Nursing Paper Example on Hypertension
Nursing Paper Example on Hypertension
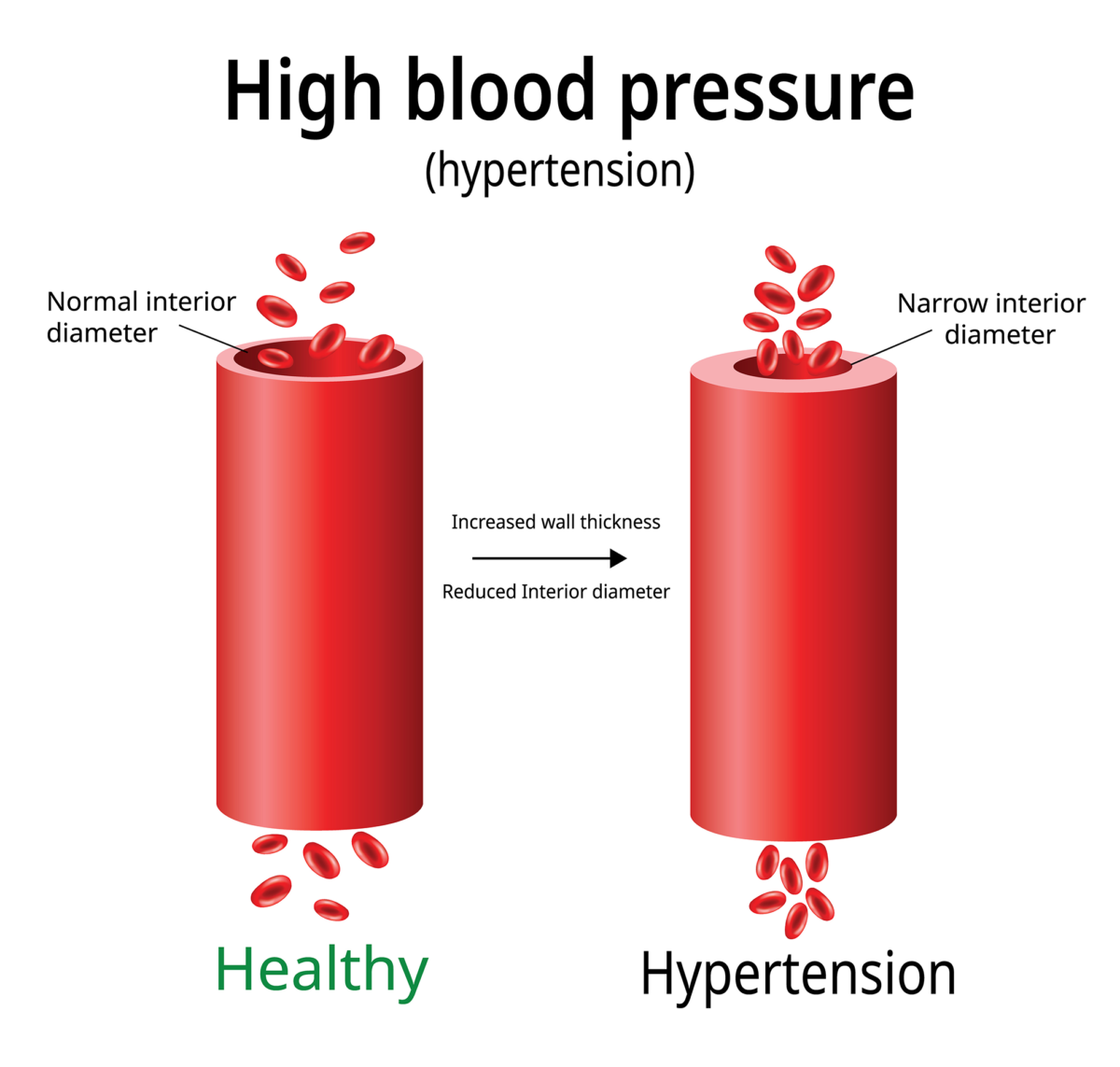
Hypertension, colloquially known as high blood pressure, stands as a pervasive chronic condition silently infiltrating the lives of millions across the globe. Defined by persistently elevated blood pressure levels, this stealthy ailment often conceals itself behind a veil of asymptomatic ambiguity, making it a formidable health concern. Its insidious nature lies in its ability to quietly wreak havoc on the cardiovascular system, laying the foundation for severe complications like heart disease, stroke, and renal impairment. In this context, the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) serves as a crucial guide, emphasizing the necessity of consistent blood pressure readings surpassing the 130/80 mmHg threshold for diagnosis. Beyond its physiological implications, hypertension’s impact extends into the realms of daily functioning, emotional well-being, and overall quality of life. Unmasking this silent threat demands a holistic understanding, with proactive measures woven into the fabric of diagnosis, treatment, and patient education. (Nursing Paper Example on Hypertension)
Signs and Symptoms of Hypertension
Hypertension, although often asymptomatic, manifests through various signs and symptoms, serving as subtle warnings of an underlying cardiovascular challenge.
