Nursing Paper example on Appendicitis: Understanding the Causes, Symptoms, Diagnosis, and Treatment
/in Assignment Help, Assignment Help Nursing, BLOG, Homework Help, Nursing Exam Help, Nursing Paper Help, Solved Nursing Essays /by Aimee GraceNursing Paper example on Appendicitis: Understanding the Causes, Symptoms, Diagnosis, and Treatment
Appendicitis, a condition marked by inflammation of the appendix, is a prevalent medical emergency worldwide. The appendix, a small pouch located at the junction of the small and large intestines, serves no apparent function in humans and can become inflamed due to various factors. While the exact cause of appendicitis remains uncertain, it is often linked to blockage of the appendix by fecal matter, foreign bodies, or infection, leading to bacterial overgrowth and subsequent inflammation. This inflammation can result in severe complications if left untreated, including perforation, abscess formation, and potentially life-threatening peritonitis. Recognizing the signs and symptoms of appendicitis is crucial for prompt diagnosis and intervention, as timely surgical removal of the inflamed appendix, known as an appendectomy, is the primary treatment approach. Understanding the causes, symptoms, diagnosis, and treatment of appendicitis is essential for healthcare providers and individuals alike to effectively manage this condition and ensure favorable outcomes. (Nursing Paper example on Appendicitis: Understanding the Causes, Symptoms, Diagnosis, and Treatment)

Causes
Appendicitis can occur due to various factors, but it is commonly associated with obstruction of the appendix. The obstruction can occur for several reasons:
- Fecal Matter Blockage: One of the primary causes of appendicitis is the blockage of the appendix by hardened fecal matter. When feces become trapped within the appendix, it can lead to inflammation and subsequent infection.
- Foreign Bodies: In some cases, foreign bodies such as seeds, fruit pits, or parasites can obstruct the lumen of the appendix, triggering inflammation. These foreign bodies can enter the appendix through ingestion and become lodged within its narrow passageway.
- Infection: Infections within the gastrointestinal tract, such as gastroenteritis or viral infections, can lead to inflammation of the appendix. Bacterial overgrowth and subsequent infection can occur, contributing to the development of appendicitis.
- Lymphoid Hyperplasia: The appendix contains lymphoid tissue that plays a role in the immune system. In conditions such as lymphoid hyperplasia, this tissue can become enlarged, leading to obstruction of the appendix and inflammation.
- Tumors: Rarely, tumors or growths within the abdomen can compress the appendix, causing obstruction and subsequent inflammation. Tumors of the appendix itself, as well as neighboring structures, can contribute to the development of appendicitis.
- Genetic Predisposition: Some individuals may have a genetic predisposition to developing appendicitis. Certain genetic factors may influence the structure or function of the appendix, increasing the likelihood of obstruction and inflammation.
While these factors can contribute to the development of appendicitis, the exact cause may vary from person to person. Understanding these potential causes is essential for identifying individuals at risk and implementing preventive measures to reduce the likelihood of appendicitis. Early recognition of symptoms and timely medical intervention are crucial for preventing complications associated with appendicitis. (Nursing Paper example on Appendicitis: Understanding the Causes, Symptoms, Diagnosis, and Treatment)
Signs and Symptoms
Appendicitis typically presents with a variety of signs and symptoms, which can vary in severity and onset. Recognizing these manifestations is crucial for timely diagnosis and intervention. Common signs and symptoms of appendicitis include:
- Abdominal Pain: The hallmark symptom of appendicitis is abdominal pain, which often begins as a vague discomfort around the belly button before migrating to the lower right side of the abdomen. This pain may start as mild and gradually intensify over time.
- Nausea and Vomiting: Many individuals with appendicitis experience nausea and vomiting, which may occur in conjunction with abdominal pain or independently.
- Loss of Appetite: Appendicitis can lead to a loss of appetite or a decreased desire to eat, often due to the associated abdominal discomfort and nausea.
- Low-Grade Fever: A mild fever is a common symptom of appendicitis, typically accompanying the inflammatory response within the body.
- Localized Tenderness: Upon physical examination, healthcare providers may identify localized tenderness in the right lower quadrant of the abdomen, particularly at McBurney’s point, which is located one-third of the distance from the anterior superior iliac spine to the umbilicus.
- Rebound Tenderness: Rebound tenderness, characterized by increased pain upon the release of pressure after palpation, may also be present in individuals with appendicitis.
- Guarding: Guarding, or involuntary tensing of the abdominal muscles, may occur as a protective response to minimize pain and discomfort.
