Nursing Paper Example on Hydrocephalus: Understanding a Neurological Disorder
Nursing Paper Example on Hydrocephalus: Understanding a Neurological Disorder
Causes
Hydrocephalus can arise from various factors, both congenital and acquired, that disrupt the normal production, circulation, or absorption of cerebrospinal fluid (CSF) within the brain.
Congenital causes encompass abnormalities in fetal development, such as neural tube defects (e.g., spina bifida) or genetic predispositions. These conditions can interfere with the formation of brain structures or impair CSF flow, leading to fluid accumulation within the ventricles.
Acquired causes of hydrocephalus include infections, such as meningitis or encephalitis, which can inflame the brain’s protective membranes (meninges) and obstruct CSF pathways. Tumors within the brain or spinal cord can also impede fluid circulation by compressing or blocking the ventricular system. Traumatic brain injuries resulting from accidents or hemorrhages can disrupt CSF dynamics, leading to hydrocephalus.
Another common cause of hydrocephalus is a condition known as normal pressure hydrocephalus (NPH), which primarily affects older adults. In NPH, there is an imbalance between CSF production and absorption, leading to its accumulation despite normal pressure readings on cerebrospinal fluid analysis.
Furthermore, certain developmental abnormalities or structural malformations of the brain, such as aqueductal stenosis (narrowing of the cerebral aqueduct), can obstruct the flow of CSF between ventricles, contributing to hydrocephalus.
Additionally, complications from medical procedures, such as hemorrhages following neurosurgery or intraventricular hemorrhage in premature infants, can trigger hydrocephalus.
