Assignment Help Example on Irritable Bowel Syndrome: Understanding a Common Gastrointestinal Disorder
Assignment Help Example on Irritable Bowel Syndrome: Understanding a Common Gastrointestinal Disorder
Introduction
Abnormal Gastrointestinal Motility: One of the primary factors contributing to Irritable Bowel Syndrome (IBS) is abnormal gastrointestinal motility. This refers to irregular contractions of the muscles in the digestive tract, leading to altered bowel habits such as diarrhea, constipation, or a combination of both. These abnormal motility patterns can result in discomfort and pain for individuals with IBS.
Visceral Hypersensitivity: Another significant cause of IBS is visceral hypersensitivity. This condition involves heightened sensitivity to pain and discomfort in the internal organs, particularly the intestines. Even normal contractions or stimuli that would not typically cause discomfort can trigger pain in individuals with visceral hypersensitivity, contributing to the symptoms of IBS.
Altered Gut Microbiota: The gut microbiota, consisting of trillions of microorganisms residing in the gastrointestinal tract, play a crucial role in digestion, immunity, and overall health. Alterations in the composition and balance of these microorganisms can contribute to the development of IBS. Imbalances in gut bacteria may lead to increased inflammation, abnormal fermentation of food, and altered signaling between the gut and the brain, exacerbating symptoms of IBS.
Psychosocial Factors: Psychosocial factors, including stress, anxiety, depression, and traumatic life events, can significantly impact the development and exacerbation of IBS symptoms. Stress, in particular, has been shown to influence gut motility, visceral sensitivity, and the perception of pain in individuals with IBS. Additionally, psychological distress can lead to changes in eating habits, sleep patterns, and coping mechanisms, all of which can contribute to the severity of IBS symptoms.
Genetics: Although the exact genetic mechanisms underlying IBS are not fully understood, there is evidence to suggest that genetics play a role in predisposing individuals to the disorder. Studies have shown that individuals with a family history of IBS are at an increased risk of developing the condition themselves. Genetic variations related to gut motility, visceral sensitivity, and immune function may contribute to the susceptibility to IBS.
Environmental Factors: Environmental factors such as diet, lifestyle, and exposure to toxins or infections can also influence the development and severity of IBS symptoms. Certain foods and beverages, such as spicy foods, caffeine, alcohol, and high-fat foods, may exacerbate symptoms in some individuals. Additionally, gastrointestinal infections, particularly those caused by bacteria or parasites, can trigger the onset of IBS symptoms in susceptible individuals. (Assignment Help Example on Irritable Bowel Syndrome: Understanding a Common Gastrointestinal Disorder)
Signs and Symptoms
Abdominal Pain or Discomfort: The hallmark symptom of Irritable Bowel Syndrome (IBS) is recurrent abdominal pain or discomfort. This pain is often described as cramping, bloating, or aching and can vary in intensity and duration. The location of the pain may also vary, typically occurring in the lower abdomen but sometimes radiating to other areas. The discomfort is often relieved or improved after a bowel movement.
