Nursing Paper Example on Aseptic Meningitis: Understanding Causes, Symptoms, Diagnosis, and Treatment
/in Assignment Help, Assignment Help Nursing, BLOG, Homework Help, Nursing Exam Help, Nursing Paper Help, Psychology assignment help, Solved Nursing Essays /by Aimee GraceNursing Paper Example on Aseptic Meningitis: Understanding Causes, Symptoms, Diagnosis, and Treatment
Aseptic meningitis, characterized by inflammation of the meninges without bacterial involvement, poses significant challenges in diagnosis and management. Typically caused by viral infections, this condition manifests with symptoms like fever, headache, and neck stiffness. Understanding its causes, symptoms, and underlying mechanisms is crucial for effective patient care. This paper provides comprehensive insights into aseptic meningitis, aiming to enhance understanding among students and healthcare practitioners. By exploring the diverse etiologies, clinical presentations, pathophysiological mechanisms, and diagnostic criteria of aseptic meningitis, this paper seeks to equip readers with the knowledge necessary to recognize, diagnose, and manage this condition effectively. With a focus on simplicity and clarity, this paper elucidates the complexities of aseptic meningitis, offering a valuable resource for students seeking foundational knowledge in this area and healthcare practitioners striving to deliver high-quality care to patients affected by this condition. (Nursing Paper Example on Aseptic Meningitis: Understanding Causes, Symptoms, Diagnosis, and Treatment)
Causes
Aseptic meningitis, often triggered by viral infections, encompasses a spectrum of causative agents. Enteroviruses, particularly echoviruses and coxsackieviruses, stand out as predominant contributors to this condition. These viruses, ubiquitous in the environment, gain entry through the respiratory or gastrointestinal tract, subsequently disseminating to the central nervous system. Additionally, herpesviruses, including herpes simplex virus (HSV) and varicella-zoster virus (VZV), can precipitate aseptic meningitis, particularly during primary infection or reactivation.
Moreover, mumps virus, typically associated with parotitis, occasionally manifests with aseptic meningitis as a complication. Influenza viruses, notably influenza A and B, also pose a risk, especially during seasonal outbreaks. Beyond viral etiologies, certain medications such as nonsteroidal anti-inflammatory drugs (NSAIDs), antibiotics, and intravenous immunoglobulins (IVIG) have been implicated in drug-induced aseptic meningitis.
Furthermore, autoimmune disorders like systemic lupus erythematosus (SLE) and Behçet’s disease can trigger meningitis through immune-mediated mechanisms. Neoplastic disorders, particularly lymphomas and leukemias, may rarely infiltrate the meninges, causing aseptic meningitis as a paraneoplastic phenomenon.
Environmental factors, including overcrowding and poor sanitation, facilitate viral transmission, contributing to the incidence of aseptic meningitis. Individual susceptibility, influenced by genetic predispositions and immunocompromised states, also plays a pivotal role.
Understanding this diverse array of etiologies is paramount for accurate diagnosis and tailored management strategies. Clinicians must consider the specific infectious or non-infectious triggers, along with patient-specific factors, to formulate an effective approach to mitigating the impact of aseptic meningitis. (Nursing Paper Example on Aseptic Meningitis: Understanding Causes, Symptoms, Diagnosis, and Treatment)
Signs and Symptoms
Aseptic meningitis presents with a constellation of symptoms that overlap with those of bacterial meningitis, making accurate diagnosis challenging. The hallmark features of aseptic meningitis include fever, which is often abrupt in onset and may be accompanied by chills and rigors. Severe headache, typically diffuse and throbbing in nature, is another common symptom experienced by patients with aseptic meningitis.
Neck stiffness, or nuchal rigidity, is a characteristic finding resulting from meningeal irritation. This stiffness limits the patient’s ability to flex the neck forward, leading to discomfort and resistance upon attempted movement. Photophobia, an aversion to light, is frequently reported and contributes to the overall discomfort experienced by patients.
Nausea and vomiting are common gastrointestinal symptoms associated with aseptic meningitis, often attributed to meningeal inflammation and increased intracranial pressure. These symptoms can exacerbate the patient’s overall distress and contribute to dehydration if not adequately managed.
Patients with aseptic meningitis may also exhibit altered mental status, ranging from lethargy and confusion to frank delirium or coma in severe cases. Behavioral changes, including irritability and restlessness, may be observed, particularly in pediatric patients.
Additionally, neurological signs such as focal deficits, seizures, and cranial nerve abnormalities may manifest, depending on the extent of meningeal inflammation and involvement of adjacent structures.