- Altered Bowel Habits: Some individuals with appendicitis may experience changes in bowel habits, including constipation or diarrhea.
- Pain with Movement: Pain associated with appendicitis may worsen with movement, coughing, or sneezing, reflecting irritation of the inflamed appendix.
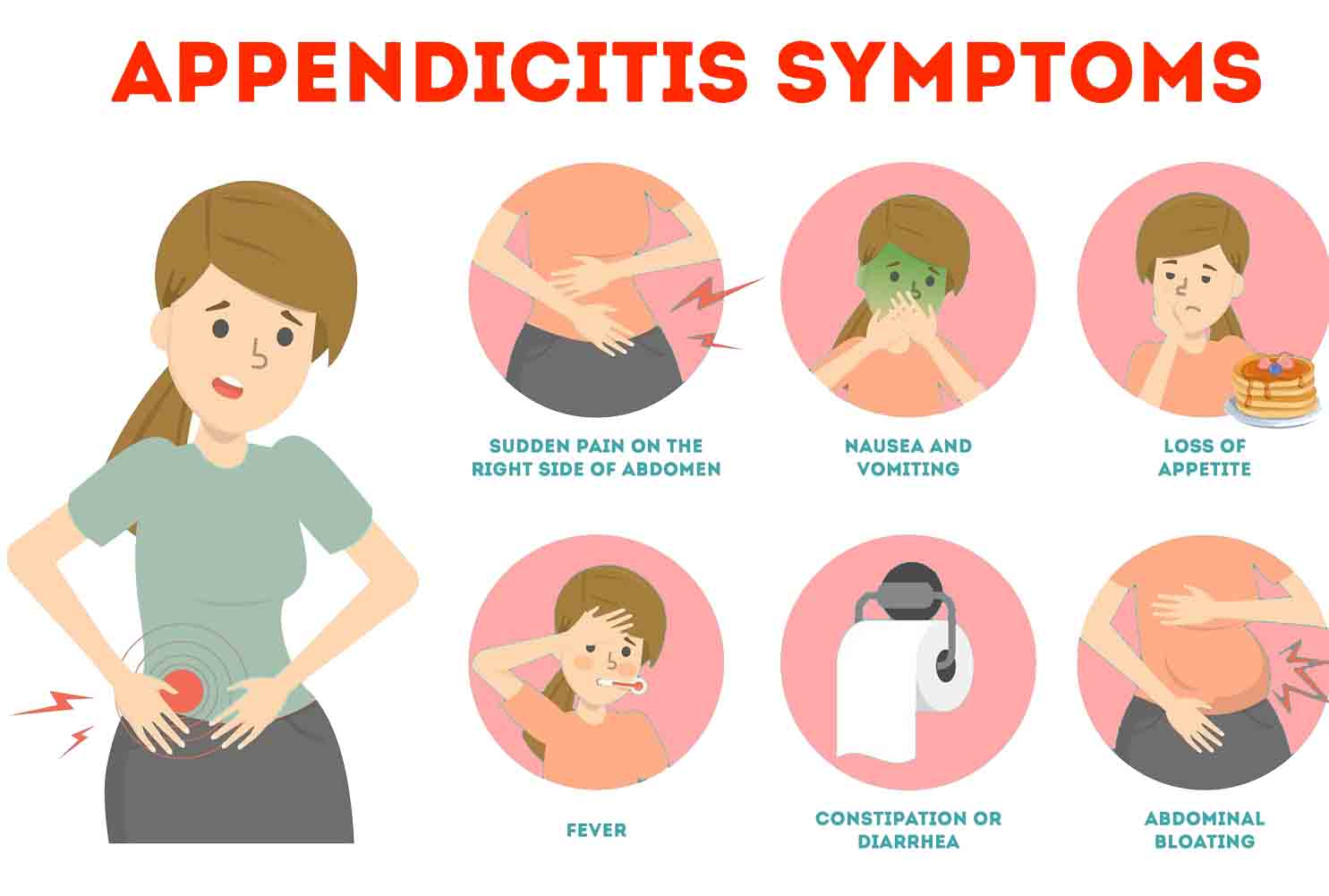
Recognizing these signs and symptoms is essential for prompt medical evaluation and appropriate management of appendicitis to prevent potential complications such as perforation and peritonitis. (Nursing Paper example on Appendicitis: Understanding the Causes, Symptoms, Diagnosis, and Treatment)
Etiology
The development of appendicitis involves a complex interplay of various factors, including genetic predisposition, environmental influences, and anatomical considerations. While the exact etiology of appendicitis may not always be clear, several key factors contribute to its onset:
- Obstruction: The most common cause of appendicitis is obstruction of the appendix, which can occur due to various factors such as hardened fecal matter, foreign bodies, or lymphoid hyperplasia. Obstruction leads to an accumulation of mucus and subsequent inflammation within the appendix.
