Nursing Paper Example on Sciatica
/in Assignment Help, BLOG, Homework Help /by Aimee GraceNursing Paper Example on Sciatica
Causes
Sciatica results from a variety of underlying causes that compress or irritate the sciatic nerve. These include:
- Herniated Discs: This is one of the most common causes. It occurs when one of the intervertebral discs bulges out and puts pressure on the surrounding nerve roots that form the sciatic nerve.
- Spinal Stenosis: This condition involves the narrowing of the spinal canal, which can compress nerves including the sciatic nerve. It is more common in older adults due to degenerative changes in the spine.
- Spondylolisthesis: This occurs when one vertebra slips forward over another, narrowing the space through which the nerve exits the spinal column, leading to sciatic nerve compression.
- Degenerative Disc Disease: Over time, the spinal discs lose their cushioning ability, becoming thinner and less flexible. This can lead to nerve compression and pain.
- Piriformis Syndrome: In some cases, the piriformis muscle, located deep in the buttocks, spasms or tightens, irritating the sciatic nerve. This is less common but still a potential cause.
- Trauma or Injury: Direct trauma to the lower back or buttocks can damage or compress the sciatic nerve, causing pain.
- Pregnancy: During pregnancy, weight gain and changes in posture can cause additional pressure on the lower spine and sciatic nerve.
Certain risk factors like prolonged sitting, diabetes, and obesity can also increase the likelihood of developing sciatica.
(Nursing Paper Example on Sciatica)
Signs and Symptoms
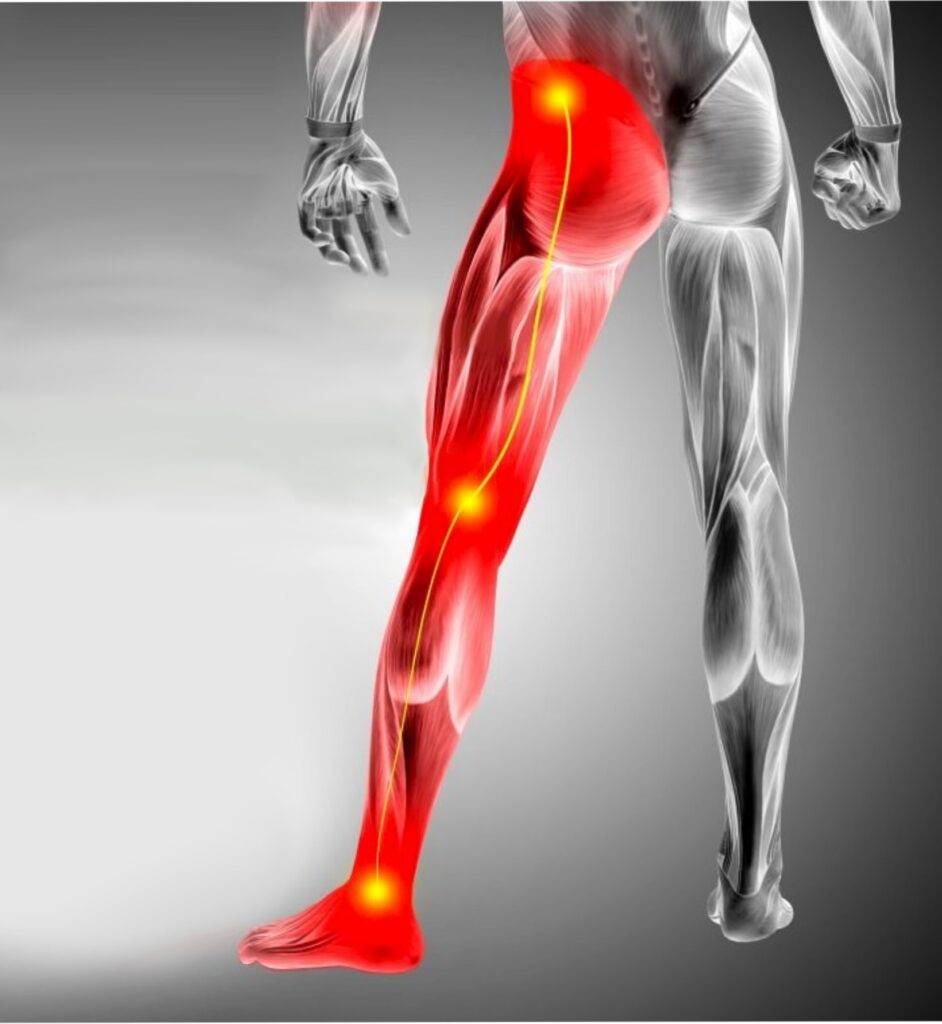
The most defining symptom of sciatica is pain that radiates along the path of the sciatic nerve, from the lower back through the hips and buttocks and down the legs. Other symptoms include:
- Radiating Pain: The pain usually affects only one side of the body and can vary in intensity from a mild ache to sharp, burning sensations or excruciating discomfort. The pain worsens with prolonged sitting or standing, sudden movements, or sneezing and coughing.
- Numbness and Tingling: Some individuals experience numbness, tingling, or “pins and needles” sensations in the leg or foot.
