Nursing Paper Example on Endometriosis: Understanding a Common yet Misunderstood Condition
Nursing Paper Example on Endometriosis: Understanding a Common yet Misunderstood Condition
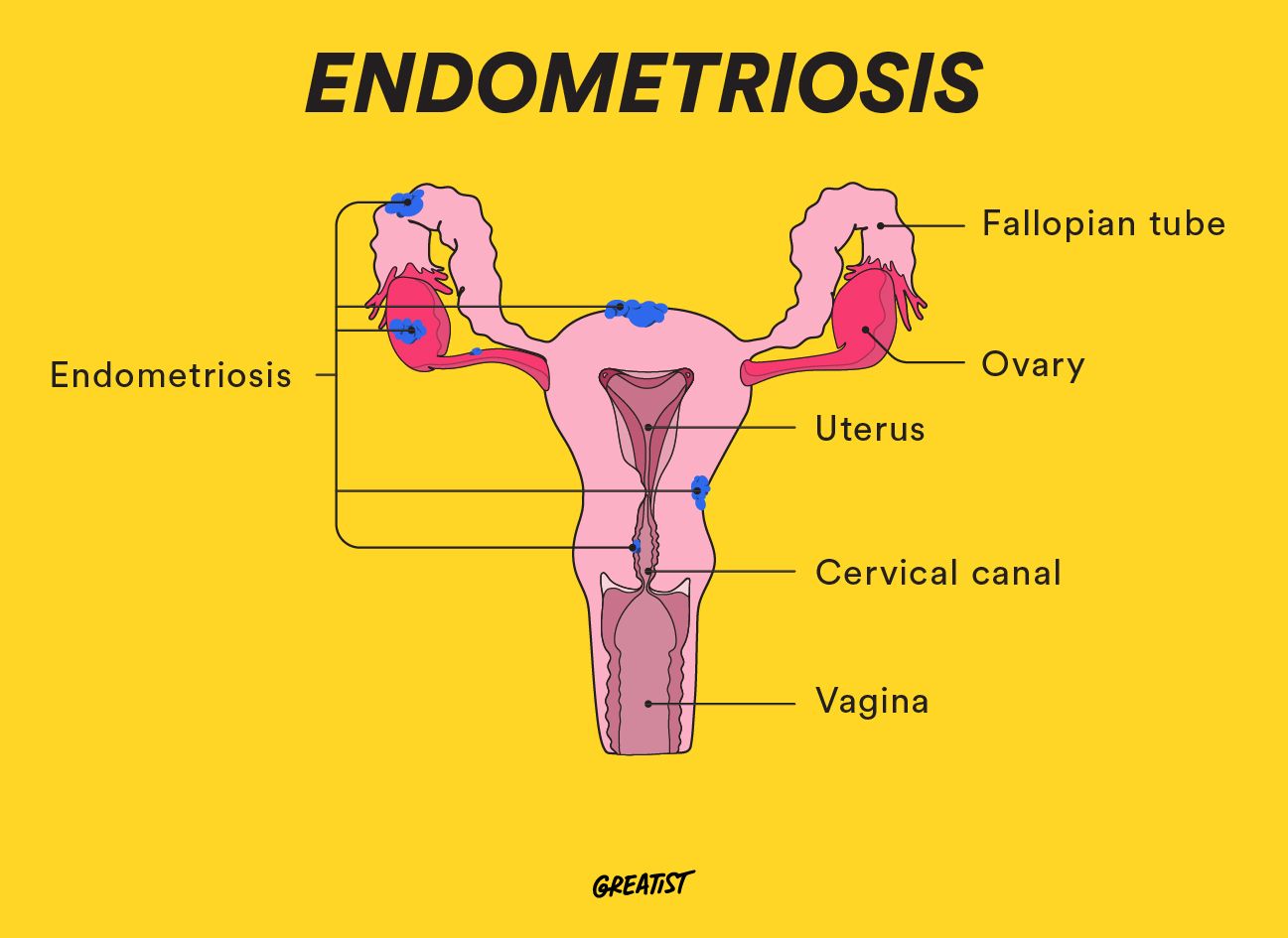
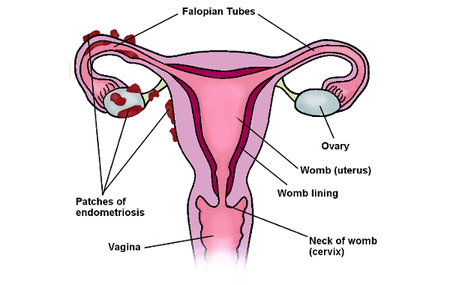
Endometriosis is a chronic gynecological condition affecting millions of individuals worldwide, characterized by the abnormal growth of endometrial-like tissue outside the uterus. Despite its prevalence, endometriosis often goes undiagnosed or misdiagnosed due to a lack of awareness and understanding among healthcare professionals and the general public. This condition can cause debilitating symptoms such as pelvic pain, menstrual irregularities, and infertility, significantly impacting a person’s physical and emotional well-being. Moreover, the societal stigma surrounding menstruation and reproductive health further complicates discussions about endometriosis, leading to delays in seeking medical care and inadequate management of symptoms. Therefore, it is imperative to raise awareness about endometriosis, educate individuals about its signs and symptoms, and advocate for improved access to comprehensive healthcare services. By doing so, we can empower individuals affected by endometriosis to seek timely diagnosis and appropriate treatment, ultimately enhancing their quality of life. (Nursing Paper Example on Endometriosis: Understanding a Common yet Misunderstood Condition)
Causes
Signs and Symptoms
Endometriosis presents with a wide range of signs and symptoms, which can vary in severity and often overlap with other gynecological conditions. The most common symptom is pelvic pain, which may be chronic and debilitating, affecting daily activities and quality of life. This pain is often cyclical, worsening during menstruation, but it can also occur at other times throughout the menstrual cycle.
Menstrual irregularities are also prevalent among individuals with endometriosis. This may include heavy menstrual bleeding, prolonged periods, or irregular menstrual cycles. Some individuals may experience bleeding between periods or spotting, further adding to the complexity of diagnosis.
Pain during intercourse, known as dyspareunia, is another hallmark symptom of endometriosis. This pain can be deep and may persist even after sexual activity has ended, causing emotional distress and impacting intimate relationships.