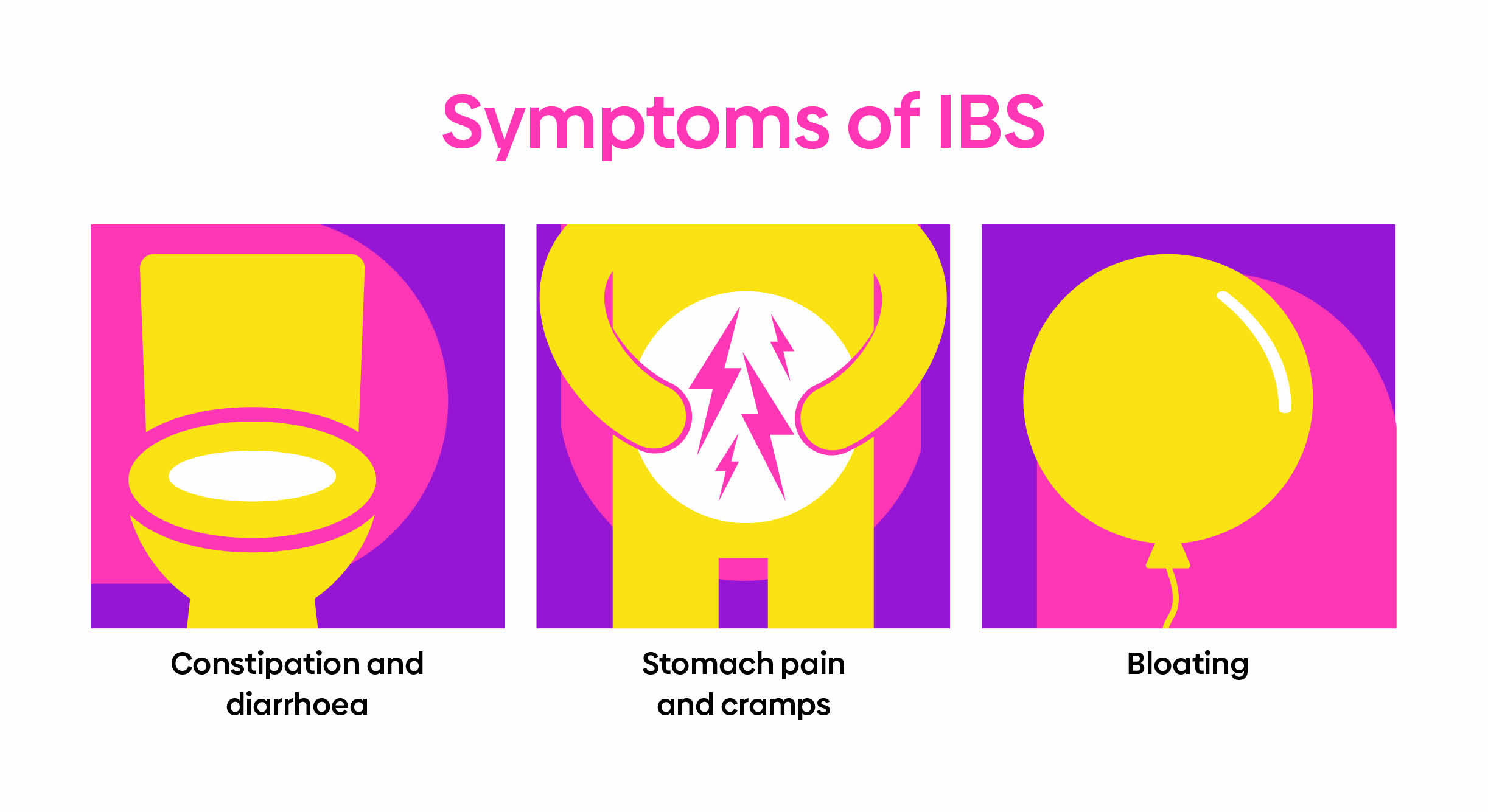
Bloating and Gas: Individuals with IBS frequently experience bloating and excessive gas. Bloating is characterized by a sensation of fullness or tightness in the abdomen, often accompanied by visible distention or swelling. Excessive gas production, leading to flatulence or belching, is also common in IBS and can contribute to discomfort and embarrassment for affected individuals.
Diarrhea: Diarrhea is a common symptom of IBS, particularly in individuals with the diarrhea-predominant subtype (IBS-D). It is characterized by loose or watery stools, increased frequency of bowel movements, and urgency to defecate. Diarrhea in IBS can be unpredictable and may occur in response to certain foods, stress, or hormonal changes.
Constipation: Constipation is another prevalent symptom of IBS, especially in individuals with the constipation-predominant subtype (IBS-C). It is characterized by infrequent bowel movements, difficulty passing stools, and a sensation of incomplete evacuation. Individuals with IBS-C may also experience straining during bowel movements and the passage of hard or lumpy stools.
Altered Bowel Habits: Many individuals with IBS experience alterations in their bowel habits, including changes in stool consistency and frequency. Some may alternate between episodes of diarrhea and constipation, while others may have a mix of both types of bowel movements. These fluctuations in bowel habits can be unpredictable and may impact daily activities and quality of life.
