Nursing Paper Help Example on Parkinson’s Disease: Unraveling the Enigma
/in Assignment Help, Assignment Help Nursing, BLOG, Homework Help, Nursing Exam Help, Nursing Paper Help, Solved Nursing Essays /by Aimee GraceNursing Paper Help Example on Parkinson’s Disease: Unraveling the Enigma
Parkinson’s Disease (PD) stands as a prevalent neurological ailment, affecting millions worldwide. Beyond its physical manifestations, PD poses significant emotional and social challenges for patients and their families. Understanding the intricacies of this condition is pivotal for effective management and support. Despite its prevalence, Parkinson’s remains a complex puzzle with many unanswered questions. Unraveling its mysteries requires a holistic approach that encompasses various facets of the disease. From its causes to its impact on daily life, exploring Parkinson’s from different angles is essential for providing comprehensive care. This essay aims to delve into the causes, signs, symptoms, etiology, pathophysiology, diagnosis criteria, treatment options, and patient education, and conclude with insights into the ongoing efforts to address this challenging neurological disorder. Through increased understanding and tailored interventions, we can strive to improve the lives of those affected by Parkinson’s Disease. (Nursing Paper Help Example on Parkinson’s Disease: Unraveling the Enigma)

Causes
Parkinson’s Disease (PD) is a complex condition influenced by a combination of genetic predisposition and environmental factors. While specific genetic mutations like SNCA and LRRK2 have been identified as contributing to susceptibility, they account for a small fraction of cases. Environmental factors, such as exposure to toxins like pesticides or traumatic head injuries, also play a role in increasing the risk of developing PD. Additionally, advancing age is a significant factor, with the prevalence of PD rising sharply in individuals over 60 years old.
Genetic factors contribute to the hereditary form of PD, accounting for approximately 5-10% of cases. Mutations in genes related to alpha-synuclein (SNCA), parkin (PARK2), PTEN-induced putative kinase 1 (PINK1), DJ-1 (PARK7), and leucine-rich repeat kinase 2 (LRRK2) have been implicated in familial cases of PD. These genetic mutations disrupt various cellular processes, including protein degradation pathways and mitochondrial function, leading to the degeneration of dopaminergic neurons in the brain.
Environmental factors also play a significant role in the development of PD. Exposure to certain toxins, such as pesticides and herbicides, has been linked to an increased risk of PD. Additionally, traumatic head injuries, particularly those resulting in loss of consciousness, have been associated with an elevated risk of developing PD later in life.
The interaction between genetic susceptibility and environmental factors is complex and not yet fully understood. Emerging research suggests that environmental toxins may trigger or accelerate the progression of PD in individuals with genetic predispositions. However, the precise mechanisms underlying this interaction remain an area of active investigation.