In addition to pelvic pain and menstrual irregularities, endometriosis can manifest as gastrointestinal symptoms. These may include bloating, constipation, diarrhea, nausea, or rectal pain, particularly during menstruation. These symptoms are often attributed to the presence of endometrial implants on the bowel or rectum, leading to inflammation and irritation.
Infertility is a significant concern for individuals with endometriosis, affecting approximately one-third to one-half of all cases. The presence of endometriosis can interfere with ovulation, fertilization, implantation, and embryo development, making it challenging to achieve pregnancy.
Furthermore, endometriosis can have a profound impact on mental health and overall well-being. Chronic pain, fertility concerns, and the disruptive nature of the condition may lead to feelings of frustration, anxiety, depression, and reduced quality of life.
Recognizing these signs and symptoms is crucial for early diagnosis and intervention, as timely management can alleviate pain, improve fertility outcomes, and enhance overall quality of life for individuals with endometriosis. (Nursing Paper Example on Endometriosis: Understanding a Common yet Misunderstood Condition)
Etiology
Endometriosis is a complex condition with a multifactorial etiology involving genetic, hormonal, immunological, and environmental factors. While the exact cause remains unclear, several theories have been proposed to explain the development of endometriosis.
One prominent theory is retrograde menstruation, where menstrual blood containing endometrial cells flows backward through the fallopian tubes into the pelvic cavity. These displaced endometrial cells then adhere to pelvic organs and tissues, leading to the formation of endometriotic lesions.
Hormonal imbalances, particularly estrogen dominance, play a crucial role in the pathogenesis of endometriosis. Estrogen promotes the growth and proliferation of endometrial tissue, contributing to the development and progression of endometriotic lesions. Conversely, progesterone, which typically inhibits endometrial growth, may be insufficient to counteract the effects of estrogen in individuals with endometriosis.
