia: Understanding a Common Gastrointestinal Disorder
/in Assignment Help, Assignment Help Nursing, BLOG, Homework Help, Nursing Exam Help, Nursing Paper Help, Solved Nursing Essays /by Aimee GraceAssignment Help on Hiatal Hernia: Understanding a Common Gastrointestinal Disorder
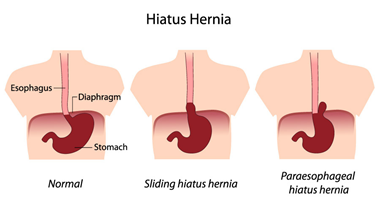
A hiatal hernia, a prevalent gastrointestinal condition, occurs when a portion of the stomach protrudes through the diaphragm into the chest cavity. Despite its frequency, understanding of this disorder remains essential due to its potential to cause discomfort and complications. This paper aims to explore the causes, signs and symptoms, etiology, pathophysiology, DSM-5 diagnosis, treatment regimens, and patient education associated with hiatal hernias. By delving into these aspects, we can gain insight into the nature of this condition and its management. Through a clear understanding of hiatal hernias, individuals affected by this disorder and healthcare professionals can make informed decisions regarding treatment and care. As we delve deeper into the complexities of hiatal hernias, we aim to shed light on this common yet often misunderstood gastrointestinal ailment. (Assignment Help on Hiatal Hernia: Understanding a Common Gastrointestinal Disorder)

Causes
Several factors contribute to the development of hiatal hernias, although the precise cause may not always be evident. Understanding these contributing factors is crucial for managing and preventing the condition.
One primary cause of hiatal hernias is age-related changes in the body. As individuals age, the muscles and tissues that support the diaphragm and surrounding structures may weaken, making it easier for the stomach to protrude through the diaphragmatic opening known as the hiatus. This weakening of muscle tone is a natural part of the aging process and can predispose older adults to hiatal hernias.
Obesity also plays a significant role in the development of hiatal hernias. Excess weight puts increased pressure on the abdomen, which can lead to the displacement of the stomach through the diaphragm. The accumulation of visceral fat in the abdominal cavity exacerbates this pressure, further contributing to the risk of hiatal hernias in obese individuals.
Additionally, lifestyle factors such as smoking and poor dietary habits can contribute to the development of hiatal hernias. Smoking weakens the lower esophageal sphincter (LES), the muscle responsible for preventing stomach acid from refluxing into the esophagus. This weakening of the LES can increase the likelihood of acid reflux and subsequently contribute to the development of hiatal hernias.
Furthermore, frequent heavy lifting or straining during bowel movements can increase intra-abdominal pressure, potentially leading to the protrusion of the stomach through the diaphragm. Chronic coughing or vomiting can also exert pressure on the abdomen, further predisposing individuals to hiatal hernias.
Certain medical conditions, such as congenital abnormalities of the diaphragm or connective tissue disorders like Ehlers-Danlos syndrome, may predispose individuals to hiatal hernias. These underlying conditions can weaken the structural integrity of the diaphragm or abdominal wall, making it easier for the stomach to herniate into the chest cavity.
The causes of hiatal hernias are multifactorial and often involve a combination of age-related changes, obesity, lifestyle factors, and underlying medical conditions. Understanding these contributing factors is essential for both preventing the development of hiatal hernias and managing existing cases effectively. (Assignment Help on Hiatal Hernia: Understanding a Common Gastrointestinal Disorder)
Signs and Symptoms
Hiatal hernias can manifest with a variety of signs and symptoms, although some individuals may remain asymptomatic. Understanding the typical presentation of this condition is essential for prompt diagnosis and management.
One of the most common symptoms associated with hiatal hernias is heartburn, also known as acid indigestion. Heartburn is characterized by a burning sensation in the chest, often occurring after meals or when lying down. This symptom arises due to the reflux of stomach acid into the esophagus, leading to irritation and inflammation of the esophageal lining.
Chest pain or discomfort may also occur in individuals with hiatal hernias. This pain is typically felt in the upper abdomen or chest area and can be mistaken for symptoms of a heart attack. The chest pain associated with hiatal hernias is often exacerbated by bending over, lying down, or eating large meals.
Difficulty swallowing, or dysphagia, is another common symptom of hiatal hernias. Individuals may experience a sensation of food getting stuck in the throat or chest while swallowing, which can be distressing and lead to decreased food intake.
Regurgitation of food or stomach contents is also a hallmark symptom of hiatal hernias. This occurs when stomach acid and undigested food reflux back into the esophagus, leading to a sour or bitter taste in the mouth. Regurgitation may occur spontaneously or be triggered by certain movements or positions.
Other less common symptoms of hiatal hernias include nausea, belching, bloating, and a feeling of fullness in the upper abdomen. These symptoms may vary in severity and frequency among affected individuals.
It is important to note that some individuals with hiatal hernias may be asymptomatic and only discover the condition incidentally during diagnostic imaging studies for unrelated reasons. Asymptomatic hiatal hernias may not require treatment unless they lead to complications or worsen over time.