Mucus in Stool: The presence of mucus in the stool is a common symptom of IBS. Mucus is a gel-like substance produced by the intestines to lubricate and protect the gastrointestinal tract. In individuals with IBS, increased mucus production may occur due to inflammation or irritation of the intestines, leading to its presence in the stool. (Assignment Help Example on Irritable Bowel Syndrome: Understanding a Common Gastrointestinal Disorder)
Etiology
The etiology of Irritable Bowel Syndrome (IBS) is multifactorial, involving a complex interplay of various factors including physiological, psychological, genetic, and environmental influences.
Abnormal Gut Motility: One key factor in the etiology of IBS is abnormal gut motility. Dysregulation of the muscular contractions in the gastrointestinal tract can lead to alterations in bowel habits, including diarrhea, constipation, or a combination of both. Abnormal motility patterns may result from disruptions in the coordination of smooth muscle contractions, leading to symptoms of IBS.
Visceral Hypersensitivity: Visceral hypersensitivity, or heightened sensitivity to pain and discomfort in the internal organs, is another significant component of IBS etiology. Individuals with IBS may have a lower threshold for perceiving visceral sensations, leading to increased pain and discomfort in response to normal gut stimuli. This heightened sensitivity can contribute to the severity and frequency of symptoms experienced by individuals with IBS.
Altered Gut Microbiota: Alterations in the composition and balance of the gut microbiota have also been implicated in the etiology of IBS. The gut microbiota play a crucial role in maintaining gut health and function, influencing processes such as digestion, immune regulation, and gut-brain communication. Disruptions in the gut microbiota, such as dysbiosis or imbalances in specific bacterial species, can lead to inflammation, increased intestinal permeability, and abnormal fermentation of food, contributing to the development of IBS symptoms.
Psychosocial Factors: Psychosocial factors, including stress, anxiety, depression, and early-life trauma, are known to influence the development and exacerbation of IBS symptoms. Stress, in particular, has been shown to affect gut motility, visceral sensitivity, and the perception of pain in individuals with IBS. Additionally, psychological distress can lead to maladaptive coping behaviors, changes in eating habits, and alterations in gut function, all of which can contribute to the etiology of IBS.
Genetic Predisposition: While the specific genetic factors contributing to IBS remain unclear, there is evidence to suggest a genetic predisposition to the disorder. Family and twin studies have demonstrated an increased risk of IBS among relatives of affected individuals, suggesting a hereditary component to the etiology of IBS. Genetic variations related to gut motility, visceral sensitivity, immune function, and neurotransmitter pathways may contribute to the susceptibility to IBS.
Environmental Triggers: Environmental factors such as diet, lifestyle, and exposure to infections or toxins can also play a role in the etiology of IBS. Certain dietary factors, including high-fat foods, spicy foods, caffeine, and alcohol, have been implicated in triggering or exacerbating IBS symptoms. Gastrointestinal infections, particularly those caused by bacteria or parasites, can also lead to the development of IBS symptoms in susceptible individuals, potentially through alterations in gut microbiota and immune function. Additionally, stressful life events or changes in routine can trigger symptom flares in individuals with IBS, highlighting the role of environmental triggers in the etiology of the disorder. (Assignment Help Example on Irritable Bowel Syndrome: Understanding a Common Gastrointestinal Disorder)

Pathophysiology
The pathophysiology of Irritable Bowel Syndrome (IBS) involves a complex interplay of physiological, psychological, and environmental factors, leading to alterations in gut function and the perception of pain.
Dysregulated Brain-Gut Axis: Central to the pathophysiology of IBS is the dysregulation of the brain-gut axis, a bidirectional communication network between the central nervous system (CNS) and the gastrointestinal tract. Abnormalities in this axis can lead to alterations in gut motility, visceral sensitivity, and the modulation of pain signals, contributing to the symptoms of IBS. Dysregulated neurotransmitter signaling, including alterations in serotonin, dopamine, and opioid pathways, may play a role in the dysregulation of the brain-gut axis in IBS.
Abnormal Gut Motility: Alterations in gut motility are a hallmark feature of IBS pathophysiology. Dysregulated smooth muscle contractions in the gastrointestinal tract can lead to abnormal motility patterns, including increased or decreased transit times, irregular bowel movements, and altered stool consistency. These abnormal motility patterns contribute to symptoms such as diarrhea, constipation, and abdominal pain in individuals with IBS.