Elevated Blood Pressure Levels: The hallmark of hypertension lies in consistently elevated blood pressure readings. The systolic pressure, representing the force exerted on the artery walls during a heartbeat, and the diastolic pressure, indicating the pressure between heartbeats, collectively define this crucial health parameter. Normal blood pressure typically hovers around 120/80 mmHg. In hypertension, these numbers escalate, reflecting the increased force exerted by circulating blood against arterial walls. However, it’s essential to note that the absence of noticeable symptoms can make hypertension a silent and insidious adversary, requiring regular monitoring for timely intervention.
Headaches and Dizziness: Some individuals with hypertension may experience recurrent headaches, often concentrated in the back of the head. These headaches result from the increased pressure within the blood vessels, affecting the blood flow to the brain. Dizziness or lightheadedness may accompany these headaches, accentuating the significance of monitoring blood pressure as a preventive measure against potential complications.
Fatigue and Visual Disturbances: Hypertension can induce feelings of persistent fatigue, impacting daily energy levels. Additionally, visual disturbances may arise, including blurred or double vision. These symptoms are attributed to the strain placed on the eyes’ blood vessels, affecting their ability to function optimally. Recognizing these signs is crucial, as they may serve as early indicators prompting individuals to seek medical evaluation and prevent the progression of hypertension. (Nursing Paper Example on Hypertension)
Shortness of Breath: In cases of severe or uncontrolled hypertension, shortness of breath can manifest. Elevated blood pressure puts strain on the heart, affecting its ability to pump blood efficiently. This can lead to inadequate oxygenation of the body, resulting in breathlessness. Shortness of breath is a red flag, indicating the need for immediate medical attention to assess and manage the cardiovascular impact of hypertension.
Chest Pain and Irregular Heartbeat: Chest pain or discomfort, often described as tightness or a squeezing sensation, can accompany hypertension. This occurs when the heart muscles struggle due to increased workload. Furthermore, irregular heartbeat or palpitations may be experienced, reflecting disturbances in the heart’s rhythm. Both symptoms necessitate prompt medical evaluation to rule out serious complications and initiate appropriate interventions.
Flushed or Red Face: External manifestations of hypertension may include a flushed or red face. The increased pressure within blood vessels near the skin’s surface can cause visible changes in skin tone. While this is not universally present in all individuals with hypertension, its occurrence emphasizes the diverse ways in which this condition may manifest.
Nosebleeds: Episodic or recurrent nosebleeds can be associated with hypertension. Elevated blood pressure may weaken small blood vessels in the nasal passages, making them more prone to ruptures. Although nosebleeds can result from various factors, their presence, especially when coupled with other hypertension symptoms, warrants thorough evaluation and blood pressure monitoring.
Understanding these signs and symptoms is pivotal for early detection and intervention. Regular blood pressure monitoring, coupled with awareness of these indicators, empowers individuals to take proactive measures, mitigating the potential complications associated with hypertension. As a silent adversary, hypertension demands keen vigilance on these subtle cues to unveil its presence and pave the way for effective management strategies. (Nursing Paper Example on Hypertension)
Diagnostic Criteria per DSM-5
Diagnosing hypertension follows stringent guidelines outlined by the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5). This essential reference tool emphasizes the persistent nature of elevated blood pressure and provides a standardized framework for clinicians to establish a diagnosis.
To meet the DSM-5 criteria for hypertension, individuals must exhibit consistent blood pressure readings that surpass the defined threshold. The conventional standard, as per recent guidelines, designates a blood pressure reading of 130/80 mmHg or higher as indicative of hypertension. This threshold represents the culmination of extensive research and clinical evidence, establishing the level at which the cardiovascular system faces an increased risk of adverse outcomes. (Nursing Paper Example on Hypertension)
It is crucial to note that a single elevated reading does not suffice for a diagnosis. The DSM-5 underscores the need for repeated measurements on separate occasions to confirm the persistent nature of elevated blood pressure. This precautionary approach aims to prevent misdiagnosis and unnecessary anxiety for individuals with isolated spikes in blood pressure due to situational factors.
Moreover, the DSM-5 recognizes the importance of accurate measurement techniques. Blood pressure measurements should be taken under standardized conditions, with the individual in a relaxed state, following a brief period of rest. Validating the accuracy of blood pressure readings involves employing well-calibrated devices and adhering to established protocols, ensuring reliable data for diagnostic purposes.
