Nursing Paper Example on Rift Valley Fever
/in Assignment Help, BLOG, Homework Help /by Aimee GraceNursing Paper Example on Rift Valley Fever
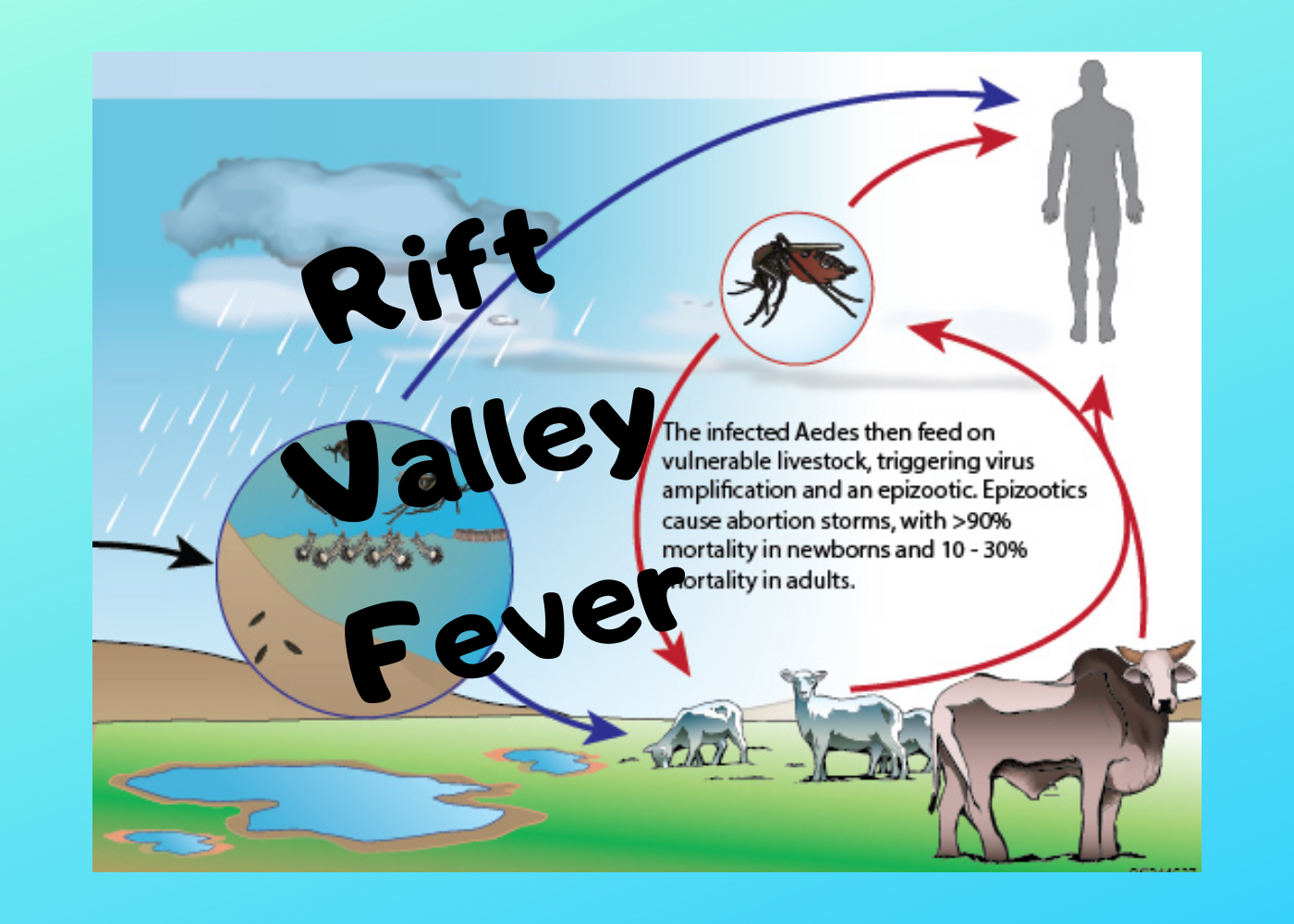
Rift Valley fever (RVF) is a viral zoonotic disease primarily affecting animals, but it can also infect humans. It is caused by the Rift Valley fever virus (RVFV), a member of the genus Phlebovirus in the family Bunyaviridae. RVF is endemic in parts of Africa and the Arabian Peninsula and is transmitted to humans through contact with the blood, body fluids, or tissues of infected animals or through mosquito bites. The disease poses a significant threat to both public health and livestock industries in affected regions.