Visceral Hypersensitivity: Visceral hypersensitivity, or heightened sensitivity to pain and discomfort in the internal organs, is another key aspect of IBS pathophysiology. Individuals with IBS may have a lower threshold for perceiving visceral sensations, leading to increased pain and discomfort in response to normal gut stimuli. This visceral hypersensitivity can amplify the perception of pain and discomfort associated with gastrointestinal symptoms, contributing to the severity and frequency of symptoms experienced by individuals with IBS.
Altered Gut Microbiota: Changes in the composition and balance of the gut microbiota have emerged as a significant factor in the pathophysiology of IBS. Disruptions in the gut microbiota, such as dysbiosis or imbalances in specific bacterial species, can lead to increased inflammation, abnormal fermentation of food, and alterations in gut-brain communication. These changes in gut microbiota composition and function contribute to the development of gastrointestinal symptoms and systemic inflammation observed in individuals with IBS.
Low-Grade Inflammation: While IBS is traditionally considered a functional gastrointestinal disorder, emerging evidence suggests the presence of low-grade inflammation in a subset of individuals with IBS. Increased immune activation and elevated levels of inflammatory mediators have been observed in the gut mucosa of some individuals with IBS, particularly those with post-infectious IBS. This low-grade inflammation may contribute to altered gut function, visceral hypersensitivity, and symptom exacerbation in individuals with IBS.
Alterations in Gut-Brain Communication: Abnormalities in gut-brain communication pathways contribute to the pathophysiology of IBS. Dysregulated signaling between the gut and the brain, mediated by neurotransmitters, neuropeptides, and immune mediators, can lead to alterations in gut motility, visceral sensitivity, and the perception of pain. These alterations in gut-brain communication pathways contribute to the development and maintenance of gastrointestinal symptoms in individuals with IBS. (Assignment Help Example on Irritable Bowel Syndrome: Understanding a Common Gastrointestinal Disorder)
DSM-5 Diagnosis
The diagnosis of Irritable Bowel Syndrome (IBS) is primarily based on clinical criteria outlined in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5). The DSM-5 provides a standardized framework for diagnosing mental and behavioral disorders, including functional gastrointestinal disorders like IBS.
Recurrent Abdominal Pain or Discomfort: The DSM-5 criteria for diagnosing IBS require the presence of recurrent abdominal pain or discomfort for at least three days per month in the last three months. This pain or discomfort is characterized by its association with bowel movements and is often relieved or improved after defecation.
Associated Symptoms: In addition to recurrent abdominal pain or discomfort, the DSM-5 criteria specify the presence of two or more associated symptoms to support the diagnosis of IBS. These associated symptoms include:
- Improvement with Defecation: Symptoms are relieved or improved after bowel movements.
- Onset Associated with a Change in Frequency of Stool: Symptoms are associated with changes in bowel habits, such as diarrhea, constipation, or alternating bowel movements.
- Onset Associated with a Change in Form (Appearance) of Stool: Symptoms are associated with changes in stool consistency, such as loose or hard stools.
Duration and Exclusion Criteria: To meet the DSM-5 criteria for IBS diagnosis, symptoms must be present for at least three months, with symptom onset occurring at least six months prior to diagnosis. Additionally, the diagnosis of IBS requires the exclusion of other gastrointestinal conditions that could account for the symptoms, such as inflammatory bowel disease, celiac disease, or colorectal cancer.
Subtypes of IBS: The DSM-5 recognizes different subtypes of IBS based on predominant bowel habits:
- Diarrhea-Predominant IBS (IBS-D): Characterized by recurrent abdominal pain or discomfort associated with diarrhea.
- Constipation-Predominant IBS (IBS-C): Characterized by recurrent abdominal pain or discomfort associated with constipation.
- Mixed-Type IBS (IBS-M): Characterized by recurrent abdominal pain or discomfort associated with both diarrhea and constipation.
