Nursing Paper Example on Cancer: Understanding the Complexity of a Devastating Disease
Nursing Paper Example on Cancer: Understanding the Complexity of a Devastating Disease
 Causes
Causes
The causes of cancer are multifactorial, encompassing a complex interplay of genetic, environmental, and lifestyle factors. Genetic mutations play a significant role in cancer development, with alterations in key genes leading to uncontrolled cell growth and proliferation. These mutations can be inherited from parents or acquired over time due to exposure to environmental carcinogens or errors in DNA replication.
Environmental factors also contribute to cancer risk, with exposure to carcinogens such as tobacco smoke, air pollutants, industrial chemicals, and radiation increasing the likelihood of developing certain types of cancer. Additionally, lifestyle choices such as diet, physical activity level, and alcohol consumption influence cancer risk. A diet high in processed meats, saturated fats, and refined sugars, combined with a sedentary lifestyle, is associated with an increased risk of developing cancer.
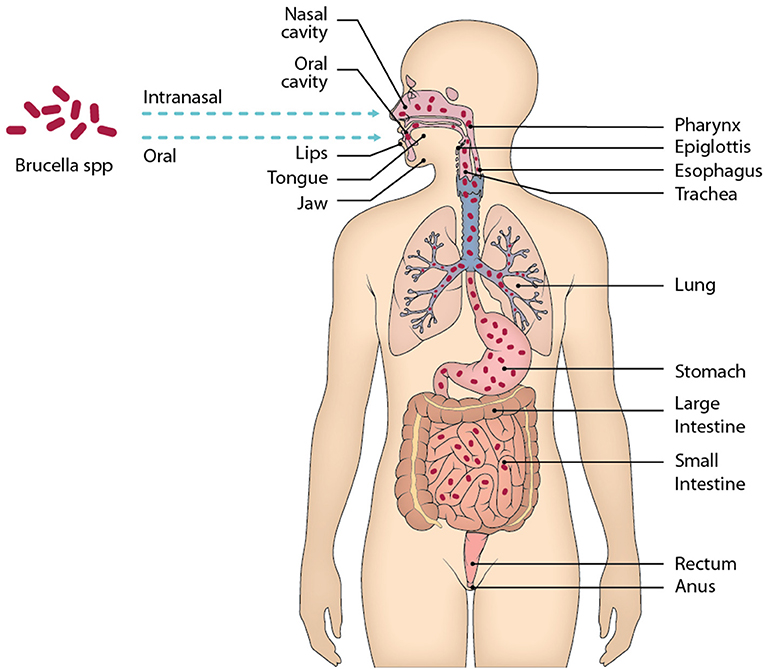
Chronic inflammation is another contributing factor to cancer development, as it creates an environment conducive to tumor growth and progression. Infections with certain viruses and bacteria, such as human papillomavirus (HPV), hepatitis B and C viruses, and Helicobacter pylori, can lead to chronic inflammation and increase the risk of developing specific types of cancer.
Furthermore, hormonal factors play a role in cancer development, particularly in hormone-sensitive cancers such as breast and prostate cancer. Hormonal imbalances, reproductive factors, and hormone replacement therapy can influence cancer risk.
Additionally, age is a significant risk factor for cancer, with the incidence of most types of cancer increasing with age. This is partly due to the accumulation of genetic mutations and exposure to environmental carcinogens over time.
In summary, cancer is a complex disease with diverse and interconnected causes. Understanding the various factors contributing to cancer development is crucial for implementing effective prevention strategies and reducing the burden of this disease on individuals and society. (Nursing Paper Example on Cancer: Understanding the Complexity of a Devastating Disease)
Signs and Symptoms
Recognizing the signs and symptoms of cancer is paramount for early detection and timely intervention. While the presentation of cancer varies depending on the type and location of the tumor, certain common indicators warrant attention.
Unexplained weight loss is a red flag often associated with various types of cancer. Sudden and unintentional weight loss, especially when accompanied by other symptoms, may signify an underlying malignancy.