Clinicians must meticulously evaluate these signs and symptoms in the context of the patient’s clinical presentation and medical history to differentiate aseptic meningitis from other conditions, including bacterial meningitis, encephalitis, and non-infectious causes of meningeal irritation. Early recognition and prompt initiation of appropriate treatment are essential for optimizing outcomes and preventing potential complications associated with aseptic meningitis. (Nursing Paper Example on Aseptic Meningitis: Understanding Causes, Symptoms, Diagnosis, and Treatment)
Etiology
The etiology of aseptic meningitis encompasses a diverse range of viral and non-viral factors. Viral infections, particularly those caused by enteroviruses, represent the most common etiological agents. Enteroviruses, including coxsackieviruses and echoviruses, are ubiquitous in the environment and commonly infect individuals through fecal-oral or respiratory routes. Other viral culprits associated with aseptic meningitis include herpesviruses, such as herpes simplex virus (HSV) and varicella-zoster virus (VZV), which can lead to meningitis during primary infection or reactivation.
Non-viral causes of aseptic meningitis include autoimmune disorders, such as systemic lupus erythematosus (SLE) and Behçet’s disease, which trigger meningitis through immune-mediated mechanisms. Certain medications, including nonsteroidal anti-inflammatory drugs (NSAIDs), antibiotics, and intravenous immunoglobulins (IVIG), have also been implicated in drug-induced aseptic meningitis.
Furthermore, neoplastic disorders, particularly lymphomas and leukemias, may infiltrate the meninges, leading to aseptic meningitis as a paraneoplastic phenomenon. Environmental factors, such as overcrowding and poor sanitation, facilitate viral transmission and contribute to the incidence of aseptic meningitis.
Individual susceptibility plays a crucial role in the development of aseptic meningitis, influenced by genetic predispositions and immunocompromised states. Immunocompromised individuals, including those with HIV/AIDS or undergoing immunosuppressive therapy, are at increased risk of developing aseptic meningitis due to impaired immune responses.
Understanding the diverse etiological factors contributing to aseptic meningitis is essential for accurate diagnosis and appropriate management strategies. Clinicians must consider the specific infectious or non-infectious triggers, along with patient-specific factors, to formulate an effective approach to mitigating the impact of aseptic meningitis. (Nursing Paper Example on Aseptic Meningitis: Understanding Causes, Symptoms, Diagnosis, and Treatment)
Pathophysiology
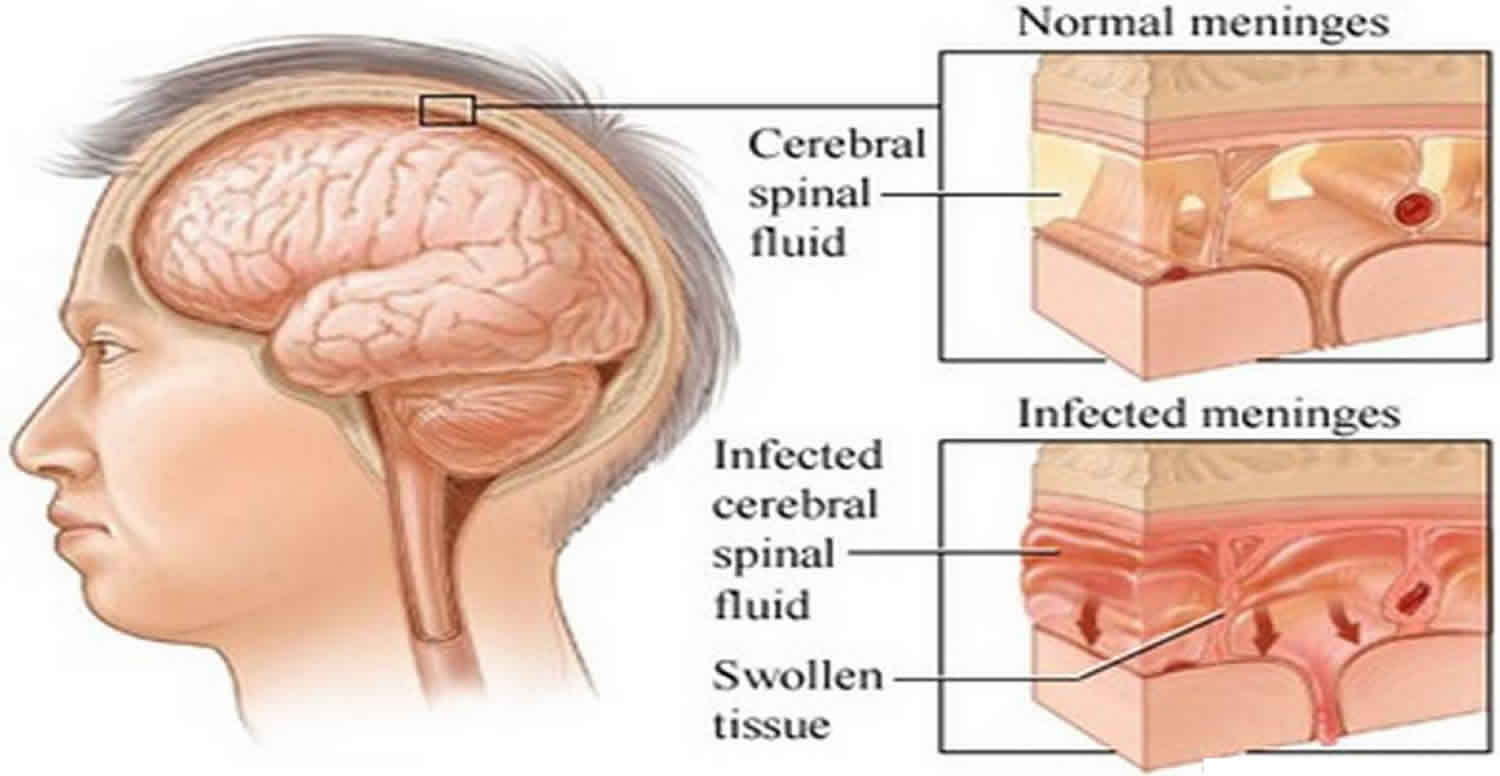