Overall, Parkinson’s Disease is a multifactorial condition influenced by a combination of genetic and environmental factors. Understanding these causes is essential for elucidating the underlying mechanisms of the disease and developing targeted interventions for prevention and treatment.
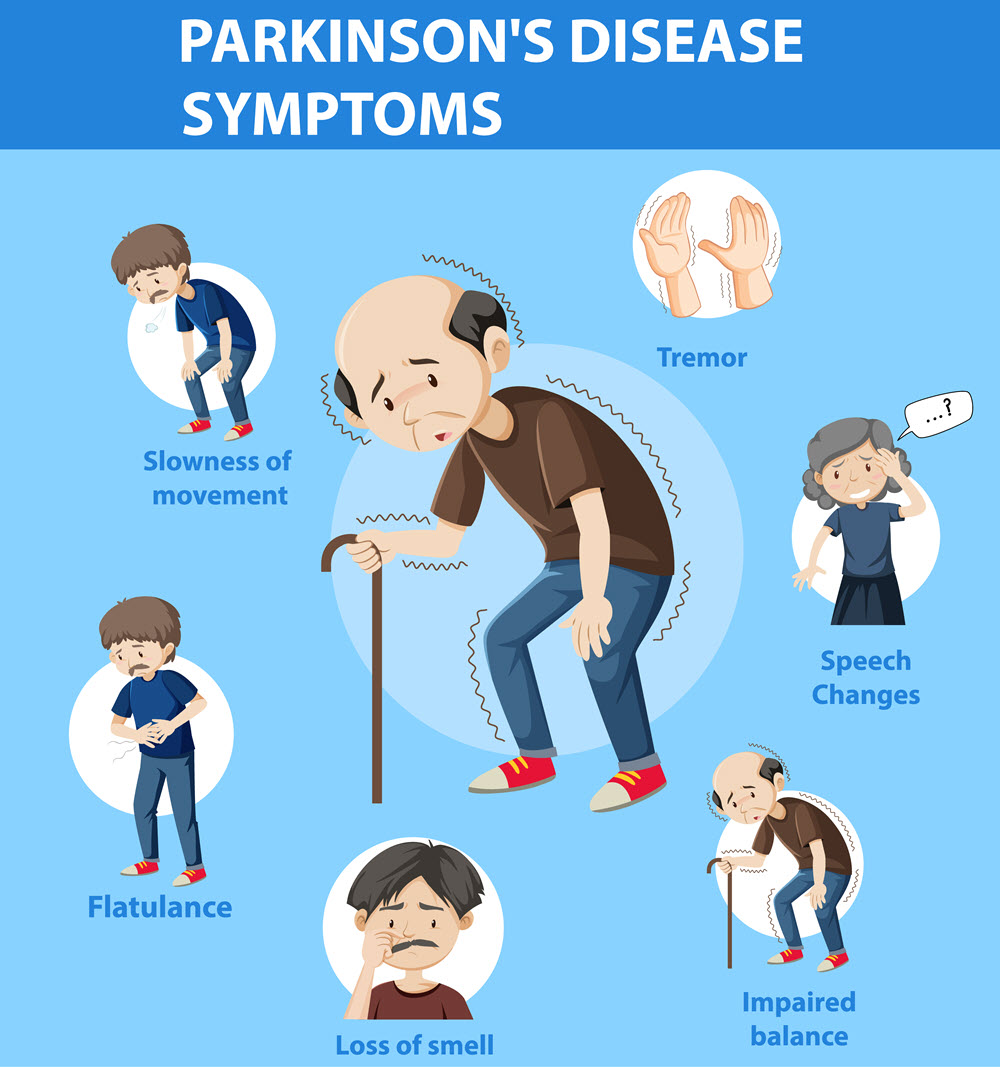
Signs and Symptoms
Parkinson’s Disease (PD) presents a diverse array of symptoms that can vary in severity and progression among individuals. The cardinal motor symptoms of PD include tremors, bradykinesia (slowness of movement), rigidity, and postural instability. Tremors, often described as rhythmic shaking, typically begin in the hands or fingers at rest and may progress to involve other parts of the body, such as the legs or jaw.
Bradykinesia manifests as a general slowness of movement, making simple tasks like buttoning a shirt or walking challenging. Patients may experience difficulty initiating movements, known as akinesia, or “freezing” episodes, where they suddenly stop moving mid-action. Rigidity refers to increased muscle stiffness, causing a sensation of stiffness or resistance to movement, particularly in the arms, legs, neck, or trunk.
Postural instability becomes prominent as PD progresses, leading to impaired balance and coordination. Patients may have difficulty maintaining an upright posture and are at an increased risk of falls, which can result in injuries.
In addition to motor symptoms, Parkinson’s Disease also presents a range of non-motor symptoms that significantly impact patients’ quality of life. These include mood disturbances such as depression and anxiety, sleep disturbances such as insomnia or excessive daytime sleepiness, and cognitive impairments such as slowed thinking, memory problems, and executive dysfunction.
Other non-motor symptoms may include autonomic dysfunction, such as constipation, urinary urgency, and orthostatic hypotension, as well as sensory symptoms like pain or altered sense of smell. Psychiatric symptoms such as hallucinations or delusions may also occur, particularly in the later stages of the disease.
The combination and severity of symptoms can vary widely among individuals with Parkinson’s Disease, making diagnosis and management challenging. Early recognition and comprehensive assessment of both motor and non-motor symptoms are essential for timely intervention and optimal care. Addressing these symptoms through a multidisciplinary approach can help improve patients’ overall well-being and quality of life. (Nursing Paper Help Example on Parkinson’s Disease: Unraveling the Enigma)
Etiology
Parkinson’s Disease (PD) is characterized by the progressive degeneration of dopaminergic neurons in the substantia nigra region of the brain. While the exact etiology of PD remains elusive, research suggests a multifactorial interplay of genetic, environmental, and biochemical factors.
