Nursing Paper Example on Genital Herpes [SOLVED]
Nursing Paper Example on Genital Herpes[SOLVED]
Causes
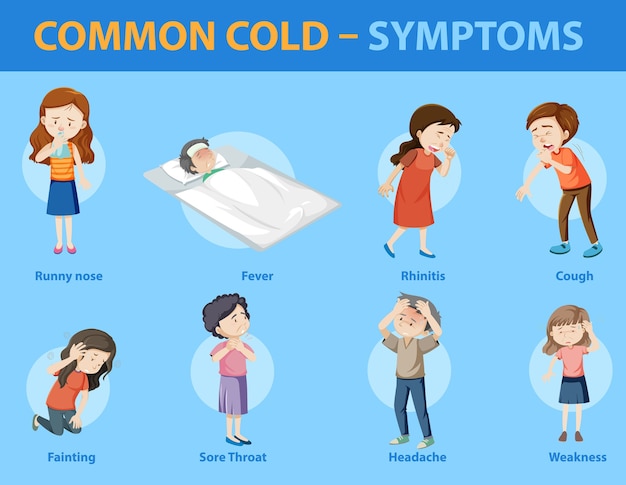
Signs and Symptoms
Genital herpes manifests with a range of signs and symptoms that can significantly impact an individual’s physical and emotional well-being. The pathognomonic signs typically include the development of painful genital ulcers or blisters, accompanied by sensations of itching, burning, or tingling in the genital area. These lesions may appear as small, fluid-filled vesicles that can rupture, leading to the formation of shallow, painful sores. The severity and duration of symptoms can vary widely among individuals, with some experiencing mild discomfort while others endure debilitating pain and discomfort. Additionally, genital herpes outbreaks may be accompanied by systemic symptoms resembling those of influenza, such as fever, body aches, headaches, and swollen lymph nodes in the groin area.
The course of genital herpes is characterized by periods of symptomatic outbreaks interspersed with periods of asymptomatic viral shedding. During asymptomatic shedding, individuals may not exhibit any visible signs or symptoms of infection, yet remain capable of transmitting the virus to sexual partners. Recurrent outbreaks of genital herpes are common and may be triggered by various factors, including stress, illness, hormonal changes, fatigue, or friction during sexual activity. Furthermore, the frequency and severity of outbreaks can vary over time, with some individuals experiencing sporadic episodes while others endure frequent recurrences.
Beyond the physical symptoms, genital herpes can have profound psychological and emotional ramifications, including feelings of shame, guilt, anxiety, depression, and diminished self-esteem. Disclosure of genital herpes status to sexual partners can also pose challenges, leading to fears of rejection, stigma, and relationship strain. Overall, the diverse array of signs and symptoms associated with genital herpes underscores the need for comprehensive education, support, and compassionate care to address the holistic needs of individuals affected by this prevalent sexually transmitted infection. (Nursing Paper Example on Genital Herpes [SOLVED])
![Nursing Paper Example on Genital Herpes: Causes, Symptoms, Diagnosis, and Treatment [SOLVED]](https://www.medicoverhospitals.in/images/diseases/genital-herpes-symptoms.webp)
Etiology
The etiology of genital herpes is multifaceted, involving intricate interactions between the herpes simplex virus (HSV) and various host factors. HSV-1 and HSV-2 are the primary causative agents, with HSV-2 being the predominant strain responsible for genital herpes. Transmission occurs through direct contact with infected mucosal surfaces, genital secretions, or skin lesions during sexual activity, including vaginal, anal, or oral sex. Notably, transmission can occur even when individuals are asymptomatic, complicating prevention efforts and contributing to the widespread prevalence of the infection.
Behavioral factors play a crucial role in the etiology of genital herpes, with unprotected sexual activity, having multiple sexual partners, and engaging in high-risk sexual behaviors increasing the risk of HSV transmission and acquisition. Additionally, certain demographic factors, such as age and gender, may influence susceptibility to infection, with younger individuals and women experiencing higher rates of acquisition.
Moreover, environmental and socioeconomic factors contribute to the epidemiology of genital herpes, with disparities in access to healthcare, sexual health education, and preventive resources influencing the distribution of infection within communities. Individuals from marginalized populations, including racial and ethnic minorities, individuals experiencing homelessness, and those with limited access to healthcare services, may face disproportionate burdens of genital herpes.