Persistent fatigue is another prevalent symptom in individuals with cancer. Fatigue that persists despite adequate rest and sleep can be indicative of an underlying medical condition, including cancer.
The presence of lumps or masses in the body can also be a warning sign of cancer. These abnormal growths may be palpable under the skin or internally and require evaluation by a healthcare professional.
Changes in bowel or bladder habits should not be ignored, as they may indicate gastrointestinal or genitourinary cancers. Symptoms such as blood in the stool or urine, persistent constipation or diarrhea, and urinary urgency or frequency warrant further investigation.
Persistent cough or hoarseness can be early indicators of lung, throat, or vocal cord cancers. These symptoms should prompt evaluation, especially in individuals with a history of smoking or exposure to environmental carcinogens.
Unexplained pain, particularly if it persists or worsens over time, may be a sign of cancer. Pain that is not attributable to other known causes or does not improve with treatment should be investigated further.
Other symptoms that may raise suspicion of cancer include unexplained fever, night sweats, and changes in skin pigmentation or texture.
It is essential to note that while these signs and symptoms may suggest the presence of cancer, they can also be indicative of other benign conditions. However, any persistent or concerning symptoms should prompt consultation with a healthcare professional for proper evaluation and diagnosis. Early detection and prompt treatment are key to improving outcomes in individuals with cancer. (Nursing Paper Example on Cancer: Understanding the Complexity of a Devastating Disease)