The DSM-5 also acknowledges the variability in blood pressure levels, accounting for factors like age, sex, and underlying health conditions. Clinicians utilize population-based norms to contextualize individual readings, allowing for a more nuanced understanding of an individual’s cardiovascular health. (Nursing Paper Example on Hypertension)
The emphasis on persistence in the diagnostic criteria aligns with the chronic nature of hypertension. This chronicity underscores the need for continuous monitoring and management to mitigate the risk of complications. The DSM-5 criteria, thus, serve as a comprehensive guide, offering a standardized approach to diagnosing hypertension while accommodating the dynamic nature of blood pressure regulation in diverse populations.
The DSM-5 criteria provide a structured and evidence-based framework for diagnosing hypertension. By emphasizing the persistence of elevated blood pressure and incorporating considerations for individual variability, these criteria contribute to accurate and reliable diagnoses. Adhering to these guidelines enables clinicians to identify hypertension early, facilitating timely interventions and preventive measures to safeguard cardiovascular health. (Nursing Paper Example on Hypertension)

Complications of Hypertension
Hypertension, if left unmanaged, unfurls a cascade of potentially severe complications, magnifying the significance of early diagnosis and vigilant control.
Heart Disease: Uncontrolled hypertension places an unwarranted burden on the heart. The constant elevated pressure forces the heart to work harder, leading to hypertrophy—the thickening of the heart muscle. This, in turn, elevates the risk of heart failure, where the heart struggles to pump blood effectively. Additionally, hypertension contributes to the development of coronary artery disease, heightening the chances of heart attacks and angina.
Stroke: The impact of hypertension extends to the cerebral vasculature, increasing the likelihood of stroke. Elevated blood pressure can damage blood vessels in the brain, leading to hemorrhagic strokes, where blood vessels rupture, or ischemic strokes, caused by blood clots. Both scenarios can result in irreversible damage to brain tissue, altering cognitive function and mobility.
Kidney Damage: The kidneys, intricate filters essential for eliminating waste from the body, bear the brunt of hypertension. Prolonged high blood pressure can impair the blood vessels in the kidneys, compromising their filtration capabilities. This can culminate in chronic kidney disease, eventually necessitating dialysis or transplantation for survival.
Vision Impairment: The delicate blood vessels in the eyes are vulnerable to the effects of hypertension. Damage to these vessels can lead to retinopathy, characterized by bleeding or swelling in the retina. Left unaddressed, this condition can result in vision impairment or even blindness, underscoring the far-reaching consequences of uncontrolled hypertension.
Aneurysms: Hypertension weakens arterial walls, predisposing individuals to the formation of aneurysms—abnormal bulges in blood vessels. These weakened vessels are at risk of rupturing, causing life-threatening internal bleeding. Aneurysms can occur in various locations, with abdominal and cerebral aneurysms posing substantial risks.
Each of these complications significantly elevates the morbidity and mortality associated with hypertension. They necessitate comprehensive medical management, often involving a combination of lifestyle modifications and pharmacological interventions. The interplay between these complications underscores the systemic impact of hypertension on multiple organ systems.
Understanding the potential consequences of uncontrolled hypertension is pivotal for individuals diagnosed with this condition. Timely and effective management, guided by healthcare professionals, can mitigate the risk of these complications. Regular monitoring, adherence to prescribed treatments, and lifestyle adjustments collectively form a robust defense against the silent but formidable threat that hypertension poses to overall health and well-being. (Nursing Paper Example on Hypertension)
Impact on Someone’s Life
Hypertension, beyond its physiological ramifications, permeates various facets of an individual’s life, influencing daily functioning, emotional well-being, and overall quality of life.
Psychological Toll: The constant awareness of residing on the precipice of a potentially life-threatening condition inflicts a psychological toll. Anxiety and stress become unwelcome companions as individuals navigate the uncertainties associated with hypertension. The specter of complications lurks in the background, shaping daily decisions and permeating thoughts, creating a persistent mental burden.
Altered Daily Functioning: Hypertension’s influence extends into the realm of daily activities. Fatigue, a common symptom, can impede productivity and energy levels. Individuals may find themselves grappling with diminished physical capabilities and a heightened sensitivity to exertion, reshaping their approach to work, exercise, and recreational pursuits.
Impact on Relationships: The emotional weight of hypertension can seep into interpersonal relationships. Family members and friends may witness the challenges faced by individuals managing this condition. The need for lifestyle modifications, dietary restrictions, and medication adherence can introduce complexities into social dynamics, necessitating understanding and support from loved ones.