Genetic predisposition also influences the development of endometriosis, with a higher prevalence observed among individuals with a family history of the condition. Specific gene variants related to hormone metabolism, inflammation, and immune response have been implicated in endometriosis susceptibility.
Furthermore, immunological dysfunction may contribute to the establishment and maintenance of endometriotic lesions. In individuals with endometriosis, alterations in immune cell function and cytokine production may impair the immune system’s ability to recognize and eliminate ectopic endometrial tissue, allowing its growth and survival.
Environmental factors, such as exposure to endocrine-disrupting chemicals, may also influence endometriosis risk. These chemicals can interfere with hormonal signaling pathways, potentially exacerbating hormonal imbalances and promoting the development of endometriotic lesions.
Overall, the etiology of endometriosis is likely multifaceted, involving a complex interplay of genetic, hormonal, immunological, and environmental factors. Further research is needed to better understand the underlying mechanisms driving the development and progression of this debilitating condition. (Nursing Paper Example on Endometriosis: Understanding a Common yet Misunderstood Condition)
 Pathophysiology
Pathophysiology
The pathophysiology of endometriosis involves the aberrant growth and function of endometrial-like tissue outside the uterus, leading to inflammation, pain, and tissue damage. This condition is characterized by the presence of endometriotic lesions, which can vary in size, location, and appearance.
Endometriotic lesions typically consist of glands and stroma resembling endometrial tissue, which respond to hormonal fluctuations throughout the menstrual cycle. However, unlike normal endometrial tissue, these lesions are located outside the uterus, commonly found on pelvic organs such as the ovaries, fallopian tubes, pelvic peritoneum, and rectovaginal septum.
During the menstrual cycle, hormonal changes trigger the proliferation and differentiation of endometrial cells within these lesions, leading to the formation of cysts, adhesions, and scar tissue. This cyclical growth and shedding of ectopic endometrial tissue contribute to the inflammatory response and tissue damage associated with endometriosis.
The presence of endometriotic lesions can also disrupt normal anatomical structures and physiological processes within the pelvis. For example, adhesions and scar tissue may distort pelvic anatomy, leading to organ dysfunction, bowel and bladder symptoms, and pelvic pain. Additionally, the inflammatory environment created by endometriotic lesions can promote nerve hypersensitivity, further exacerbating pain perception.
Moreover, endometriosis is associated with alterations in immune function and inflammatory pathways. Dysregulation of immune cell activity, cytokine production, and inflammatory mediators may contribute to the persistence and progression of endometriotic lesions by impairing the immune system’s ability to recognize and eliminate ectopic endometrial tissue.
Overall, the pathophysiology of endometriosis is complex and multifaceted, involving hormonal, inflammatory, and immunological mechanisms that contribute to the development and maintenance of endometriotic lesions and associated symptoms. Understanding these underlying processes is essential for developing targeted treatment strategies and improving outcomes for individuals with endometriosis. (Nursing Paper Example on Endometriosis: Understanding a Common yet Misunderstood Condition)
DMS-5 Diagnosis
The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5), does not specifically provide diagnostic criteria for endometriosis as it primarily focuses on mental health disorders. However, the diagnosis of endometriosis is typically made based on clinical presentation, medical history, physical examination findings, and imaging studies, with laparoscopic surgery often required for definitive confirmation.
The American College of Obstetricians and Gynecologists (ACOG) and the European Society of Human Reproduction and Embryology (ESHRE) have established guidelines for diagnosing endometriosis. According to these guidelines, a thorough medical history should be obtained, including detailed information about menstrual patterns, pelvic pain symptoms, and any associated comorbidities. Additionally, a pelvic examination may reveal tender nodules or masses suggestive of endometriotic lesions.
Imaging studies, such as transvaginal ultrasound or magnetic resonance imaging (MRI), may be used to evaluate pelvic anatomy and detect the presence of endometriotic lesions, although these modalities have limited sensitivity and specificity for diagnosing endometriosis.