Genetic factors contribute to the development of PD, with several gene mutations identified in familial cases. Mutations in genes such as alpha-synuclein (SNCA), parkin (PARK2), PTEN-induced putative kinase 1 (PINK1), DJ-1 (PARK7), and leucine-rich repeat kinase 2 (LRRK2) have been associated with an increased risk of PD. These genetic mutations disrupt various cellular processes, including protein degradation pathways and mitochondrial function, leading to neuronal dysfunction and degeneration.
Environmental factors also play a role in the etiology of PD. Exposure to certain toxins and chemicals, such as pesticides, herbicides, and heavy metals, has been linked to an elevated risk of developing PD. Additionally, traumatic head injuries, particularly those resulting in loss of consciousness, have been associated with an increased risk of PD later in life.
Biochemical abnormalities, including oxidative stress, mitochondrial dysfunction, and inflammation, are thought to contribute to the pathogenesis of PD. Oxidative stress, resulting from an imbalance between the production of reactive oxygen species and antioxidant defenses, can damage cellular components and contribute to neuronal degeneration. Mitochondrial dysfunction, characterized by impaired energy production and increased oxidative stress, further exacerbates neuronal vulnerability in PD. Inflammation, involving the activation of microglia and the release of pro-inflammatory cytokines, contributes to neuroinflammation and neuronal damage in PD.
The complex interplay of genetic, environmental, and biochemical factors underscores the heterogeneous nature of PD. Understanding the etiological factors involved in PD is crucial for elucidating its underlying mechanisms and developing targeted interventions for prevention and treatment. Further research into the intricate interactions between these factors may provide valuable insights into the pathogenesis of PD and guide the development of novel therapeutic strategies. (Nursing Paper Help Example on Parkinson’s Disease: Unraveling the Enigma)
Pathophysiology
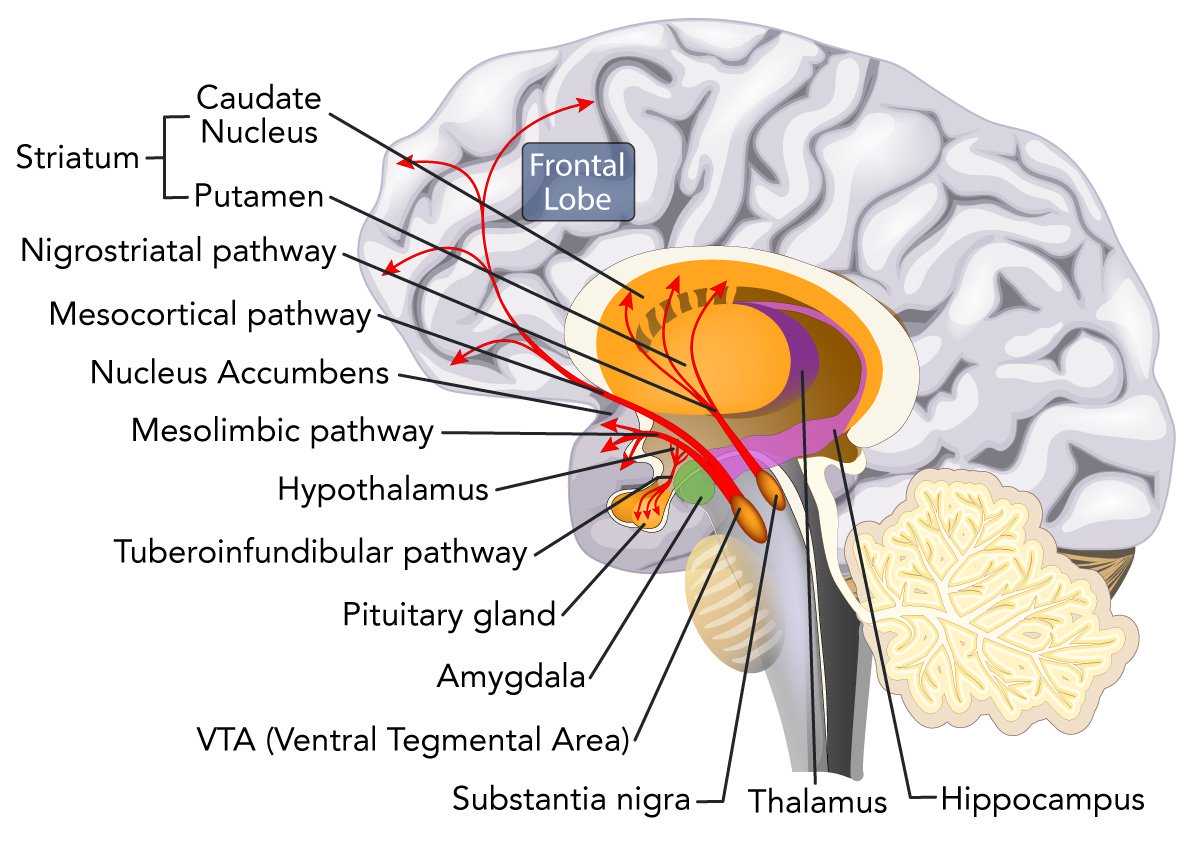
Parkinson’s Disease (PD) is characterized by the progressive degeneration of dopaminergic neurons in the substantia nigra pars compacta region of the brain. The hallmark pathological feature of PD is the formation of intracellular protein aggregates called Lewy bodies, primarily composed of misfolded alpha-synuclein protein. These Lewy bodies disrupt cellular function and contribute to neuronal dysfunction and death in PD.
The degeneration of dopaminergic neurons leads to a depletion of dopamine, a neurotransmitter involved in regulating movement and coordination. The loss of dopamine in the basal ganglia, particularly in the nigrostriatal pathway, results in impaired motor control and the characteristic motor symptoms of PD, including tremors, bradykinesia, rigidity, and postural instability.