Etiology
The etiology of cancer is multifaceted and encompasses a wide array of factors that contribute to its development. Central to cancer etiology are genetic alterations, which can occur through inherited mutations or acquired changes during an individual’s lifetime. Inherited genetic mutations, such as those associated with the BRCA1 and BRCA2 genes in breast and ovarian cancers, predispose individuals to an increased risk of developing cancer.
Environmental factors also play a crucial role in cancer etiology. Exposure to carcinogens, including tobacco smoke, ultraviolet radiation, asbestos, and certain chemicals found in the workplace or environmental pollution, can damage cellular DNA and initiate the process of carcinogenesis.
Lifestyle choices significantly influence cancer risk and etiology. Poor dietary habits, including consumption of processed foods high in saturated fats and sugars, as well as low intake of fruits and vegetables, are associated with an increased risk of certain cancers. Sedentary behavior and obesity are also established risk factors for cancer development.
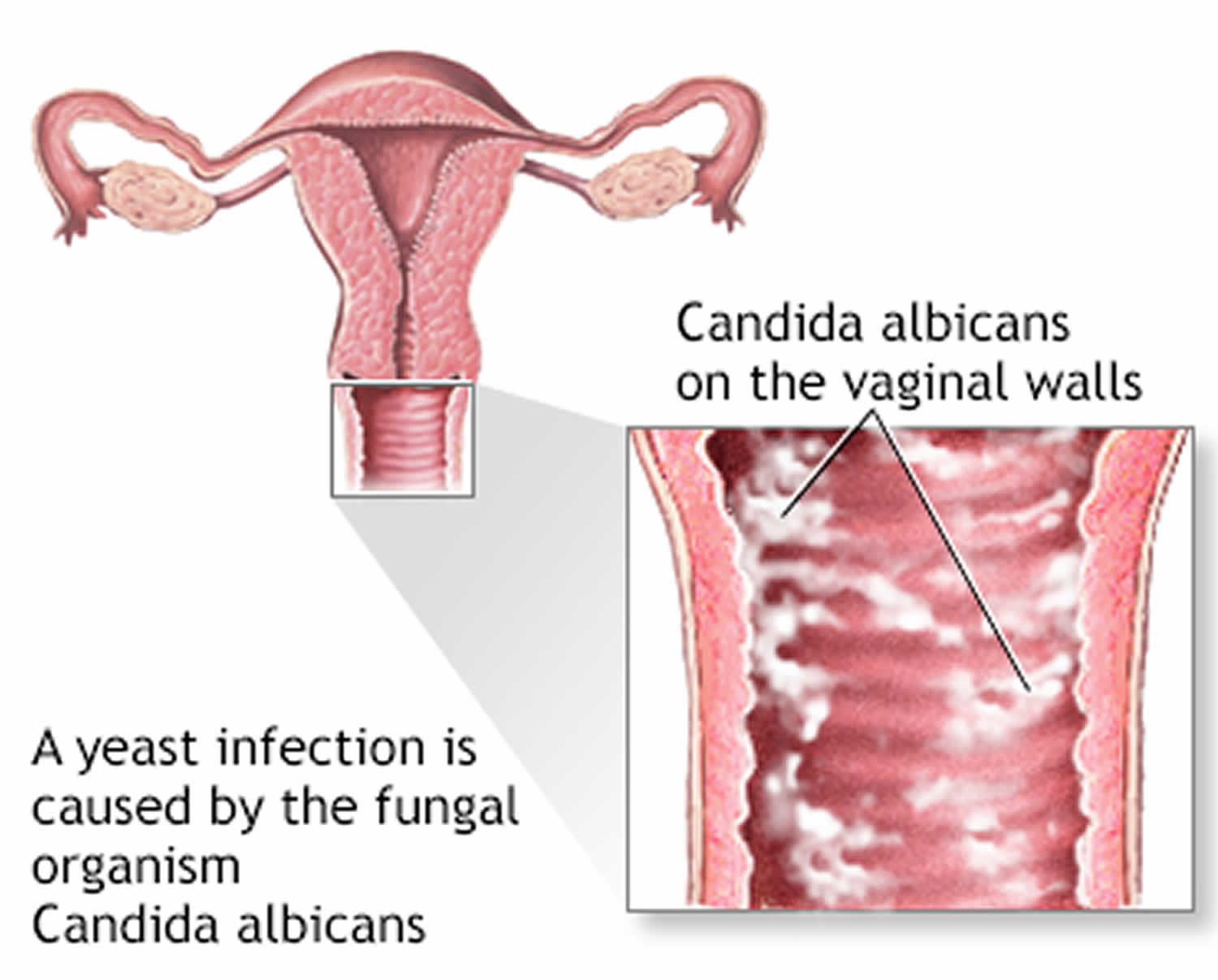
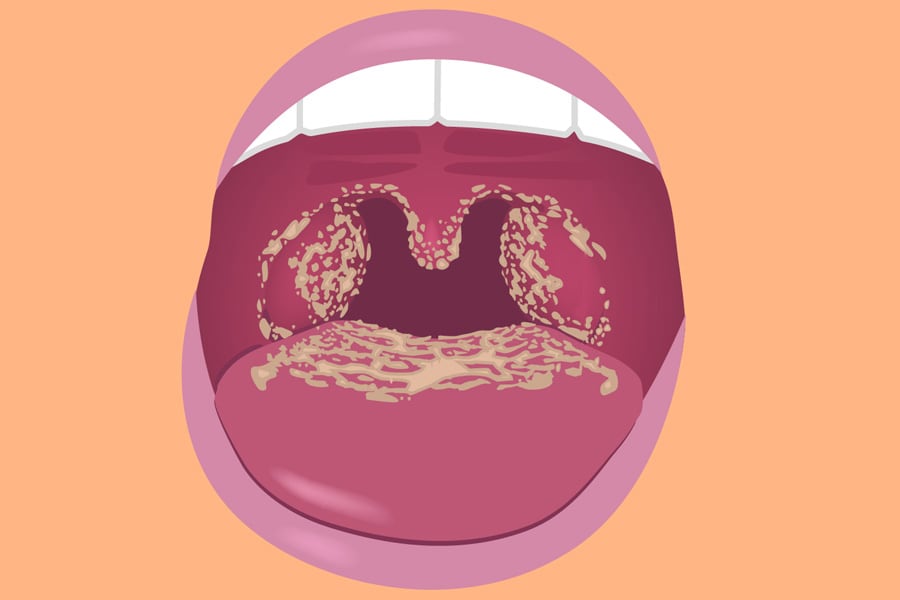
Chronic inflammation is a hallmark of cancer etiology, contributing to tumor initiation, promotion, and progression. Infections with certain viruses and bacteria can induce chronic inflammation and increase cancer risk. For example, chronic infection with the human papillomavirus (HPV) is a major risk factor for cervical, anal, and oropharyngeal cancers.