Understanding the diverse causes of hydrocephalus is essential for accurate diagnosis and tailored treatment strategies. Identifying the underlying etiology guides healthcare professionals in addressing the specific factors contributing to CSF accumulation, thereby optimizing patient management and outcomes. (Nursing Paper Example on Hydrocephalus: Understanding a Neurological Disorder)
Signs and Symptoms
Recognizing the signs and symptoms of hydrocephalus is crucial for early diagnosis and intervention. The presentation of symptoms can vary depending on the age of the individual and the underlying cause of the condition.
In infants, symptoms of hydrocephalus may include an enlarged head circumference (macrocephaly), bulging fontanelles (the soft spots on the baby’s skull), and a rapid increase in head size. Infants may also exhibit irritability, poor feeding, vomiting, and downward deviation of the eyes (sunsetting sign). Additionally, developmental delays, such as delays in achieving motor milestones, may be observed.
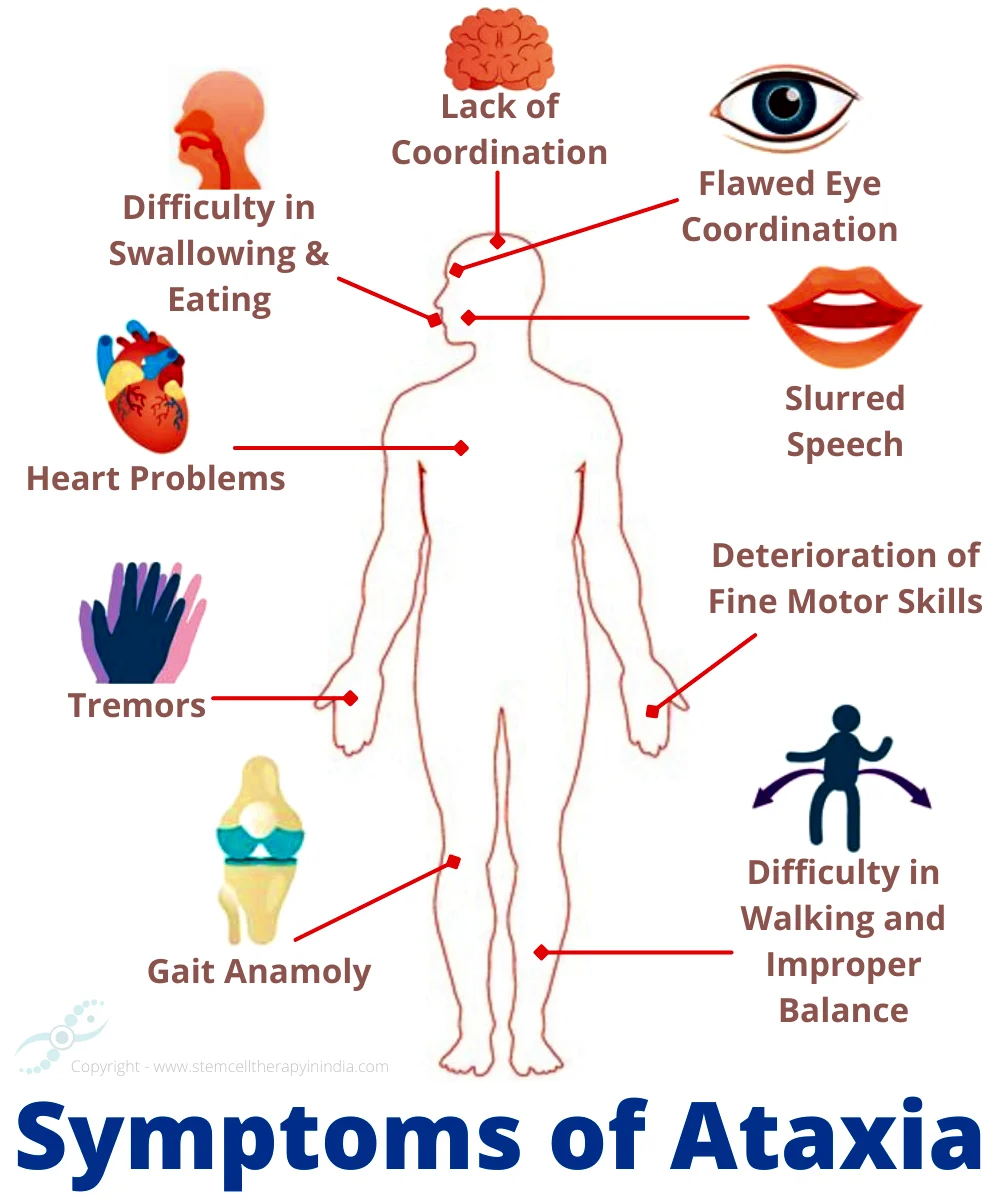
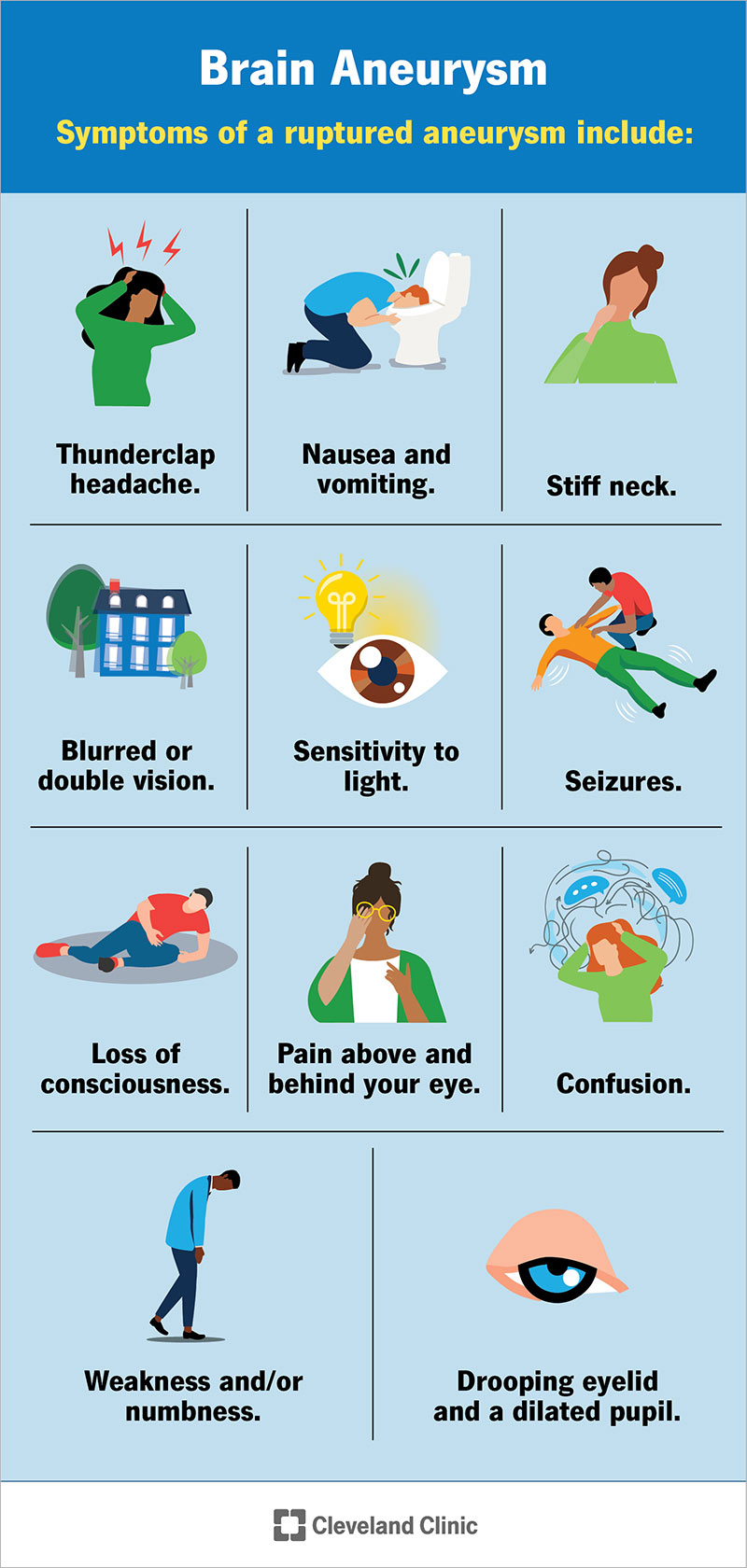
Children and adults with hydrocephalus may experience headaches, which are often worse in the morning or upon waking, due to increased intracranial pressure. Other common symptoms include nausea, vomiting (particularly in the absence of gastrointestinal illness), visual disturbances (such as blurred or double vision), and difficulty with balance or gait.

Cognitive impairments, including memory problems, difficulty concentrating, and changes in mood or behavior, can also occur in individuals with hydrocephalus. Some individuals may experience urinary incontinence or urgency due to pressure on the bladder from enlarged ventricles.