In cases where clinical suspicion remains high despite negative imaging findings, laparoscopic surgery may be performed to visualize the pelvic organs and obtain tissue samples for histological examination. The presence of endometriotic lesions, characterized by the presence of endometrial-like tissue outside the uterus, confirms the diagnosis of endometriosis.
Overall, while the DSM-5 does not provide specific diagnostic criteria for endometriosis, healthcare providers use a combination of clinical evaluation, imaging studies, and surgical findings to diagnose this condition accurately. Early recognition and diagnosis are crucial for initiating appropriate management strategies and improving outcomes for individuals with endometriosis. (Nursing Paper Example on Endometriosis: Understanding a Common yet Misunderstood Condition)
Treatment Regimens and Patient Education
Management of endometriosis aims to alleviate symptoms, improve quality of life, and preserve fertility. Treatment regimens often involve a multidisciplinary approach tailored to the individual’s symptoms, severity of disease, and reproductive goals.
- Pain Management: Nonsteroidal anti-inflammatory drugs (NSAIDs) are commonly used to alleviate pelvic pain and discomfort associated with endometriosis. These medications help reduce inflammation and provide symptomatic relief during menstruation and throughout the menstrual cycle.
- Hormonal Therapies: Hormonal therapies are frequently prescribed to suppress menstruation and hormonal fluctuations, thereby inhibiting the growth of endometrial tissue. Options include combined hormonal contraceptives (birth control pills, patches, or vaginal rings), progestins, gonadotropin-releasing hormone (GnRH) agonists, and danazol. These medications can help alleviate pelvic pain, reduce menstrual flow, and improve quality of life.
- Surgical Interventions: Laparoscopic surgery is often recommended for individuals with severe symptoms or fertility concerns. Surgical options include laparoscopic excision or ablation of endometriotic lesions, ovarian cystectomy for endometriomas, and lysis of adhesions to restore pelvic anatomy. In cases where fertility preservation is a priority, conservative surgical approaches may be employed to remove endometriotic lesions while preserving reproductive organs.
- Assisted Reproductive Technologies (ART): For individuals experiencing infertility due to endometriosis, ART procedures such as in vitro fertilization (IVF) may be considered. IVF involves retrieving eggs from the ovaries, fertilizing them with sperm in a laboratory, and transferring the resulting embryos into the uterus for implantation.
- Patient Education: Educating patients about endometriosis is essential for empowering them to participate in their care and make informed decisions about treatment options. Patients should be provided with information about the condition’s etiology, signs and symptoms, diagnostic methods, and available treatment modalities. Additionally, patients should be educated about lifestyle modifications, such as regular exercise, stress management, and dietary changes, which may help alleviate symptoms and improve overall well-being.
Furthermore, patients should be encouraged to maintain open communication with their healthcare providers, report any changes in symptoms promptly, and actively participate in shared decision-making regarding their treatment plan. By fostering patient education and engagement, healthcare providers can support individuals with endometriosis in managing their condition effectively and optimizing their quality of life. (Nursing Paper Example on Endometriosis: Understanding a Common yet Misunderstood Condition)
Conclusion
Endometriosis is a complex gynecological condition characterized by the growth of endometrial-like tissue outside the uterus, leading to chronic pelvic pain, menstrual irregularities, and infertility. While its exact cause remains unclear, factors such as retrograde menstruation, hormonal imbalances, genetic predisposition, and immunological dysfunction contribute to its development. Early recognition and accurate diagnosis of endometriosis are crucial for implementing effective management strategies and improving patient outcomes. Treatment regimens may include pain management with NSAIDs, hormonal therapies to suppress menstruation, surgical interventions to remove endometriotic lesions, and assisted reproductive technologies for infertility. Furthermore, patient education plays a pivotal role in empowering individuals with endometriosis to actively participate in their care and make informed decisions about treatment options. By fostering a multidisciplinary approach and promoting patient-centered care, healthcare providers can better support individuals with endometriosis in managing their condition and enhancing their quality of life. (Nursing Paper Example on Endometriosis: Understanding a Common yet Misunderstood Condition)
References
https://www.ncbi.nlm.nih.gov/books/NBK567777/