Psychological Factors: While the DSM-5 primarily focuses on the gastrointestinal symptoms of IBS, it also acknowledges the role of psychological factors in the disorder. Psychological distress, including anxiety and depression, commonly co-occur with IBS and may influence symptom severity and treatment outcomes. However, the DSM-5 criteria for IBS diagnosis do not require the presence of specific psychological symptoms.
Overall, the DSM-5 provides a standardized framework for diagnosing IBS based on the presence of recurrent abdominal pain or discomfort and associated symptoms, duration of symptoms, and exclusion of other gastrointestinal conditions. This diagnostic framework facilitates accurate diagnosis and appropriate management of individuals with IBS. (Assignment Help Example on Irritable Bowel Syndrome: Understanding a Common Gastrointestinal Disorder)
Treatment Regimens and Patient Education
Effective management of Irritable Bowel Syndrome (IBS) involves a multidisciplinary approach focused on symptom control, lifestyle modifications, and patient education to improve quality of life and reduce symptom burden.
Dietary Modifications: Dietary modifications are a cornerstone of IBS management and involve identifying and avoiding trigger foods that exacerbate symptoms. Common trigger foods include high-fat foods, spicy foods, caffeine, alcohol, and certain types of carbohydrates known as FODMAPs (fermentable oligosaccharides, disaccharides, monosaccharides, and polyols). Following a low-FODMAP diet, under the guidance of a healthcare professional, can help alleviate symptoms in some individuals with IBS. Additionally, increasing fiber intake through sources such as fruits, vegetables, and whole grains may improve bowel regularity in individuals with constipation-predominant IBS.
Medications: Medications may be prescribed to alleviate specific symptoms of IBS and improve overall symptom control. Depending on the predominant symptoms, medications such as antispasmodics, laxatives, antidiarrheals, or low-dose tricyclic antidepressants may be recommended. For individuals with severe symptoms or refractory to other treatments, newer medications targeting gut motility, visceral hypersensitivity, or gut microbiota may be considered. It is essential for healthcare providers to tailor medication regimens to the individual needs and preferences of patients with IBS.
Stress Management Techniques: Stress is a common trigger for IBS symptoms and can exacerbate gastrointestinal discomfort. Incorporating stress management techniques such as mindfulness, relaxation exercises, deep breathing, yoga, or cognitive-behavioral therapy can help individuals with IBS reduce stress levels and improve symptom control. Identifying and addressing sources of stress in one’s life and developing coping strategies to manage stress effectively are essential components of IBS management.
Behavioral Therapies: Behavioral therapies, including gut-directed hypnotherapy and biofeedback, have been shown to be effective in managing symptoms of IBS. These therapies focus on modifying gut-brain interactions, improving coping skills, and reducing symptom severity. Gut-directed hypnotherapy, in particular, has been shown to alleviate symptoms of IBS and improve overall quality of life in some individuals.
Patient Education: Patient education plays a crucial role in empowering individuals with IBS to manage their symptoms effectively and make informed decisions about their healthcare. Educating patients about the nature of IBS, common triggers, dietary modifications, stress management techniques, and treatment options empowers them to take an active role in their care. Providing written materials, online resources, and access to support groups can further enhance patient education and support self-management of IBS symptoms.
Monitoring and Follow-Up: Regular monitoring and follow-up with healthcare providers are essential components of IBS management. Healthcare providers should regularly assess symptom severity, treatment efficacy, and potential side effects of medications. Adjustments to treatment regimens may be necessary based on individual response and evolving symptoms. Open communication between patients and healthcare providers facilitates ongoing support, education, and optimization of IBS management strategies.
The management of Irritable Bowel Syndrome (IBS) requires a comprehensive approach that addresses symptom control, lifestyle modifications, and patient education. Dietary modifications, medications, stress management techniques, and behavioral therapies play key roles in symptom management and improving quality of life for individuals with IBS. Patient education is essential for empowering individuals to take an active role in managing their symptoms and making informed decisions about their healthcare. By implementing a multidisciplinary approach and providing ongoing support and education, healthcare providers can optimize the management of IBS and improve outcomes for patients. (Assignment Help Example on Irritable Bowel Syndrome: Understanding a Common Gastrointestinal Disorder)