In older adults with normal pressure hydrocephalus (NPH), the classic triad of symptoms consists of gait disturbances (difficulty walking or maintaining balance), urinary incontinence, and cognitive decline (memory problems, slowed thinking). These symptoms may develop gradually over time, leading to a decline in functional abilities and quality of life.
Prompt recognition of these signs and symptoms is essential for timely medical evaluation and diagnosis of hydrocephalus. Early intervention can help alleviate symptoms, prevent complications, and improve long-term outcomes for individuals affected by this neurological disorder. (Nursing Paper Example on Hydrocephalus: Understanding a Neurological Disorder)
Etiology
Understanding the diverse etiology of hydrocephalus involves recognizing the underlying factors that contribute to the abnormal accumulation of cerebrospinal fluid (CSF) within the brain’s ventricular system.

Congenital hydrocephalus often stems from developmental anomalies during fetal growth. Neural tube defects, such as spina bifida or anencephaly, disrupt the proper formation of the brain and spinal cord, leading to CSF circulation abnormalities. Genetic predispositions may also play a role, with certain genetic mutations increasing the risk of hydrocephalus.
Acquired hydrocephalus can result from various factors, including infections that affect the central nervous system. Meningitis or encephalitis can inflame the brain’s protective membranes (meninges), leading to obstruction of CSF pathways and subsequent fluid accumulation. Tumors within the brain or spinal cord can compress or block CSF flow, disrupting normal fluid dynamics. Traumatic brain injuries, such as those caused by accidents or hemorrhages, can also disrupt CSF circulation, leading to hydrocephalus.