Hormonal factors also play a significant role in cancer etiology, particularly in hormone-sensitive cancers such as breast and prostate cancer. Hormonal imbalances, reproductive factors, and exogenous hormone use can influence cancer risk and progression.
Moreover, age is a fundamental factor in cancer etiology, with the incidence of most cancers increasing with advancing age. The accumulation of genetic mutations, prolonged exposure to environmental carcinogens, and changes in hormonal levels over time contribute to the age-related increase in cancer risk.
In summary, cancer etiology is complex and multifactorial, involving interactions between genetic, environmental, lifestyle, inflammatory, hormonal, and age-related factors. Understanding the diverse etiological factors contributing to cancer development is crucial for implementing effective prevention strategies and reducing the global burden of this disease. (Nursing Paper Example on Cancer: Understanding the Complexity of a Devastating Disease)
Pathophysiology
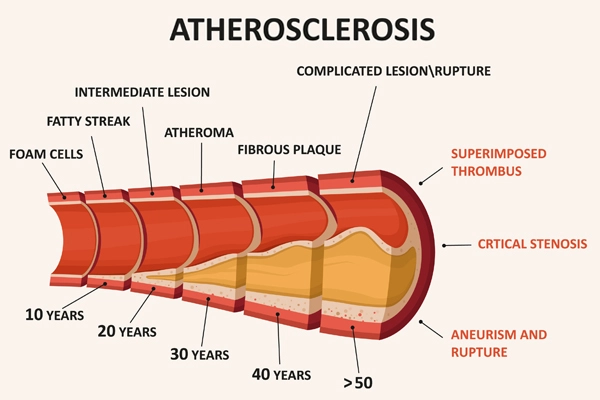
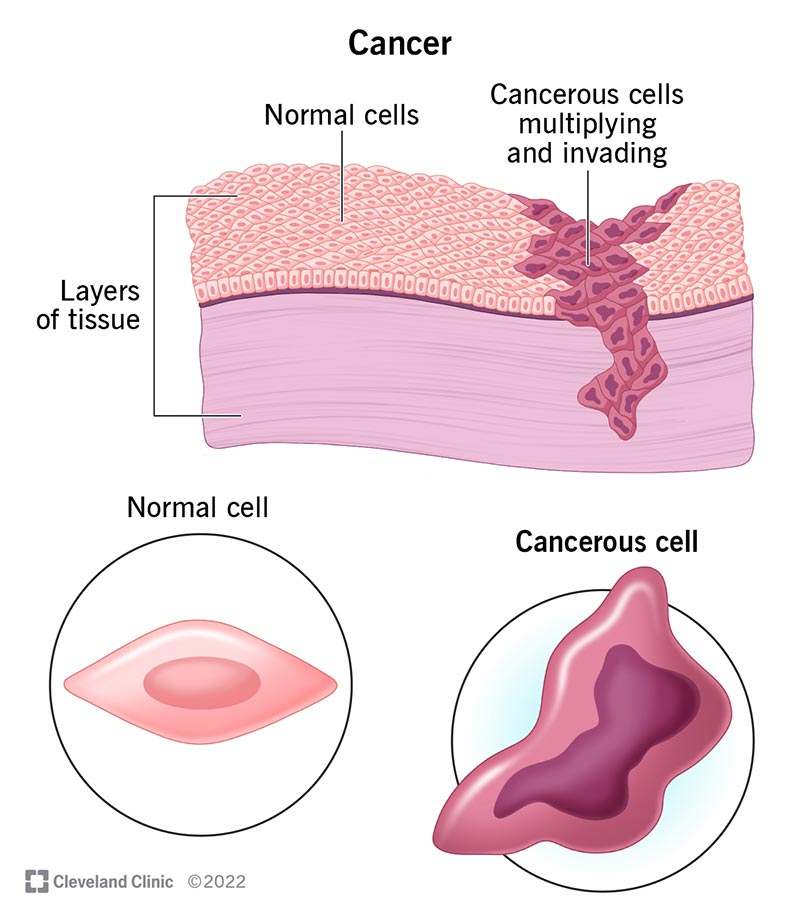
The pathophysiology of cancer involves a complex interplay of molecular and cellular events that culminate in uncontrolled growth and spread of abnormal cells. This process, known as carcinogenesis, is characterized by several key hallmarks that distinguish cancer cells from normal cells.