- Muscle Weakness: In more severe cases, the affected leg may feel weak or difficult to move, which can result in difficulty walking or standing.
- Reflex Changes: Diminished reflexes, particularly in the knee or Achilles tendon, may be observed.
Etiology
Sciatica is most commonly caused by structural abnormalities in the spine that lead to nerve compression. Herniated discs are the most frequent etiology, particularly in individuals aged 30-50. However, the etiology can also be multifactorial, particularly in cases related to spinal degeneration in older adults. In younger individuals, sciatica can be associated with lifestyle factors such as poor posture, prolonged sitting, or physically demanding jobs.
(Nursing Paper Example on Sciatica)
Pathophysiology
Sciatica occurs due to irritation or compression of the sciatic nerve, which originates from the L4 to S3 nerve roots in the lower spine. Compression of these nerve roots can result from structural abnormalities like herniated discs or stenosis. This compression leads to nerve inflammation, which in turn causes the pain and neurological symptoms associated with sciatica.
- Mechanical Compression: This is the primary factor in most cases, where a physical structure such as a disc or vertebra puts pressure on the nerve.
- Inflammatory Mediators: Inflammation of the nerve due to irritation from the surrounding structures leads to the release of inflammatory cytokines, which amplify pain and discomfort.
- Neuropathic Pain: Continued compression leads to neuropathic pain, which is often chronic and can be debilitating if not properly managed.
Diagnosis
Diagnosis of sciatica involves a combination of medical history, physical examination, and imaging studies:
- Physical Examination: Clinicians test for signs of sciatic nerve irritation, including the straight leg raise (SLR) test. This test involves raising the affected leg while the patient lies flat; pain produced during this maneuver can suggest nerve root involvement.
- Imaging:
- X-rays are useful for ruling out other causes like fractures or bone abnormalities.
- Magnetic Resonance Imaging (MRI) is the gold standard for diagnosing disc herniation or other soft tissue abnormalities that could be compressing the sciatic nerve.
- CT Scans may also be used, particularly when MRI is contraindicated or unavailable.
- Electromyography (EMG): This test measures the electrical activity of muscles and can indicate the presence of nerve damage.
Early diagnosis is crucial to prevent long-term complications and deterioration.
(Nursing Paper Example on Sciatica)
Treatment Regimens
The management of sciatica depends on the underlying cause and the severity of symptoms. Most cases of sciatica resolve with conservative treatment, though more severe cases may require surgery.
- Conservative Treatment:
- Medications: Nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen or naproxen are often used to reduce inflammation and relieve pain. In more severe cases, muscle relaxants, corticosteroids, or opioid medications may be prescribed.
- Physical Therapy: Physical therapy involves exercises designed to improve flexibility, strengthen the back and core muscles, and relieve pressure on the sciatic nerve. Stretching exercises and techniques such as massage, heat/cold therapy, and electrical stimulation are also employed.
- Lifestyle Modifications: Patients are encouraged to maintain good posture, avoid heavy lifting, and engage in low-impact exercises such as swimming or walking to aid recovery.
- Interventional Treatments:
- Epidural Steroid Injections: These injections deliver anti-inflammatory medication directly to the affected area, helping to reduce inflammation and pain.
- Surgical Options: Surgery is typically considered when conservative treatments fail, or if there is severe nerve damage. Surgical options include:
- Microdiscectomy: The removal of part of a herniated disc that is pressing on the nerve.
- Laminectomy: Removal of part of the vertebral bone (lamina) to widen the spinal canal and relieve pressure on the nerve.
Patient Education
Educating patients on sciatica management is essential in preventing recurrence and ensuring long-term success. Key aspects include:
- Exercise: Patients should be encouraged to engage in regular physical activity, focusing on low-impact exercises like swimming and cycling. Strengthening exercises for the core and back muscles help support the spine.
- Posture and Ergonomics: Patients should be taught how to maintain proper posture while sitting, standing, and lifting heavy objects. Using ergonomic furniture and taking breaks from prolonged sitting are important preventive measures.
- Weight Management: Obesity can place extra strain on the spine, contributing to sciatic nerve compression. Maintaining a healthy weight through diet and exercise is critical.
- Smoking Cessation: Smoking can accelerate spinal degeneration and impair disc health, increasing the risk of sciatica.
Conclusion
Sciatica is a common and often debilitating condition that results from the compression of the sciatic nerve. While conservative treatments such as physical therapy, medications, and lifestyle changes can effectively manage the condition, severe cases may require surgical intervention. Early diagnosis and patient education play a crucial role in improving outcomes and preventing recurrence.
References
Mayo Clinic. (2022). Sciatica: Symptoms and causes. https://www.mayoclinic.org/diseases-conditions/sciatica/symptoms-causes/syc-20377435
National Institute of Neurological Disorders and Stroke (NINDS). (2021). Sciatica fact sheet. https://www.ninds.nih.gov/health-information/disorders/sciatica
Cleveland Clinic. (2020). Sciatica: Symptoms, causes, and treatments. https://my.clevelandclinic.org/health/diseases/12792-sciatica
Johns Hopkins Medicine. (2021). Sciatica. https://www.hopkinsmedicine.org/health/conditions-and-diseases/sciatica