Causes
Rift Valley fever is caused by the Rift Valley fever virus (RVFV), which primarily infects livestock, including sheep, goats, cattle, and camels. The virus can be transmitted to humans through several routes:
- Mosquito Bites: Mosquitoes, particularly Aedes species, act as vectors of RVFV. Infected mosquitoes transmit the virus through bites, especially during periods of heavy rainfall when mosquito populations surge.
- Direct Contact with Infected Animals: Humans can become infected by handling the blood, tissues, or organs of animals during slaughter or birthing processes. Veterinarians, farmers, and butchers are particularly at risk.
- Consumption of Contaminated Meat or Milk: Ingestion of undercooked or raw animal products from infected animals can lead to infection.
- Aerosol Transmission: In laboratory settings, inhalation of aerosolized particles from infected animals or tissues can transmit the virus.
Epidemiology
RVF was first identified in Kenya in 1931 during an outbreak among sheep. Since then, periodic outbreaks have occurred across sub-Saharan Africa and parts of the Arabian Peninsula. The disease primarily affects regions with heavy rainfall, as flooding creates breeding grounds for mosquitoes, which serve as the primary vector. Livestock, particularly young animals, are highly susceptible to the disease, resulting in high mortality rates during outbreaks. Human cases typically occur in agricultural settings where people come into contact with infected livestock.
(Nursing Paper Example on Rift Valley Fever)
Signs and Symptoms
Rift Valley fever can range from a mild flu-like illness to severe, life-threatening conditions. Most infected individuals experience mild symptoms, while a small percentage develop more severe forms of the disease. The incubation period is typically 2–6 days after exposure to the virus.
- Mild Form: In mild cases, RVF presents with symptoms such as fever, headache, muscle pain, joint pain, and fatigue. These flu-like symptoms usually resolve within a week.
- Severe Form: In severe cases, the disease can progress to more serious conditions:
- Ocular Disease: Retinitis or inflammation of the retina can lead to vision loss, although this is usually temporary.
- Encephalitis: Inflammation of the brain can occur, leading to headaches, seizures, and neurological complications.
- Hemorrhagic Fever: A small percentage of patients develop hemorrhagic symptoms, including vomiting blood, bleeding from the gums or nose, and internal bleeding, which can be fatal.
- Liver Complications: Hepatitis and severe liver damage are common in severe cases of RVF, contributing to multi-organ failure in fatal cases.
Etiology
Rift Valley fever is caused by RVFV, a single-stranded RNA virus in the Bunyaviridae family. The virus can survive in mosquito eggs, allowing it to persist in the environment for extended periods, particularly during dry seasons. When heavy rains occur, mosquito eggs hatch, and infected mosquitoes can spread the virus to animals and humans. Outbreaks are typically associated with climatic events such as floods and heavy rainfall.
Pathophysiology
RVFV enters the body through mosquito bites or direct contact with infected tissues. Once inside the body, the virus replicates in the liver, spleen, and other organs, leading to widespread inflammation and damage. In severe cases, the virus can cause significant liver damage, which disrupts clotting mechanisms and leads to hemorrhagic symptoms. The immune response to the virus also plays a role in the development of encephalitis and retinitis, leading to neurological and ocular complications.
Diagnosis
The diagnosis of Rift Valley fever is confirmed through laboratory testing, as the clinical presentation is often non-specific and resembles other viral infections. Diagnostic methods include:
- Serology: Detection of specific antibodies (IgM and IgG) to RVFV using enzyme-linked immunosorbent assays (ELISA) or other serological tests.
- Polymerase Chain Reaction (PCR): PCR tests can detect viral RNA in blood or tissue samples, allowing for early diagnosis.