One hallmark of cancer pathophysiology is sustained proliferative signaling, where cancer cells acquire the ability to proliferate indefinitely due to the dysregulation of signaling pathways involved in cell growth and division. This results from genetic mutations that activate oncogenes or inactivate tumor suppressor genes, leading to uncontrolled cell cycle progression.
Another hallmark is evasion of growth suppressors, whereby cancer cells bypass mechanisms that normally inhibit excessive cell growth. Dysregulation of apoptosis, the programmed cell death process, allows cancer cells to evade cell death and persist despite genetic damage or cellular stress.
Additionally, cancer cells exhibit replicative immortality, a hallmark stemming from the activation of telomerase or alternative lengthening of telomeres, enabling unlimited cell division potential.
Angiogenesis, the process of forming new blood vessels, is crucial for tumor growth and metastasis. Cancer cells secrete pro-angiogenic factors that stimulate the formation of new blood vessels, ensuring adequate nutrient and oxygen supply to support tumor growth.
Cancer cells also possess invasive and metastatic capabilities, allowing them to invade surrounding tissues, intravasate into blood or lymphatic vessels, and establish distant metastases. This metastatic spread is facilitated by alterations in cell adhesion molecules and extracellular matrix remodeling enzymes.
Furthermore, cancer cells exhibit tumor-promoting inflammation, which creates a microenvironment conducive to tumor growth and progression. Inflammatory mediators released by cancer cells and tumor-associated immune cells promote angiogenesis, tissue remodeling, and immune evasion.
Overall, the pathophysiology of cancer involves a complex interplay of genetic, molecular, and cellular alterations that confer hallmark traits enabling cancer cells to proliferate, evade growth suppressors, resist cell death, sustain replicative immortality, promote angiogenesis, invade and metastasize, and induce tumor-promoting inflammation. Understanding these underlying mechanisms is essential for developing targeted therapies and improving outcomes for individuals affected by cancer. (Nursing Paper Example on Cancer: Understanding the Complexity of a Devastating Disease)
DMS-5 Diagnosis
The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5), provides criteria for diagnosing specific types of cancer based on clinical presentation, imaging studies, and laboratory findings. Diagnosing cancer involves a multidisciplinary approach, with healthcare professionals utilizing a combination of tools and techniques to accurately identify the presence and extent of the disease.
One of the primary methods used for cancer diagnosis is imaging studies, including computed tomography (CT) scans, magnetic resonance imaging (MRI), positron emission tomography (PET) scans, and ultrasound. These imaging modalities allow healthcare providers to visualize internal organs and tissues, identify suspicious masses or lesions, and determine the extent of tumor involvement.
Laboratory studies are also essential for cancer diagnosis, with blood tests, tumor markers, and biopsy specimens providing valuable information about the nature and characteristics of the disease. Blood tests may reveal abnormalities such as elevated levels of tumor markers, which are substances produced by cancer cells or the body in response to cancer. Tumor markers such as prostate-specific antigen (PSA), carcinoembryonic antigen (CEA), and CA-125 are commonly used to screen for and monitor certain types of cancer.
