Comprehensive Nursing Paper Example on Anthrax: A Comprehensive Overview
Comprehensive Nursing Paper Example on Anthrax: A Comprehensive Overview
Causes
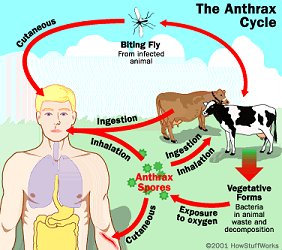
Anthrax is primarily caused by exposure to the bacterium Bacillus anthracis, which commonly affects animals such as cattle, sheep, and goats. Humans typically contract anthrax through direct contact with infected animals or contaminated animal products. The spores of Bacillus anthracis are highly resilient and can remain viable in the environment for decades, making them a persistent threat.
The three primary modes of transmission for anthrax are cutaneous, inhalation, and gastrointestinal.
- Cutaneous Anthrax: This is the most common form of anthrax and occurs when spores enter the body through a break in the skin, such as a cut or abrasion, during contact with infected animals or contaminated animal products. Farmers, veterinarians, and workers in the animal industry are at higher risk of contracting cutaneous anthrax.
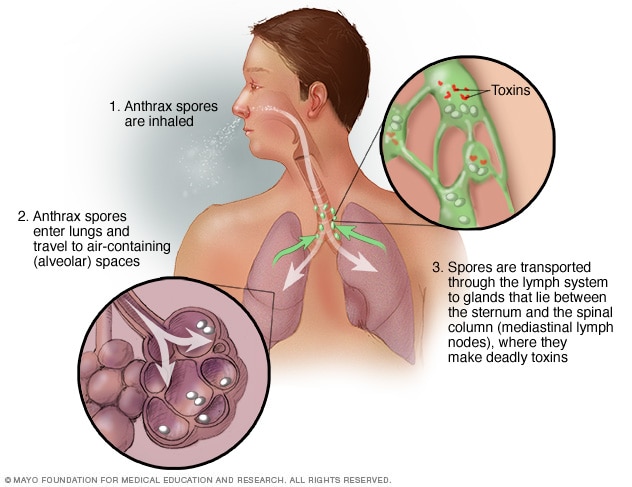
- Inhalation Anthrax: Inhalation anthrax is the most lethal form and occurs when spores are inhaled into the lungs. This usually happens through the inhalation of contaminated dust or aerosols, often during the handling of infected animal hides or through deliberate release as a bioterrorism agent.
- Gastrointestinal Anthrax: This rare form of anthrax occurs when spores are ingested, usually through the consumption of undercooked meat from infected animals. It can result in severe gastrointestinal symptoms such as abdominal pain, vomiting, and diarrhea.
Additionally, anthrax can also be transmitted through injection drug use when heroin or cocaine is contaminated with spores, leading to a rare form known as injection anthrax.
Understanding the various modes of transmission is crucial for implementing preventive measures to reduce the risk of anthrax infection. Public health efforts aimed at monitoring livestock health, ensuring food safety, and educating individuals about proper hygiene practices play a significant role in preventing anthrax outbreaks. (Comprehensive Nursing Paper Example on Anthrax: A Comprehensive Overview)
Signs and Symptoms
Anthrax presents with a range of symptoms that vary depending on the mode of transmission and the severity of the infection. Early recognition of these symptoms is crucial for prompt diagnosis and treatment.
- Cutaneous Anthrax: The most common form of anthrax, cutaneous anthrax, typically begins with the appearance of a small, painless sore or lesion at the site of spore entry, such as a cut or abrasion. This sore may develop into a blister with surrounding swelling and redness. Over time, the blister may ulcerate and form a black eschar, a characteristic hallmark of cutaneous anthrax.
- Inhalation Anthrax: Inhalation anthrax often presents initially with flu-like symptoms, including fever, cough, headache, and fatigue. As the infection progresses, patients may experience severe respiratory distress, chest discomfort, and shortness of breath. Inhalation anthrax can rapidly progress to severe respiratory failure and shock if left untreated.
- Gastrointestinal Anthrax: Symptoms of gastrointestinal anthrax typically manifest within one to seven days after ingestion of contaminated meat. Patients may experience abdominal pain, nausea, vomiting, diarrhea, and fever. Severe cases can lead to gastrointestinal bleeding, septic shock, and death.
- Injection Anthrax: Injection anthrax, although rare, presents similarly to cutaneous anthrax but occurs at the site of injection in individuals who use contaminated drugs. Symptoms include localized swelling, redness, and ulceration at the injection site.
Prompt medical attention is essential if any of these symptoms are present, particularly in areas where anthrax is endemic or in situations where exposure is suspected. Timely diagnosis and appropriate treatment can significantly improve patient outcomes and prevent complications associated with anthrax infection. (Comprehensive Nursing Paper Example on Anthrax: A Comprehensive Overview)
Etiology
The bacterium Bacillus anthracis is the causative agent behind anthrax. This gram-positive, rod-shaped bacterium is capable of forming highly resistant spores, which are the infectious form of the organism. These spores enable Bacillus anthracis to survive harsh environmental conditions, including extremes of temperature, pH, and dehydration, for extended periods, contributing to its persistence in the environment.