- Infection: Infections within the gastrointestinal tract, such as viral or bacterial gastroenteritis, can trigger inflammation of the appendix. Bacterial overgrowth within the obstructed appendix can lead to infection and exacerbate the inflammatory response.
- Dietary Factors: Dietary habits may play a role in the development of appendicitis. Diets low in fiber and high in processed foods may increase the risk of constipation, which in turn can contribute to fecal matter accumulation and obstruction of the appendix.
- Genetic Predisposition: Some individuals may have a genetic predisposition to developing appendicitis. Certain genetic factors may influence the structure or function of the appendix, making some individuals more susceptible to obstruction and inflammation.
- Anatomical Considerations: Anatomical variations, such as a narrow or tortuous appendix, may predispose individuals to appendicitis. These variations can increase the likelihood of obstruction and impede the flow of mucus within the appendix.
- Age: Appendicitis can occur at any age but is most common in individuals between the ages of 10 and 30. This age distribution suggests that factors such as lifestyle habits and physiological changes during adolescence may contribute to the development of the condition.
Understanding the multifactorial nature of appendicitis etiology is essential for identifying individuals at risk and implementing preventive measures to reduce the likelihood of appendicitis. By addressing modifiable risk factors and promoting healthy lifestyle habits, healthcare providers can play a crucial role in preventing the onset of this common medical condition. (Nursing Paper example on Appendicitis: Understanding the Causes, Symptoms, Diagnosis, and Treatment)
Pathophysiology
The pathophysiology of appendicitis involves a sequence of events that culminate in inflammation and potential complications of the appendix. Understanding these processes is essential for effective management and prevention of severe outcomes. The pathophysiological cascade of appendicitis typically unfolds as follows:
- Obstruction: The initial event in appendicitis is the obstruction of the appendix, which can occur due to various factors such as fecal matter, foreign bodies, or lymphoid hyperplasia. Obstruction leads to an accumulation of mucus within the appendix, causing distension and increased intraluminal pressure.
- Ischemia and Necrosis: The increased pressure within the obstructed appendix compromises blood flow to the organ, leading to tissue ischemia and necrosis. Ischemia deprives the appendix of oxygen and nutrients, resulting in cellular injury and death.
- Bacterial Proliferation: As the appendix becomes ischemic and necrotic, bacterial proliferation occurs within the organ. Bacteria present in the gastrointestinal tract colonize the obstructed appendix, leading to infection and exacerbation of the inflammatory response.
- Inflammatory Response: The presence of bacteria triggers an inflammatory response within the appendix, characterized by the release of inflammatory mediators such as cytokines and chemokines. This inflammatory cascade leads to tissue edema, vasodilation, and infiltration of immune cells, further exacerbating inflammation.
- Appendiceal Wall Perforation: In severe cases, the combination of increased intraluminal pressure, tissue ischemia, and bacterial infection can lead to perforation of the appendiceal wall. Appendiceal perforation allows the release of infected contents into the abdominal cavity, increasing the risk of complications such as abscess formation and peritonitis.
- Complications: Perforation of the appendix can result in the spread of infection and inflammation throughout the abdomen, leading to complications such as abscess formation, peritonitis, and sepsis.
By understanding the pathophysiological mechanisms underlying appendicitis, healthcare providers can tailor treatment strategies to mitigate inflammation, prevent complications, and promote optimal outcomes for affected individuals. (Nursing Paper example on Appendicitis: Understanding the Causes, Symptoms, Diagnosis, and Treatment)
DSM-5 Diagnosis
The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5), provides criteria for the diagnosis of various mental health disorders, including appendicitis. While appendicitis is not a psychiatric disorder, the DSM-5 includes criteria for medical conditions that may present with psychological symptoms or impact mental health.
The diagnosis of appendicitis is primarily based on clinical presentation, physical examination, and imaging studies. The DSM-5 does not specifically outline criteria for the diagnosis of appendicitis; however, healthcare providers use established medical criteria to assess and diagnose the condition.
Clinical Presentation: Individuals with appendicitis typically present with characteristic signs and symptoms, including abdominal pain, nausea, vomiting, loss of appetite, and low-grade fever. The location and nature of the pain, along with associated symptoms, aid in the clinical assessment of appendicitis.