Biopsy specimens obtained through procedures such as fine-needle aspiration, core biopsy, or surgical excision allow for the histological examination of tissue samples under a microscope. Pathological analysis of biopsy specimens provides critical information about the type of cancer, its grade and stage, and other important characteristics that guide treatment decisions.
In addition to imaging studies and laboratory tests, clinical evaluation by healthcare providers plays a crucial role in cancer diagnosis. Healthcare professionals assess patients’ medical history, perform physical examinations, and review symptoms to determine the likelihood of cancer and guide further diagnostic investigations.
Overall, the DSM-5 diagnosis of cancer involves a comprehensive evaluation encompassing imaging studies, laboratory tests, biopsy specimens, and clinical assessment. By integrating these diagnostic approaches, healthcare providers can accurately identify cancer, characterize its features, and develop tailored treatment plans to optimize patient outcomes. (Nursing Paper Example on Cancer: Understanding the Complexity of a Devastating Disease)
Treatment Regimens and Patient Education
The treatment of cancer is highly individualized and may involve a combination of modalities tailored to the specific type, stage, and characteristics of the disease, as well as the patient’s overall health and preferences. Treatment regimens typically include a combination of surgery, chemotherapy, radiation therapy, targeted therapy, immunotherapy, hormone therapy, and supportive care interventions.
Surgery is often the primary treatment for solid tumors and involves the removal of the cancerous tissue. Depending on the extent of the disease, surgery may be curative or palliative, aiming to remove the entire tumor or alleviate symptoms and improve quality of life.
Chemotherapy utilizes powerful medications to destroy cancer cells or inhibit their growth. These drugs may be administered orally or intravenously and may be used as a standalone treatment or in combination with other modalities such as surgery or radiation therapy.
Radiation therapy employs high-energy beams to target and destroy cancer cells while minimizing damage to surrounding healthy tissue. It is often used in conjunction with surgery or chemotherapy to enhance treatment efficacy or as a standalone therapy for certain types of cancer.
Targeted therapy utilizes drugs or other substances that specifically target cancer cells or their molecular pathways, minimizing harm to healthy cells. These therapies are designed to interfere with specific proteins or signaling pathways involved in cancer growth and progression.
Immunotherapy harnesses the body’s immune system to recognize and destroy cancer cells. These treatments work by stimulating the immune response or by removing barriers that prevent immune cells from recognizing and attacking cancer cells.
Hormone therapy is commonly used to treat hormone-sensitive cancers such as breast and prostate cancer. These therapies work by blocking the production or action of hormones that promote cancer growth.
Patient education is an integral component of cancer care, empowering individuals to make informed decisions about their treatment options, manage treatment-related side effects, and adopt healthy lifestyle behaviors. Patients should be provided with comprehensive information about their diagnosis, treatment plan, potential side effects, and available support services.
Additionally, patients should be encouraged to actively participate in their care by asking questions, expressing concerns, and seeking clarification as needed. Patient education materials, support groups, and counseling services can help individuals cope with the emotional and psychological challenges associated with cancer diagnosis and treatment.
By incorporating patient education into cancer care, healthcare providers can enhance treatment adherence, improve patient satisfaction, and promote overall well-being throughout the cancer journey. Empowering patients with knowledge and support enables them to navigate the complexities of cancer treatment and achieve the best possible outcomes. (Nursing Paper Example on Cancer: Understanding the Complexity of a Devastating Disease)


:max_bytes(150000):strip_icc()/VWH-JessicaOlah-CommonSymptomsofCarbonMonoxidePoisoning-Standard-460087eaa2ad4058af35e4606caabe07.jpg)

:max_bytes(150000):strip_icc()/what-is-botulism-4142153-FINAL-e8e26c264c8e4e55a73f560fdd87c420.gif)