Nursing Paper Example on Thymoma
Nursing Paper Example on Thymoma
Thymoma is a rare type of tumor originating from the epithelial cells of the thymus gland, which is located in the anterior mediastinum, just behind the sternum. While often slow-growing, thymomas can sometimes be invasive and spread to surrounding tissues. The thymus gland plays a vital role in immune system development, particularly during childhood, as it facilitates the maturation of T-cells, which are essential for adaptive immunity. Thymoma is often associated with autoimmune conditions, particularly myasthenia gravis.
Causes and Risk Factors of Thymoma
The exact causes of thymoma are largely unknown, though certain genetic and environmental factors may contribute. Unlike many cancers, thymoma is not typically linked to lifestyle factors, but it may be associated with some genetic predispositions.
- Autoimmune Diseases: Thymoma is frequently associated with autoimmune diseases, especially myasthenia gravis, a disorder where antibodies attack the neuromuscular junction, leading to muscle weakness. Up to 30-40% of thymoma cases present with myasthenia gravis (National Cancer Institute [NCI], 2022).
- Genetic Factors: Some studies suggest that genetic mutations, particularly in tumor suppressor genes, may play a role in thymoma development, though further research is necessary.
- Age and Gender: Thymoma is more common in adults between 40 and 60 years of age, with no significant gender predilection.
Pathophysiology
Thymoma arises from epithelial cells within the thymus gland. These tumors are generally slow-growing, with some cases remaining confined to the thymus and others invading nearby structures or metastasizing to distant organs.
Classification: Thymomas are categorized into five types (Type A, AB, B1, B2, and B3) based on histological features. Type A thymomas have spindle-shaped cells and are often noninvasive, while Types B1, B2, and B3 exhibit increased lymphocyte infiltration and greater likelihood of invasion (World Health Organization [WHO], 2023).
Immunological Link: The thymus gland’s role in T-cell maturation may explain the association between thymomas and autoimmune conditions. The dysfunction of T-cells in thymoma can result in autoimmunity and explain the coexistence of thymoma with diseases like myasthenia gravis and pure red cell aplasia.
(Nursing Paper Example on Thymoma)
Signs and Symptoms
Thymomas are often asymptomatic in early stages and may be discovered incidentally during imaging for other conditions. However, as the tumor grows, symptoms can appear due to compression of surrounding structures or immunological effects.
- Respiratory Symptoms: Chest pain, shortness of breath, and persistent cough may occur due to compression of the trachea or lungs.
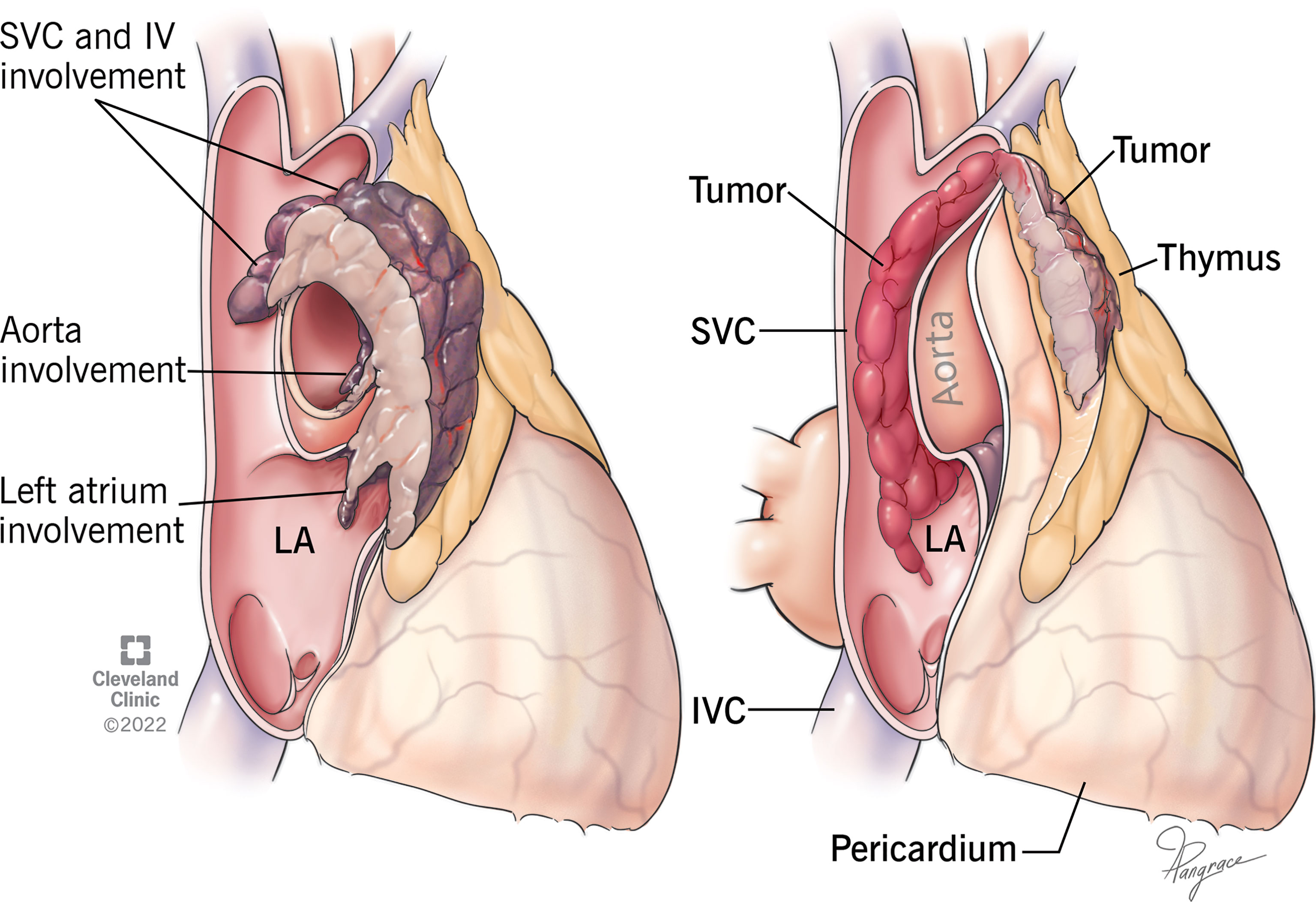
- Superior Vena Cava Syndrome: Tumors that press on the superior vena cava may cause swelling of the face and upper body, along with dilation of veins in the neck and chest.