Furthermore, the interplay between the immune system and HSV infection is a critical aspect of the etiology of genital herpes. Compromised immune function, as seen in conditions such as HIV/AIDS or immunosuppressive therapy, can increase susceptibility to HSV infection and exacerbate the severity and frequency of outbreaks.
Overall, a comprehensive understanding of the multifaceted etiology of genital herpes is essential for developing effective prevention strategies, promoting sexual health education, and addressing the broader public health implications of this prevalent sexually transmitted infection. (Nursing Paper Example on Genital Herpes [SOLVED])
Pathophysiology
The pathophysiology of genital herpes is characterized by a complex interplay between the herpes simplex virus (HSV) and the host immune response. Following initial infection, HSV establishes latency within sensory nerve ganglia, particularly the sacral ganglia for genital herpes. During latency, the virus remains dormant within the nerve cells, evading immune detection and surveillance.
Periodically, under certain triggers such as stress, illness, hormonal changes, or immunosuppression, the virus undergoes reactivation, resulting in the production of new viral particles. These particles travel along sensory nerve fibers to the site of primary infection in the genital mucosa, where they replicate and cause recurrent outbreaks of genital herpes.
The mechanisms underlying HSV reactivation are multifactorial and not yet fully elucidated. However, it is believed that various stimuli, including neuronal and hormonal factors, ultraviolet radiation, trauma, and inflammation, can disrupt the delicate balance between viral latency and reactivation.
During outbreaks, HSV replicates within epithelial cells of the genital mucosa, leading to the formation of characteristic vesicles and ulcers. Viral replication triggers local inflammation, resulting in tissue damage and the release of proinflammatory cytokines. This inflammatory response contributes to the clinical manifestations of genital herpes, including pain, itching, and erythema.
Furthermore, viral shedding occurs intermittently, even in the absence of visible lesions, allowing for the transmission of HSV to sexual partners. Asymptomatic shedding poses challenges for both diagnosis and prevention, as individuals may unknowingly transmit the virus to others.
Overall, the pathophysiology of genital herpes involves a dynamic interplay between viral replication, immune evasion, and host inflammatory responses. Understanding these underlying mechanisms is crucial for developing targeted therapeutic interventions and preventive strategies aimed at mitigating the burden of genital herpes and reducing its transmission within the population. (Nursing Paper Example on Genital Herpes [SOLVED])
DSM-5 Diagnosis
The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5), does not provide specific diagnostic criteria for genital herpes. However, it acknowledges the psychological impact of sexually transmitted infections (STIs) on affected individuals and emphasizes the importance of considering the psychosocial context when assessing and managing these conditions.
Diagnosis of genital herpes primarily relies on clinical evaluation, including a thorough medical history, physical examination, and laboratory testing. Clinicians assess for the presence of characteristic symptoms, such as painful genital ulcers or lesions, itching, burning sensations, and flu-like symptoms. A detailed sexual history is essential for identifying potential risk factors, recent sexual contacts, and previous STI diagnoses.
Laboratory tests play a supplementary role in confirming the diagnosis of genital herpes and identifying the causative strain of the herpes simplex virus (HSV). Common diagnostic modalities include viral culture, polymerase chain reaction (PCR) testing, and serological assays for HSV antibodies. Viral culture and PCR testing can detect the presence of HSV DNA in genital lesions or secretions, providing definitive evidence of active infection. Serological testing measures the presence of HSV-specific antibodies in the blood, aiding in the diagnosis of past or asymptomatic infections.
Moreover, the DSM-5 underscores the importance of addressing the psychological and emotional aspects of genital herpes diagnosis and management. Individuals diagnosed with genital herpes may experience a range of psychosocial reactions, including anxiety, depression, stigma, and relationship distress. Healthcare providers should offer empathetic support, counseling, and resources to help patients cope with the emotional impact of the diagnosis and navigate disclosure to sexual partners.