The signs and symptoms of hiatal hernias can vary widely among individuals but often include heartburn, chest pain, difficulty swallowing, regurgitation of food, and other gastrointestinal discomfort. Recognizing these symptoms is crucial for timely diagnosis and appropriate management of this common gastrointestinal condition. (Assignment Help on Hiatal Hernia: Understanding a Common Gastrointestinal Disorder)
Etiology
The etiology of hiatal hernias involves a combination of anatomical and physiological factors that contribute to the weakening of the diaphragmatic hiatus and subsequent herniation of the stomach into the chest cavity.
One of the primary contributors to the development of hiatal hernias is age-related changes in the body. As individuals age, the integrity of the diaphragmatic hiatus and the surrounding supportive structures may weaken. This weakening can result from the natural degeneration of connective tissues and muscles, making it easier for the stomach to protrude through the diaphragm.
Obesity is another significant etiological factor in the development of hiatal hernias. Excess adipose tissue in the abdominal region increases intra-abdominal pressure, which can force the stomach upward through the weakened diaphragmatic hiatus. The accumulation of visceral fat further exacerbates this pressure, predisposing obese individuals to hiatal hernias.
Chronic conditions that increase intra-abdominal pressure, such as persistent coughing, frequent heavy lifting, or straining during bowel movements, can also contribute to the development of hiatal hernias. These activities exert stress on the abdominal wall and diaphragm, potentially leading to the displacement of the stomach into the chest cavity.
Additionally, certain lifestyle factors and habits can weaken the lower esophageal sphincter (LES), the muscular ring that normally prevents stomach acid from refluxing into the esophagus. Smoking, excessive alcohol consumption, and poor dietary habits can all contribute to the relaxation or weakening of the LES, increasing the risk of acid reflux and subsequent hiatal hernias.
Genetic predisposition may also play a role in the etiology of hiatal hernias. Individuals with a family history of hiatal hernias or connective tissue disorders may be more susceptible to developing this condition due to inherited anatomical variations or weaknesses in the diaphragmatic hiatus.
The etiology of hiatal hernias involves a complex interplay of age-related changes, obesity, chronic conditions affecting intra-abdominal pressure, lifestyle factors, and genetic predisposition. Understanding these underlying factors is essential for identifying individuals at risk and implementing appropriate preventive measures. (Assignment Help on Hiatal Hernia: Understanding a Common Gastrointestinal Disorder)
Pathophysiology
The pathophysiology of hiatal hernias involves the disruption of normal anatomical structures and physiological processes within the gastrointestinal tract, leading to symptoms and complications associated with this condition.
The primary abnormality in hiatal hernias is the displacement of the stomach through the diaphragmatic hiatus into the chest cavity. This herniation occurs when the natural anatomical barrier provided by the diaphragm is weakened or compromised, allowing a portion of the stomach to protrude upward.
As a result of this displacement, the normal anatomical relationship between the esophagus and the stomach is altered. The lower esophageal sphincter (LES), a muscular ring located at the junction of the esophagus and stomach, may become displaced or stretched due to the upward movement of the stomach. This displacement can impair the function of the LES, leading to relaxation or incompetence of the sphincter.
The weakening of the LES contributes to the pathogenesis of gastroesophageal reflux disease (GERD), a common complication of hiatal hernias. In individuals with hiatal hernias, the displaced stomach is more prone to reflux of acidic gastric contents into the esophagus. This reflux of stomach acid irritates the esophageal mucosa, leading to symptoms such as heartburn, chest pain, and regurgitation.
Furthermore, the herniation of the stomach through the diaphragm can disrupt the normal anatomy of the gastroesophageal junction. This disruption may result in the formation of a hernia sac, which can trap portions of the stomach or other abdominal organs within the chest cavity. In severe cases, this hernia sac can become incarcerated or strangulated, leading to complications such as obstruction or ischemia of the trapped organs.
Chronic inflammation and irritation of the esophageal mucosa due to acid reflux can also predispose individuals with hiatal hernias to complications such as esophagitis, Barrett’s esophagus, and esophageal strictures.
The pathophysiology of hiatal hernias involves the displacement of the stomach through the diaphragmatic hiatus, disruption of the normal anatomical relationship between the esophagus and stomach, impairment of LES function, and increased susceptibility to GERD and its associated complications. Understanding these underlying pathophysiological mechanisms is crucial for the management and treatment of hiatal hernias. (Assignment Help on Hiatal Hernia: Understanding a Common Gastrointestinal Disorder)
DSM-5 Diagnosis
The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5), published by the American Psychiatric Association, does not include specific diagnostic criteria for hiatal hernias as it primarily focuses on mental health disorders. However, hiatal hernias are diagnosed through clinical evaluation and diagnostic imaging studies rather than through psychiatric assessment.
Diagnosing hiatal hernias typically involves a comprehensive medical history and physical examination. Healthcare providers will inquire about the patient’s symptoms, including heartburn, chest pain, difficulty swallowing, and regurgitation of food, as well as any risk factors or underlying conditions that may predispose them to hiatal hernias.