Normal pressure hydrocephalus (NPH) often occurs in older adults and is characterized by an imbalance between CSF production and absorption. Although the exact cause of NPH is not fully understood, it may be associated with conditions such as subarachnoid hemorrhage, meningitis, or head trauma.
Structural abnormalities of the brain, such as aqueductal stenosis (narrowing of the cerebral aqueduct), can obstruct CSF flow between ventricles, contributing to hydrocephalus. Additionally, certain medical procedures or complications, such as intraventricular hemorrhage following neurosurgery or premature birth, can lead to hydrocephalus.
Identifying the specific etiological factors contributing to hydrocephalus is essential for tailoring treatment approaches and optimizing outcomes for affected individuals. A comprehensive understanding of the underlying causes guides healthcare professionals in addressing the root factors that drive CSF accumulation, thereby improving patient management and prognosis. (Nursing Paper Example on Hydrocephalus: Understanding a Neurological Disorder)
Pathophysiology
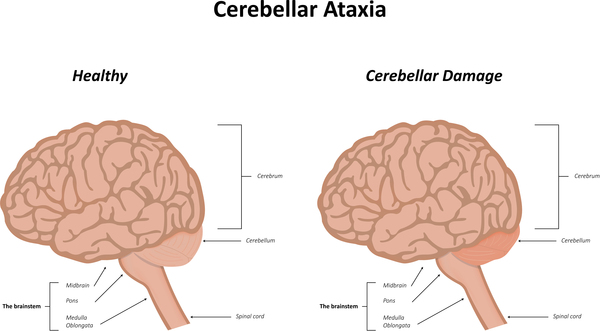
Hydrocephalus arises from disruptions in the delicate balance of cerebrospinal fluid (CSF) dynamics within the brain, leading to abnormal accumulation and increased intracranial pressure.
CSF is produced by the choroid plexus within the brain’s ventricles and serves vital functions, including cushioning the brain, removing waste products, and providing essential nutrients. Under normal circumstances, CSF flows through the ventricular system and is reabsorbed into the bloodstream via arachnoid granulations.
Obstructions or disturbances in CSF circulation disrupt this process, leading to hydrocephalus. Obstructive hydrocephalus occurs when physical blockages, such as tumors, cysts, or structural abnormalities like aqueductal stenosis, obstruct the flow of CSF within the ventricles. This obstruction leads to the accumulation of fluid proximal to the blockage, causing ventricular enlargement and increased intracranial pressure.
Communicating hydrocephalus, on the other hand, involves impaired CSF absorption or reabsorption. In conditions like normal pressure hydrocephalus (NPH), there is an imbalance between CSF production and absorption, leading to fluid accumulation despite normal CSF pressure readings. This accumulation leads to ventricular enlargement and subsequent compression of brain tissue.
Increased intracranial pressure resulting from hydrocephalus can have profound effects on brain function and structure. It can compress and distort brain tissue, leading to neurological deficits, cognitive impairments, and behavioral changes. Additionally, elevated pressure within the skull can impede cerebral blood flow, further compromising brain function.
The pathophysiology of hydrocephalus underscores the importance of timely diagnosis and intervention to alleviate symptoms, prevent complications, and preserve neurological function. Treatment strategies aim to restore normal CSF dynamics through interventions such as shunt placement, endoscopic third ventriculostomy, or other surgical approaches. Understanding the underlying pathophysiological mechanisms guiding hydrocephalus informs healthcare professionals in selecting the most appropriate management strategies for affected individuals, thereby optimizing patient outcomes.
DSM-5 Diagnosis
Diagnosing hydrocephalus involves a comprehensive assessment of clinical symptoms, neuroimaging findings, and underlying etiology, guided by the diagnostic criteria outlined in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5).
The DSM-5 criteria for hydrocephalus primarily focus on the presence of characteristic symptoms and neuroimaging evidence of ventricular enlargement. Symptoms may include headaches, vomiting, visual disturbances, cognitive impairments, gait disturbances, and urinary incontinence, depending on the age and specific type of hydrocephalus.