- Myasthenia Gravis: Patients often present with muscle weakness, especially in the eyes and face, along with fatigue and difficulty swallowing due to myasthenia gravis.
- Other Autoimmune Symptoms: Thymoma patients may experience autoimmune-related symptoms such as anemia and aplastic anemia due to pure red cell aplasia (American Cancer Society [ACS], 2022).
Diagnosis of Thymoma
Diagnosis often requires a combination of imaging studies and histological examination to differentiate thymoma from other anterior mediastinal masses.
- Imaging:
- Chest X-Ray: A thymoma can appear as a mass in the anterior mediastinum on a chest X-ray.
- CT and MRI Scans: These imaging techniques offer greater detail for tumor location and invasion into adjacent structures.
- Biopsy: For a definitive diagnosis, a biopsy is usually required. This can be performed with a needle aspiration or through a surgical procedure to obtain a tissue sample.
- Blood Tests: In cases where myasthenia gravis is suspected, acetylcholine receptor antibodies may be detected in the blood (National Institutes of Health [NIH], 2023).
Treatment Options
Treatment for thymoma varies by tumor stage, with surgery being the most common and effective intervention for localized tumors. Advanced cases may require a multimodal approach.
- Surgery: Surgical resection is the treatment of choice for thymomas that have not spread beyond the thymus. Complete removal improves prognosis and reduces recurrence risk.
- Radiation Therapy: For invasive thymomas or incomplete surgical resection, radiation therapy can help reduce the risk of local recurrence.
- Chemotherapy: In cases where the thymoma has metastasized, chemotherapy may be administered as a primary treatment or in combination with radiation. Drugs like cisplatin and cyclophosphamide are often used.
- Targeted Therapy and Immunotherapy: These emerging treatments are under investigation for thymoma. Research focuses on targeting specific proteins in tumor cells to inhibit growth (World Health Organization [WHO], 2023).
Prognosis and Complications
The prognosis of thymoma largely depends on tumor stage and histological type. Early-stage thymomas have a favorable prognosis, with five-year survival rates over 90% following complete surgical resection.
- Metastasis: Advanced thymomas can invade local tissues and metastasize, reducing prognosis.
- Autoimmune Complications: Untreated thymomas may lead to worsening autoimmune symptoms, particularly myasthenia gravis, affecting quality of life.
- Recurrence: Even after successful surgery, thymomas can recur, especially if invasion was present at the time of initial treatment (American Cancer Society [ACS], 2022).
Prevention and Follow-Up
Currently, there are no specific preventive measures for thymoma due to its unclear etiology. Regular monitoring and follow-up with imaging and clinical evaluations are essential for patients post-treatment to detect any recurrence early.
(Nursing Paper Example on Thymoma)
Conclusion
Thymoma is a rare but potentially complex tumor with a close link to autoimmune diseases, most notably myasthenia gravis. Proper diagnosis, surgical intervention, and appropriate follow-up are crucial for effective management and a positive prognosis. Research into targeted therapies and immunotherapy may provide new avenues for treating advanced thymoma cases, offering hope for improved outcomes.
References
American Cancer Society (ACS). (2022). Thymoma and Thymic Carcinoma. https://www.cancer.org
National Cancer Institute (NCI). (2022). Thymoma and Thymic Carcinoma Treatment (Adult) (PDQ®)–Health Professional Version. https://www.cancer.gov
National Institutes of Health (NIH). (2023). Thymoma and Other Mediastinal Tumors. https://www.nih.gov
World Health Organization (WHO). (2023). Classification of Thymic Epithelial Tumors. https://www.who.int