The pathogenicity of Bacillus anthracis is attributed to two major virulence factors: the anthrax toxin and the poly-D-glutamic acid capsule.
- Anthrax Toxin: The anthrax toxin is composed of three protein components: protective antigen (PA), lethal factor (LF), and edema factor (EF). PA facilitates the entry of LF and EF into host cells, where they exert their toxic effects. LF disrupts cellular signaling pathways, leading to cell death, while EF disrupts cellular fluid balance, causing edema.
- Poly-D-Glutamic Acid Capsule: Bacillus anthracis is encapsulated by a poly-D-glutamic acid capsule, which protects it from phagocytosis by host immune cells, enabling the bacterium to evade the host immune response and proliferate within the host.
The combination of these virulence factors contributes to the pathogenesis of anthrax by facilitating bacterial survival, dissemination, and host tissue damage.
Factors influencing the severity of anthrax infection include the route and dose of exposure, host immune status, and strain virulence. Inhalation anthrax, for example, is associated with higher mortality rates compared to cutaneous anthrax due to the rapid dissemination of spores within the host and systemic toxin effects.
Understanding the etiology of anthrax is essential for developing effective preventive measures, diagnostic strategies, and therapeutic interventions aimed at controlling the spread of the disease and mitigating its impact on public health. (Comprehensive Nursing Paper Example on Anthrax: A Comprehensive Overview)
Pathophysiology
The pathophysiology of anthrax involves a complex interplay between the bacterium Bacillus anthracis, its virulence factors, and the host immune response.
- Entry and Germination: Anthrax spores enter the body through inhalation, ingestion, or skin abrasions. Once inside the body, spores encounter favorable conditions and germinate into actively growing bacteria.
- Toxin Production: Bacillus anthracis produces two main toxins: the edema toxin and the lethal toxin. These toxins are composed of three proteins: protective antigen (PA), edema factor (EF), and lethal factor (LF). PA binds to host cell receptors, facilitating the entry of EF and LF into the cells.
- Cellular Damage: Once inside the host cells, EF disrupts cellular signaling pathways, leading to an increase in intracellular cyclic AMP (cAMP) levels, which results in edema formation. LF, on the other hand, cleaves specific proteins involved in cell signaling, leading to cell death and tissue damage.
- Immune Evasion: Bacillus anthracis evades the host immune response through various mechanisms. The poly-D-glutamic acid capsule surrounding the bacterium inhibits phagocytosis by immune cells. Additionally, the toxins produced by Bacillus anthracis impair the function of immune cells, further compromising the host’s ability to combat the infection.
- Systemic Effects: As the infection progresses, the toxins produced by Bacillus anthracis disseminate throughout the body, leading to systemic effects such as fever, shock, and organ failure. In inhalation anthrax, the rapid dissemination of toxins via the bloodstream results in severe respiratory distress and ultimately death if untreated.
Understanding the pathophysiology of anthrax is crucial for developing targeted therapeutic interventions aimed at disrupting the bacterial lifecycle and mitigating the deleterious effects of the toxins on the host. (Comprehensive Nursing Paper Example on Anthrax: A Comprehensive Overview)
DSM-5 Diagnosis
Anthrax is not classified in the DSM-5 (Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition) as it is an infectious disease and not a mental health disorder. However, it is essential for healthcare professionals to accurately diagnose and manage anthrax infections to prevent complications and ensure appropriate treatment.
Clinical diagnosis of anthrax typically relies on a combination of patient history, physical examination, and laboratory tests.
- Patient History: Healthcare providers inquire about potential exposure to anthrax, including recent contact with infected animals, contaminated animal products, or suspected bioterrorism incidents. Information regarding travel to endemic regions or occupational exposure is also important.
- Physical Examination: Cutaneous anthrax is characterized by the presence of skin lesions, such as painless ulcers with a characteristic black eschar, at the site of spore entry. Inhalation anthrax may present with respiratory symptoms, including cough, chest discomfort, and difficulty breathing. Gastrointestinal anthrax can manifest as abdominal pain, nausea, vomiting, and diarrhea.
- Laboratory Tests: Diagnostic tests for anthrax include culture and polymerase chain reaction (PCR) assays to detect Bacillus anthracis in clinical specimens such as blood, skin lesions, or respiratory secretions. Serological tests, such as enzyme-linked immunosorbent assay (ELISA), can detect antibodies against Bacillus anthracis antigens.
While not classified in the DSM-5, accurate diagnosis of anthrax is crucial for initiating timely treatment with antibiotics and supportive care. Healthcare providers must remain vigilant for signs and symptoms suggestive of anthrax, particularly in regions where the disease is endemic or during suspected bioterrorism events, to promptly identify and manage cases. (Comprehensive Nursing Paper Example on Anthrax: A Comprehensive Overview)