Neuroimaging modalities such as computed tomography (CT) scans or magnetic resonance imaging (MRI) are essential for confirming the diagnosis. These imaging studies reveal ventricular enlargement, often accompanied by periventricular white matter changes indicative of increased intracranial pressure.
Additionally, the DSM-5 emphasizes the importance of identifying the underlying etiology contributing to hydrocephalus. This involves a thorough medical history, including prenatal or birth complications, previous infections or head injuries, and a family history of neurological disorders. Identifying the specific cause of hydrocephalus aids in tailoring treatment strategies and predicting prognosis.
In cases of normal pressure hydrocephalus (NPH), additional diagnostic criteria include the classic triad of symptoms consisting of gait disturbances, urinary incontinence, and cognitive decline. These symptoms must be present to a significant degree and interfere with daily functioning.
Accurate diagnosis of hydrocephalus is crucial for initiating appropriate treatment interventions, which may include surgical placement of a ventriculoperitoneal shunt, endoscopic third ventriculostomy, or other CSF diversion procedures. Early diagnosis and intervention can help alleviate symptoms, prevent complications, and improve long-term outcomes for individuals affected by hydrocephalus. The DSM-5 criteria serve as a valuable diagnostic tool for healthcare professionals in identifying and managing this complex neurological disorder.
Treatment Regimens and Patient Education
Effective management of hydrocephalus requires a multifaceted approach that includes both medical interventions and patient education aimed at optimizing outcomes and improving quality of life.
Surgical Interventions: Surgical interventions are often necessary to alleviate symptoms and prevent complications associated with hydrocephalus. The most common surgical procedure is the placement of a ventriculoperitoneal (VP) shunt, which diverts excess cerebrospinal fluid (CSF) from the brain’s ventricles to the abdominal cavity, where it can be reabsorbed by the body. Endoscopic third ventriculostomy (ETV) is another surgical option that involves creating a new pathway for CSF drainage within the brain’s ventricular system. The choice of surgical intervention depends on factors such as the underlying cause of hydrocephalus, the patient’s age, and medical history, and the presence of any comorbidities.
Medical Management: In addition to surgical interventions, medical management may be necessary to control symptoms and optimize patient outcomes. This may include medications to alleviate symptoms such as headaches or nausea, as well as ongoing monitoring of CSF pressure levels to ensure optimal shunt function. Physical therapy, occupational therapy, and speech therapy may also be recommended to address functional impairments associated with hydrocephalus.
Patient Education: Patient education plays a crucial role in empowering individuals with hydrocephalus and their caregivers to effectively manage the condition and minimize complications. Key components of patient education include:
- Understanding the Condition: Educating patients and caregivers about the underlying causes, symptoms, and potential complications of hydrocephalus helps them recognize and respond to changes in their condition.
- Shunt Management: For individuals with VP shunts, proper shunt management is essential to prevent complications such as infections or shunt malfunction. Patients and caregivers should receive education on the signs and symptoms of shunt malfunction and when to seek medical attention.
- Lifestyle Modifications: Patients may benefit from lifestyle modifications to optimize their overall health and well-being. This may include maintaining a healthy diet, staying physically active within recommended limits, and managing other medical conditions that may impact hydrocephalus.
- Follow-Up Care: Regular follow-up appointments with healthcare providers are essential for monitoring the effectiveness of treatment interventions and detecting any changes in the condition early. Patients and caregivers should be educated about the importance of attending scheduled appointments and communicating any concerns or changes in symptoms to their healthcare team.
By providing comprehensive education and support, healthcare providers can empower individuals with hydrocephalus to actively participate in their care and achieve the best possible outcomes. Ongoing education and support are essential components of holistic care for individuals affected by this complex neurological disorder. (Nursing Paper Example on Hydrocephalus: Understanding a Neurological Disorder)






:max_bytes(150000):strip_icc()/VWH-AdrianaSanchez-CopingWithAtaxiaTelangiectasia-Standard-3c8f38f48f894426a011ae01d163db01.jpg)







:max_bytes(150000):strip_icc()/rehabilitation-therapies-for-multiple-sclerosis-4072854-e72137c8397a4d909ce759135c9fa3a8.png)