In addition to dopaminergic dysfunction, PD is associated with alterations in other neurotransmitter systems, including cholinergic and noradrenergic pathways. Imbalances in these neurotransmitter systems contribute to non-motor symptoms such as cognitive impairment, autonomic dysfunction, and psychiatric symptoms in PD.
Oxidative stress plays a crucial role in the pathophysiology of PD, contributing to neuronal damage and death. Reactive oxygen species generated during normal cellular metabolism can overwhelm antioxidant defenses, leading to oxidative damage to cellular components such as lipids, proteins, and DNA. Oxidative stress further exacerbates mitochondrial dysfunction, impairing energy production and increasing neuronal vulnerability in PD.
Neuroinflammation also plays a significant role in the pathophysiology of PD. Activation of microglia, the resident immune cells of the central nervous system, and the release of pro-inflammatory cytokines contribute to neuroinflammation and neuronal damage in PD. Chronic neuroinflammation further amplifies oxidative stress and exacerbates neurodegeneration in PD.
The pathophysiology of PD is complex and multifaceted, involving a combination of dopaminergic dysfunction, protein aggregation, oxidative stress, mitochondrial dysfunction, and neuroinflammation. Understanding the underlying mechanisms of PD is crucial for developing targeted therapeutic strategies aimed at slowing or halting disease progression and improving outcomes for individuals affected by this debilitating neurological disorder. (Nursing Paper Help Example on Parkinson’s Disease: Unraveling the Enigma)
DSM-5 Diagnosis
The diagnosis of Parkinson’s Disease (PD) is primarily clinical and based on the presence of specific motor symptoms outlined in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5). According to DSM-5 criteria, the diagnosis of PD requires the presence of at least two of the following motor symptoms: tremors at rest, bradykinesia, and rigidity. These motor symptoms must be persistent and not attributed to other medical conditions or medication effects.
Tremor at rest is characterized by rhythmic shaking of the hands, fingers, or other body parts, typically occurring when the affected limb is at rest and diminishing with voluntary movement. Bradykinesia refers to slowness of movement and difficulty initiating and executing voluntary movements, leading to a generalized reduction in spontaneous movement. Rigidity is defined as increased resistance to passive movement of the limbs, resulting in stiffness or inflexibility of muscles.
In addition to motor symptoms, the diagnosis of PD may also involve the assessment of non-motor symptoms, such as cognitive impairment, autonomic dysfunction, and psychiatric symptoms. However, these non-motor symptoms are not included in the DSM-5 criteria for PD diagnosis.