Financial Implications: The financial strain of managing hypertension cannot be overlooked. Costs associated with medications, regular medical check-ups, and potential hospitalizations contribute to the economic burden. The financial impact may extend to factors such as health insurance premiums, creating an additional layer of stress for those navigating the complexities of hypertension. (Nursing Paper Example on Hypertension)
Diminished Quality of Life: Hypertension, if inadequately controlled, can lead to a diminished overall quality of life. The specter of potential complications may rob individuals of the freedom to fully engage in life’s experiences. Fear and uncertainty can overshadow moments of joy, creating a sense of constraint and limiting the pursuit of a fulfilling and unrestricted life.
Navigating these multifaceted challenges requires a holistic approach to hypertension management. Beyond medical interventions, addressing the emotional and lifestyle aspects is essential. Support networks, both familial and social, play a pivotal role in helping individuals cope with the emotional strain. Furthermore, healthcare providers should adopt a comprehensive perspective, recognizing the interconnectedness of physical and mental well-being in hypertension management. (Nursing Paper Example on Hypertension)
Hypertension is not confined to blood pressure readings; it weaves itself into the fabric of daily life. Recognizing and addressing its impact on psychological well-being, daily functioning, relationships, and financial stability is paramount. By fostering a holistic understanding and providing comprehensive support, healthcare professionals can guide individuals toward a more balanced and fulfilling life despite the challenges posed by this chronic condition.
Treatment Regimens for Hypertension
Effectively managing hypertension demands a multifaceted approach, integrating pharmacological interventions, lifestyle modifications, and patient education to address both the symptoms and underlying causes of the condition. (Nursing Paper Example on Hypertension)

Pharmacological Interventions: Pharmacological treatments play a pivotal role in controlling hypertension. Medications such as angiotensin-converting enzyme (ACE) inhibitors, beta-blockers, calcium channel blockers, and diuretics are commonly prescribed. These medications work by either relaxing blood vessels, reducing the volume of circulating blood, or modifying heart function. Tailoring the medication regimen to an individual’s specific health profile and closely monitoring for potential side effects are crucial aspects of pharmacological management.
Lifestyle Modifications: Non-pharmacological interventions form the cornerstone of hypertension management. Lifestyle modifications encompass dietary changes, regular physical activity, weight management, and stress reduction. Adopting a heart-healthy diet rich in fruits, vegetables, and low-fat dairy products, and limiting sodium intake is crucial. Regular exercise, such as brisk walking or cycling, contributes to weight control and promotes cardiovascular health. Stress management techniques, including mindfulness and relaxation exercises, aid in maintaining optimal blood pressure levels. (Nursing Paper Example on Hypertension)
Patient Education: Educating individuals about hypertension is paramount for effective management and prevention. Patients need a clear understanding of their condition, the importance of medication adherence, and the role of lifestyle modifications. Knowledge about potential complications and the significance of regular blood pressure monitoring empowers individuals to actively participate in their care. Healthcare providers play a crucial role in imparting this knowledge, fostering a collaborative approach that engages patients in the decision-making process. (Nursing Paper Example on Hypertension)
Regular Monitoring: Regular blood pressure monitoring is a key component of both treatment and prevention. Home blood pressure monitors allow individuals to track their blood pressure between medical appointments, providing valuable data for healthcare providers to adjust treatment plans as needed. This proactive approach facilitates early intervention, preventing spikes in blood pressure and reducing the risk of complications.
Preventive Measures: Patient education extends to preventive measures aimed at reducing the risk of developing hypertension. Promoting a heart-healthy lifestyle from an early age, including a balanced diet and regular exercise, can contribute to maintaining optimal blood pressure levels. Additionally, raising awareness about the hereditary component of hypertension encourages individuals with a family history to be vigilant and adopt preventive measures early on.
Hypertension management requires a comprehensive strategy that combines pharmacological and non-pharmacological interventions, supported by patient education. By addressing the condition from multiple angles, healthcare professionals can enhance treatment effectiveness, improve patient outcomes, and empower individuals to take proactive steps in managing and preventing hypertension. (Nursing Paper Example on Hypertension)
Conclusion
Tackling hypertension requires a blend of awareness and action. From spotting the subtle signs to following the DSM-5 guide for diagnosis, the journey through this health challenge is complex. Complications can affect different parts of the body, emphasizing the need for thorough management. Beyond the physical impact, hypertension alters daily life, affecting emotions and even finances. Treatment involves both medicine and lifestyle changes, and educating patients plays a crucial role. Simple steps like eating well, staying active, and keeping stress in check are essential. By understanding the whole picture and using various strategies, both healthcare pros and individuals can team up to control hypertension and improve overall well-being. (Nursing Paper Example on Hypertension)
References






:max_bytes(150000):strip_icc()/heartillustration-58ce8e243df78c3c4f6e87ec.jpg)