The pathophysiology of aseptic meningitis involves a cascade of inflammatory processes triggered by viral or non-viral etiologies. In viral aseptic meningitis, viral particles gain entry into the central nervous system (CNS) via various routes, including the bloodstream or direct neuronal spread. Once inside the CNS, viral replication occurs, leading to the release of viral antigens and activation of the immune response.
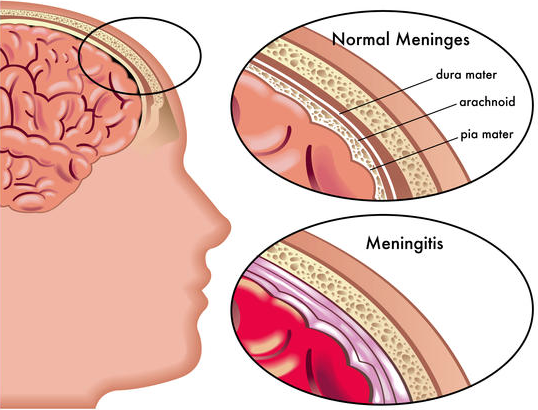
This immune response involves the activation of resident microglia and infiltration of peripheral immune cells, including lymphocytes and monocytes, into the meninges and cerebrospinal fluid (CSF). The release of pro-inflammatory cytokines, such as interleukin-1β (IL-1β) and tumor necrosis factor-alpha (TNF-α), further amplifies the inflammatory cascade, contributing to meningeal inflammation and increased permeability of the blood-brain barrier.
The influx of immune cells and cytokines into the CSF leads to characteristic changes, including elevated white blood cell count (pleocytosis) and increased protein levels, observed in the cerebrospinal fluid analysis of patients with aseptic meningitis. Additionally, disruption of the blood-brain barrier allows for the diffusion of inflammatory mediators and viral particles into the brain parenchyma, contributing to neuronal injury and dysfunction.
Non-viral causes of aseptic meningitis, such as autoimmune disorders and drug-induced reactions, involve immune-mediated mechanisms that result in meningeal inflammation and disruption of normal CNS homeostasis. Autoimmune reactions lead to the production of autoantibodies targeting components of the CNS, while drug-induced reactions may involve direct toxicity or immune-mediated hypersensitivity responses.
Overall, the pathophysiology of aseptic meningitis is characterized by a complex interplay of viral or non-viral triggers, immune-mediated inflammation, and disruption of CNS homeostasis, resulting in the characteristic clinical manifestations observed in affected individuals. Understanding these underlying mechanisms is crucial for guiding therapeutic interventions and preventing complications associated with aseptic meningitis. (Nursing Paper Example on Aseptic Meningitis: Understanding Causes, Symptoms, Diagnosis, and Treatment)
DMS-5 Diagnosis
The diagnosis of aseptic meningitis relies on a combination of clinical evaluation, laboratory tests, and imaging studies, with specific criteria outlined in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DMS-5). According to DMS-5, the presence of characteristic symptoms such as fever, headache, and neck stiffness is essential for diagnosing aseptic meningitis. These symptoms typically manifest acutely and may be accompanied by additional signs such as photophobia, nausea, and altered mental status.