In summary, while the DSM-5 does not provide specific diagnostic criteria for genital herpes, it highlights the significance of considering the psychological dimensions of STI diagnosis and management. A comprehensive approach to diagnosis, including clinical evaluation and laboratory testing, coupled with supportive counseling, is essential for addressing the holistic needs of individuals affected by genital herpes. (Nursing Paper Example on Genital Herpes [SOLVED])
Treatment Regimens and Patient Education
Effective management of genital herpes involves a combination of antiviral medications, supportive care, and patient education aimed at symptom relief, outbreak prevention, and reducing the risk of transmission to sexual partners.
Antiviral Therapy: Antiviral medications such as acyclovir, valacyclovir, and famciclovir are the cornerstone of treatment for genital herpes. These medications work by inhibiting viral replication, thereby reducing the severity and duration of outbreaks. Treatment regimens may vary depending on the frequency and severity of symptoms, ranging from episodic therapy for symptomatic outbreaks to suppressive therapy for individuals with frequent recurrences. Episodic therapy involves starting antiviral medication at the onset of symptoms and continuing for a specified duration to hasten healing and alleviate symptoms. Suppressive therapy entails daily use of antiviral medication to reduce the frequency and severity of outbreaks, as well as asymptomatic shedding, thereby lowering the risk of transmission to sexual partners.
Supportive Care: In addition to antiviral therapy, supportive care measures can help alleviate symptoms and promote healing during genital herpes outbreaks. These may include topical treatments such as lidocaine or benzocaine creams to relieve pain and discomfort, as well as sitz baths with warm water to soothe genital lesions and promote healing. Patients should also be advised to avoid tight-fitting clothing, irritants, and sexual activity during outbreaks to prevent exacerbation of symptoms and reduce the risk of transmission.
Patient Education: Patient education plays a crucial role in empowering individuals with genital herpes to manage their condition effectively and make informed decisions regarding treatment and prevention. Healthcare providers should provide comprehensive information about the nature of genital herpes, including its transmission, symptoms, and potential complications. Patients should be counseled on the importance of safer sexual practices, including condom use, disclosure of herpes status to sexual partners, and risk reduction strategies. Additionally, patients should be encouraged to seek regular medical follow-up for monitoring and adjustment of treatment regimens as needed. Emphasizing the importance of open communication with sexual partners and destigmatizing discussions surrounding genital herpes can help reduce feelings of shame, guilt, and isolation often associated with the condition.
A multifaceted approach to genital herpes management encompassing antiviral therapy, supportive care, and patient education is essential for optimizing outcomes and improving the quality of life for individuals affected by this common sexually transmitted infection. By providing comprehensive care and empowering patients with knowledge and resources, healthcare providers can mitigate the burden of genital herpes and promote sexual health and well-being. (Nursing Paper Example on Genital Herpes [SOLVED])
Conclusion

![Nursing Paper Example on Genital Herpes: Causes, Symptoms, Diagnosis, and Treatment [SOLVED]](https://www.mymed.com/image/1470/medicalarticle/800)

![Nursing Paper Example on Gonorrhea [SOLVED]](https://wdy.h-cdn.co/assets/17/20/1024x512/gallery-1495059098-gonorrhea-symptoms-in-women.jpg)
![Nursing Paper Example on Gonorrhea [SOLVED]](https://www.ncbi.nlm.nih.gov/books/NBK558903/bin/gonorrhea.jpg)
![Nursing Paper Example on Chorea [SOLVED]](https://www.physio-pedia.com/images/thumb/8/8d/Chorea.jpeg/300px-Chorea.jpeg)
![Nursing Paper Example on Chronic Fatigue Syndrome [SOLVED]](https://static.independent.co.uk/s3fs-public/thumbnails/image/2017/11/29/10/istock-6104496044444.jpg?width=1200&height=1200&fit=crop)
![Nursing Paper Example on Chronic Fatigue Syndrome [SOLVED]](https://images.herzindagi.info/image/2023/Sep/chronic-fatigue-syndrome-symptoms.jpg)
![Nursing Paper Example on Circadian Rhythm Sleep Disorder [SOLVED]](https://i0.wp.com/post.medicalnewstoday.com/wp-content/uploads/sites/3/2022/09/circadian_rhythm_sleep_disorder_bw_1296x728_header-1024x575.jpg?w=1155&h=1528)
![Nursing Paper Example on Circadian Rhythm Sleep Disorder [SOLVED]](https://www.pulmonarydocs.com/img/shutterstock_360063584.jpg)
 Causes
Causes
 Causes
Causes