- Virus Isolation: In specialized laboratories, RVFV can be isolated from blood or tissue samples through cell culture techniques.
Treatment Regimens
There is no specific antiviral treatment for Rift Valley fever. Management focuses on supportive care to alleviate symptoms and prevent complications. Treatment options include:
- Supportive Care: Patients with mild disease typically recover without medical intervention, but supportive care such as hydration, pain relief, and fever management is essential.
- Hospitalization: Patients with severe disease, especially those with hemorrhagic fever or encephalitis, may require hospitalization. Supportive care may include blood transfusions, intravenous fluids, and monitoring of liver and kidney function.
- Experimental Antivirals: Ribavirin, an antiviral drug, has shown some efficacy in experimental settings, but its use in humans is not yet well-established.
(Nursing Paper Example on Rift Valley Fever)
Prevention
Preventing Rift Valley fever focuses on controlling mosquito populations and minimizing human exposure to infected animals. Key prevention strategies include:
- Vector Control: Reducing mosquito populations through insecticides, draining standing water, and using mosquito nets and repellents.
- Personal Protective Equipment (PPE): Individuals working with livestock should wear gloves, protective clothing, and masks to prevent contact with blood and tissues of infected animals.
- Vaccination of Livestock: Vaccinating livestock against RVFV can reduce the risk of transmission to humans. Live-attenuated and inactivated vaccines are available for animals in endemic areas.
- Public Health Education: Raising awareness about the risks of RVF and promoting safe practices in livestock handling can help reduce human infections.
Complications
In severe cases, Rift Valley fever can lead to life-threatening complications, including:
- Hemorrhagic Fever: Uncontrolled bleeding due to liver dysfunction and coagulopathy can lead to shock and death.
- Encephalitis: Neurological complications can result in long-term cognitive impairment or seizures.
- Vision Loss: Ocular disease can cause permanent vision impairment in a small percentage of patients.
Patient Education
Educating communities in endemic areas is crucial for preventing RVF outbreaks. Key points include:
- Safe Animal Handling: Farmers and veterinarians should use protective measures when handling animals, especially during slaughter or birthing.
- Mosquito Prevention: Communities should be educated on reducing mosquito breeding sites and using protective measures, such as nets and insect repellents.
- Consumption of Safe Animal Products: Proper cooking of meat and boiling of milk can reduce the risk of infection from contaminated animal products.
Conclusion
Rift Valley fever remains a significant public health threat in Africa and the Arabian Peninsula. The disease primarily affects livestock but can have severe consequences for human health. Controlling outbreaks requires a multifaceted approach, including vector control, livestock vaccination, and public health education. With no specific antiviral treatment available, early detection and supportive care are essential for reducing mortality. Continued research and surveillance are necessary to prevent future outbreaks and protect vulnerable populations.
(Nursing Paper Example on Rift Valley Fever)
References
- Centers for Disease Control and Prevention (CDC). Rift Valley Fever. https://www.cdc.gov/vhf/rvf/index.html
- World Health Organization (WHO). Rift Valley Fever. https://www.who.int/news-room/fact-sheets/detail/rift-valley-fever
- LaBeaud, A. D., & Kazura, J. W. (2010). “Rift Valley Fever Virus.” Clinical Microbiology Reviews, 23(2), 277-289. https://doi.org/10.1128/CMR.00035-09
- Daubney, R., Hudson, J. R., & Garnham, P. C. (1931). “Enzootic Hepatitis or Rift Valley Fever: An Undescribed Virus Disease of Sheep, Cattle and Man from East Africa.” The Journal of Pathology and Bacteriology, 34(4), 545-579. https://doi.org/10.1002/path.1700340418
- Bird, B. H., & Nichol, S. T. (2012). “Breaking the Chain: Rift Valley Fever Virus Control via Livestock Vaccination.” Current Opinion in Virology, 2(3), 315-323. https://doi.org/10.1016/j.coviro.2012.03.008







:max_bytes(150000):strip_icc()/VWH-DermNetNZ-PubicLice-01-216e9ce4a4fd4b0c986846a1c8067e82.jpg)