Laboratory tests play a crucial role in confirming the diagnosis of aseptic meningitis. Cerebrospinal fluid (CSF) analysis via lumbar puncture reveals findings consistent with meningeal inflammation, including elevated white blood cell count (pleocytosis), increased protein levels, and normal to mildly elevated glucose levels. Additionally, polymerase chain reaction (PCR) testing of CSF can detect viral nucleic acids, aiding in the identification of specific viral pathogens responsible for aseptic meningitis.
Imaging studies, such as magnetic resonance imaging (MRI) or computed tomography (CT) scans of the brain, may be performed to rule out other neurological conditions or complications associated with aseptic meningitis, such as cerebral edema or hydrocephalus.
The diagnosis of aseptic meningitis requires careful consideration of the patient’s clinical presentation, medical history, and laboratory findings, as well as the exclusion of bacterial meningitis through appropriate diagnostic tests. By adhering to the diagnostic criteria outlined in DMS-5 and utilizing a comprehensive approach to evaluation, healthcare practitioners can accurately diagnose aseptic meningitis and initiate timely management strategies to optimize patient outcomes. (Nursing Paper Example on Aseptic Meningitis: Understanding Causes, Symptoms, Diagnosis, and Treatment)
Treatment Regimens and Patient Education
The management of aseptic meningitis primarily focuses on supportive care, symptom relief, and addressing specific underlying causes if identified. Since aseptic meningitis is often caused by viral infections, treatment is aimed at alleviating symptoms and promoting recovery, as viral infections are typically self-limiting.
Patients diagnosed with aseptic meningitis are advised to get adequate rest and ensure proper hydration. Bed rest is often recommended during the acute phase of the illness to facilitate recovery and reduce the risk of complications. Hydration is crucial to prevent dehydration, especially in cases where patients experience nausea, vomiting, or fever. Encouraging fluid intake, including water, electrolyte solutions, and clear fluids, helps maintain hydration status and supports the body’s immune response.
Over-the-counter medications such as nonsteroidal anti-inflammatory drugs (NSAIDs) or acetaminophen may be used to alleviate fever, headache, and muscle pain. However, caution should be exercised when administering NSAIDs, particularly in patients with underlying renal impairment or gastrointestinal disorders.
In severe cases of aseptic meningitis or when complications arise, hospitalization may be necessary for close monitoring and intravenous administration of fluids and medications. Intravenous fluids help maintain hydration and electrolyte balance, while medications such as antiemetics may be prescribed to alleviate nausea and vomiting.
Patient education plays a crucial role in the management of aseptic meningitis, empowering individuals to actively participate in their care and recovery process. Patients should be informed about the nature of the illness, the expected course of symptoms, and potential complications. Clear instructions regarding medication use, including dosage, frequency, and possible side effects, should be provided to ensure compliance and safety.
Additionally, patients should be educated about the importance of follow-up appointments with healthcare providers to monitor their progress and address any concerns or new symptoms. Prevention strategies, including good hygiene practices such as handwashing and avoiding close contact with individuals who are sick, should also be emphasized to reduce the risk of viral transmission and recurrence of aseptic meningitis.
By providing comprehensive patient education and implementing appropriate treatment regimens, healthcare providers can effectively manage aseptic meningitis, promote symptom relief, and support patients toward optimal recovery. (Nursing Paper Example on Aseptic Meningitis: Understanding Causes, Symptoms, Diagnosis, and Treatment)
Conclusion
Aseptic meningitis presents a complex challenge in diagnosis and management, requiring a thorough understanding of its diverse etiologies, clinical manifestations, and treatment approaches. Through comprehensive insights into the causes, symptoms, pathophysiology, and diagnosis of aseptic meningitis, healthcare practitioners can better navigate the complexities of this condition and provide optimal care for affected individuals. The multifactorial nature of aseptic meningitis, encompassing viral and non-viral triggers, underscores the importance of tailored treatment regimens and patient education to address specific underlying causes and promote symptom relief. By emphasizing supportive care, symptom management, and preventive measures, healthcare providers can empower patients to actively participate in their recovery process and minimize the risk of complications. Through ongoing research and clinical advancements, further improvements in the diagnosis, treatment, and management of aseptic meningitis can be achieved, ultimately enhancing outcomes and reducing the burden of this condition on individuals and healthcare systems alike. (Nursing Paper Example on Aseptic Meningitis: Understanding Causes, Symptoms, Diagnosis, and Treatment)