Diagnostic imaging studies such as upper gastrointestinal (GI) endoscopy, barium swallow radiography, and esophageal pH monitoring may be utilized to confirm the presence of a hiatal hernia and assess its severity. Upper GI endoscopy allows direct visualization of the esophagus, stomach, and diaphragmatic hiatus, enabling healthcare providers to identify any anatomical abnormalities or herniation of the stomach. Barium swallow radiography involves swallowing a contrast dye that coats the esophagus and stomach, which can highlight the presence of a hiatal hernia on X-ray images. Esophageal pH monitoring measures the acidity levels in the esophagus over some time, which can help diagnose gastroesophageal reflux disease (GERD) associated with hiatal hernias.
While the DSM-5 does not provide specific diagnostic criteria for hiatal hernias, healthcare providers need to consider this condition in patients presenting with gastrointestinal symptoms suggestive of a hiatal hernia. Prompt and accurate diagnosis allows for appropriate management and treatment of hiatal hernias to alleviate symptoms and prevent complications associated with this common gastrointestinal disorder.
While the DSM-5 does not include specific diagnostic criteria for hiatal hernias, healthcare providers diagnose this condition through clinical evaluation and diagnostic imaging studies such as upper GI endoscopy, barium swallow radiography, and esophageal pH monitoring. Recognition of gastrointestinal symptoms and risk factors associated with hiatal hernias is crucial for accurate diagnosis and management of this condition. (Assignment Help on Hiatal Hernia: Understanding a Common Gastrointestinal Disorder)
Treatment Regimens and Patient Education
Treatment for hiatal hernias aims to alleviate symptoms, prevent complications, and improve the overall quality of life for affected individuals. Management strategies often include lifestyle modifications, medications, and, in some cases, surgical intervention. Patient education plays a crucial role in empowering individuals to manage their condition effectively.
Lifestyle Modifications:
Dietary Changes: Patients with hiatal hernias are advised to avoid foods and beverages that can exacerbate symptoms, such as spicy foods, caffeine, alcohol, and acidic foods. Smaller, more frequent meals are recommended to reduce the likelihood of gastric reflux.
Weight Management: Maintaining a healthy weight through diet and regular exercise can help reduce intra-abdominal pressure and alleviate symptoms associated with hiatal hernias. Obesity is a significant risk factor for the development and progression of hiatal hernias.
Posture and Positioning: Patients should avoid lying down or bending over immediately after meals, as these positions can increase the risk of acid reflux and discomfort. Elevating the head of the bed while sleeping can also help reduce nighttime reflux symptoms.
Medications:
Antacids and Acid Suppressants: Over-the-counter antacids or prescription medications that reduce gastric acid production, such as proton pump inhibitors (PPIs) or H2-receptor antagonists, may be prescribed to alleviate heartburn and acid reflux symptoms.
Prokinetic Agents: Medications that enhance gastrointestinal motility, such as prokinetic agents, may be recommended to improve esophageal clearance and reduce the risk of acid reflux.
Surgical Intervention:
Fundoplication: In severe cases of hiatal hernias associated with persistent symptoms despite conservative management, surgical intervention may be considered. Fundoplication is a surgical procedure that involves wrapping the upper portion of the stomach around the lower esophagus to reinforce the lower esophageal sphincter and prevent acid reflux.
Patient Education:
Understanding the Condition: Patients should be educated about the anatomy and pathophysiology of hiatal hernias, as well as the factors that contribute to symptom exacerbation.
Medication Adherence: Patients should understand the importance of adhering to prescribed medications and following dosage instructions to effectively manage symptoms and prevent complications.
Lifestyle Modifications: Educating patients about dietary changes, weight management, and proper posture can empower them to make informed decisions and actively participate in their treatment regimen.
Monitoring and Follow-up: Patients should be encouraged to monitor their symptoms and report any changes or worsening of symptoms to their healthcare provider. Regular follow-up appointments are essential for evaluating treatment efficacy and adjusting management strategies as needed.
The treatment of hiatal hernias encompasses lifestyle modifications, medications, and, in some cases, surgical intervention. Patient education is integral to ensuring adherence to treatment regimens, promoting self-management, and optimizing outcomes for individuals affected by this common gastrointestinal disorder. (Assignment Help on Hiatal Hernia: Understanding a Common Gastrointestinal Disorder)
Conclusion
Hiatal hernias are common gastrointestinal disorders characterized by the protrusion of the stomach through the diaphragm into the chest cavity. Through exploration of its causes, signs and symptoms, etiology, pathophysiology, DSM-5 diagnosis, treatment regimens, and patient education, we gain valuable insight into the complexities of this condition. By incorporating lifestyle modifications, medications, and, when necessary, surgical intervention, individuals with hiatal hernias can effectively manage symptoms and prevent complications. Patient education plays a pivotal role in empowering individuals to make informed decisions regarding their treatment and lifestyle choices. Through understanding and adherence to recommended management strategies, patients can improve their quality of life and mitigate the impact of hiatal hernias on their daily activities and overall well-being. (Assignment Help on Hiatal Hernia: Understanding a Common Gastrointestinal Disorder)