Physical Examination: Healthcare providers perform a thorough physical examination to assess abdominal tenderness, rebound tenderness, guarding, and other signs indicative of appendicitis. Special attention is paid to McBurney’s point, located in the right lower quadrant of the abdomen, where tenderness may be localized.
Imaging Studies: Imaging studies, such as ultrasound or computed tomography (CT) scans, are often used to confirm the diagnosis of appendicitis and evaluate the severity of inflammation. Imaging findings, such as an enlarged, inflamed appendix or the presence of an appendicolith (calcified deposit), support the diagnosis of appendicitis.
Laboratory Tests: Blood tests, including white blood cell count and C-reactive protein levels, may also aid in the diagnosis of appendicitis by indicating the presence of inflammation.
Overall, the diagnosis of appendicitis is based on a combination of clinical presentation, physical examination findings, and supportive imaging studies. Timely diagnosis and intervention are essential for preventing complications associated with appendicitis and ensuring optimal outcomes for affected individuals. (Nursing Paper example on Appendicitis: Understanding the Causes, Symptoms, Diagnosis, and Treatment)
Treatment Regimens and Patient Education
Treatment regimens for appendicitis typically involve prompt surgical intervention to remove the inflamed appendix, known as an appendectomy. The choice of surgical approach depends on various factors, including the severity of appendicitis and the patient’s overall health status.
Surgical Options:
- Laparoscopic Appendectomy: In uncomplicated cases of appendicitis, laparoscopic appendectomy is often preferred. This minimally invasive procedure involves making small incisions in the abdomen through which specialized surgical instruments and a camera (laparoscope) are inserted. The surgeon removes the inflamed appendix, and the incisions are closed with sutures or surgical staples. Laparoscopic appendectomy typically results in less postoperative pain, shorter hospital stays, and quicker recovery times compared to open surgery.
- Open Appendectomy: In cases of complicated appendicitis, such as perforation or abscess formation, open appendectomy may be necessary. This involves making a larger incision in the abdomen to access the inflamed appendix directly. Open surgery may be preferred when laparoscopic surgery is not feasible or when the surgeon needs better visualization and access to the abdominal cavity.
Postoperative Care:
After surgery, patients are closely monitored for complications and are typically prescribed pain medications and antibiotics to manage pain and prevent infection. Patients are advised to gradually resume normal activities as tolerated and to follow up with their healthcare provider for wound care and postoperative instructions.
Patient Education:
Patient education is an integral component of the management of appendicitis and plays a crucial role in promoting recovery and preventing recurrence. Key aspects of patient education include:
- Recognizing Symptoms: Educating patients about the signs and symptoms of appendicitis, including abdominal pain, nausea, vomiting, and fever, empowers them to seek prompt medical attention if symptoms arise.
- Importance of Timely Intervention: Emphasizing the importance of seeking medical care promptly upon experiencing symptoms of appendicitis can prevent complications such as perforation and peritonitis.
- Postoperative Care: Providing detailed instructions on postoperative care, including wound care, pain management, activity restrictions, and dietary recommendations, facilitates optimal recovery and reduces the risk of complications.
- Follow-up Care: Stressing the importance of attending follow-up appointments with healthcare providers for postoperative evaluation and monitoring ensures continuity of care and early detection of any potential issues.
By educating patients about the signs, symptoms, and management of appendicitis, healthcare providers empower individuals to take an active role in their health and well-being, ultimately improving outcomes and quality of life. (Nursing Paper example on Appendicitis: Understanding the Causes, Symptoms, Diagnosis, and Treatment)
Conclusion
Appendicitis is a common medical condition characterized by inflammation of the appendix, typically requiring prompt surgical intervention for optimal management. Understanding the multifactorial nature of its etiology, which includes factors such as obstruction, infection, genetic predisposition, and anatomical variations, is essential for identifying individuals at risk and implementing preventive measures. Recognizing the signs and symptoms of appendicitis, obtaining a timely diagnosis based on clinical presentation, physical examination, and imaging studies, and undergoing prompt surgical treatment, preferably through laparoscopic appendectomy for uncomplicated cases, are crucial steps in preventing complications and ensuring favorable outcomes. Patient education plays a pivotal role in empowering individuals to recognize symptoms, seek timely medical attention, adhere to postoperative care instructions, and attend follow-up appointments for optimal recovery and long-term health. Through a comprehensive understanding of the causes, symptoms, diagnosis, and treatment of appendicitis, healthcare providers and patients can collaboratively manage this condition and promote overall well-being. (Nursing Paper example on Appendicitis: Understanding the Causes, Symptoms, Diagnosis, and Treatment)