Diagnostic confirmation of PD may require additional investigations, including neuroimaging studies such as magnetic resonance imaging (MRI) or dopamine transporter (DAT) imaging using single-photon emission computed tomography (SPECT) or positron emission tomography (PET). These imaging modalities can help differentiate PD from other Parkinsonian syndromes and provide supportive evidence for the diagnosis.
It is important to note that the diagnosis of PD is based on clinical judgment and may require ongoing assessment and monitoring to confirm and refine the diagnosis over time. Collaborative evaluation by a multidisciplinary team, including neurologists, movement disorder specialists, and neuropsychologists, can aid in the accurate diagnosis and management of PD, ensuring optimal care for individuals affected by this complex neurological disorder. (Nursing Paper Help Example on Parkinson’s Disease: Unraveling the Enigma)
Treatment Regimens and Patient Education
The management of Parkinson’s Disease (PD) requires a comprehensive approach that addresses both motor and non-motor symptoms, focusing on symptom relief, functional improvement, and enhancing patients’ overall quality of life. Treatment regimens for PD typically include pharmacological interventions, non-pharmacological therapies, and patient education.
Pharmacological interventions form the cornerstone of PD management, aimed at replenishing dopamine levels in the brain and alleviating motor symptoms. Levodopa, a precursor to dopamine, is the most effective medication for PD and is often combined with carbidopa to enhance its efficacy and reduce side effects. Dopamine agonists, such as pramipexole and ropinirole, mimic the action of dopamine and can be used as monotherapy or in combination with levodopa. Monoamine oxidase-B (MAO-B) inhibitors, such as rasagiline and selegiline, inhibit the breakdown of dopamine and can help prolong the effects of levodopa.
In addition to pharmacotherapy, non-pharmacological therapies play a crucial role in managing PD symptoms and improving patients’ functional status. Physical therapy focuses on maintaining mobility, flexibility, and balance, while occupational therapy helps patients adapt to daily activities and tasks. Speech therapy can address speech and swallowing difficulties commonly seen in PD, while cognitive rehabilitation may benefit patients with cognitive impairment. Deep brain stimulation (DBS) surgery is a surgical intervention that can help alleviate motor symptoms in advanced PD by delivering electrical stimulation to specific brain regions involved in motor control.
Patient education is essential in empowering individuals with PD and their caregivers to actively participate in disease management and optimize treatment outcomes. Education about medication adherence, including proper dosing schedules and potential side effects, is crucial for optimizing medication efficacy and minimizing complications. Patients should also be educated about lifestyle modifications, including regular exercise, a healthy diet, and stress management, which can help improve motor function and overall well-being.
Furthermore, patients and caregivers should be educated about symptom recognition and management strategies for both motor and non-motor symptoms. This includes recognizing “off” periods, when medication effectiveness wears off and symptoms return, and implementing strategies to minimize their impact. Additionally, patients should be educated about resources and support services available in their community, including support groups, counseling services, and caregiver support programs.
In conclusion, the management of Parkinson’s Disease requires a multidisciplinary approach that incorporates pharmacological and non-pharmacological interventions, along with patient education and support. By addressing motor and non-motor symptoms comprehensively and empowering patients and caregivers with knowledge and resources, it is possible to improve outcomes and enhance the quality of life for individuals living with PD. (Nursing Paper Help Example on Parkinson’s Disease: Unraveling the Enigma)
Conclusion
Parkinson’s Disease (PD) presents a complex challenge, necessitating a multifaceted approach to management. By exploring its causes, signs, symptoms, etiology, pathophysiology, diagnostic criteria, treatment options, and patient education, this essay has provided a comprehensive overview of PD. The emphasis on genetic, environmental, and biochemical factors in the etiology and pathophysiology sheds light on the intricate mechanisms underlying PD. Additionally, the inclusion of DSM-5 diagnostic criteria highlights the importance of accurate diagnosis in guiding treatment decisions. Treatment regimens, incorporating pharmacological and non-pharmacological interventions, alongside patient education, are essential for optimizing outcomes and enhancing the quality of life for individuals with PD. Despite the challenges posed by PD, ongoing research and collaborative efforts offer hope for improved management strategies and better outcomes, underscoring the importance of a holistic approach in addressing this enigmatic neurological disorder. (Nursing Paper Help Example on Parkinson’s Disease: Unraveling the Enigma)



