Nursing Paper Example on Brown-Sequard Syndrome: An Overview
/in Assignment Help, Assignment Help Nursing, BLOG, Homework Help, Nursing Exam Help, Nursing Paper Help, Solved Nursing Essays /by Aimee GraceNursing Paper Example on Brown-Sequard Syndrome: An Overview
Brown-Sequard Syndrome, named after its discoverer Charles-Édouard Brown-Séquard, is a rare neurological disorder that affects the spinal cord, resulting in distinct neurological deficits. This syndrome, often caused by traumatic spinal cord injuries or other pathological conditions, presents with a unique set of symptoms that can vary in severity depending on the location and extent of the spinal cord damage. Understanding the causes, signs, and treatment options for Brown-Sequard Syndrome is crucial for healthcare professionals to provide effective care and support to affected individuals. This paper aims to explore the causes, signs and symptoms, etiology, pathophysiology, DSM-5 diagnosis, treatment regimens and patient education, and conclude with insights into this complex neurological disorder. By delving into these aspects, we can gain a comprehensive understanding of Brown-Sequard Syndrome and its implications for patient care and management. (Nursing Paper Example on Brown-Sequard Syndrome: An Overview)

Causes of Brown-Sequard Syndrome
Brown-Sequard Syndrome typically arises from traumatic injuries to the spinal cord, often resulting from accidents, falls, or acts of violence. These injuries can lead to compression, contusion, or laceration of the spinal cord, disrupting its normal function. Additionally, tumors, both primary and metastatic, can impinge upon the spinal cord, causing damage and subsequent neurological deficits characteristic of Brown-Sequard Syndrome.
Infections such as abscesses or inflammatory conditions like transverse myelitis can also affect the spinal cord, leading to this syndrome. Moreover, degenerative diseases such as multiple sclerosis or spinal cord ischemia due to vascular disorders can contribute to the development of Brown-Sequard Syndrome.
Penetrating injuries, such as gunshot wounds or stab wounds, pose a significant risk for causing Brown-Sequard Syndrome by directly damaging one side of the spinal cord. The severity of the syndrome often correlates with the extent of spinal cord injury, with complete transections resulting in more profound deficits compared to partial injuries.
Additionally, certain medical procedures, such as spinal surgeries or epidural steroid injections, carry a risk of complications that may include damage to the spinal cord, potentially leading to Brown-Sequard Syndrome.
Rarely, non-traumatic causes such as spinal cord infarction, spinal cord tumors, or vascular malformations can also result in Brown-Sequard Syndrome. In some cases, the exact cause of the syndrome may remain unknown, especially when no clear traumatic or pathological event precipitates its onset.
Overall, Brown-Sequard Syndrome can stem from various causes, including traumatic injuries, tumors, infections, degenerative diseases, and vascular disorders affecting the spinal cord. Understanding these diverse etiologies is crucial for accurate diagnosis and effective management of this neurological disorder. (Nursing Paper Example on Brown-Sequard Syndrome: An Overview)
Signs and Symptoms
The signs and symptoms of Brown-Sequard Syndrome are characterized by a distinct pattern of neurological deficits resulting from damage to one side of the spinal cord. These deficits typically manifest differently depending on the level and extent of the spinal cord injury.
One of the hallmark features of Brown-Sequard Syndrome is weakness or paralysis on one side of the body, known as hemiparaplegia. This weakness affects the muscles controlled by the damaged portion of the spinal cord, leading to impaired motor function.
In addition to hemiparaplegia, individuals with Brown-Sequard Syndrome may experience loss of sensation on the same side of the body as the paralysis. This sensory loss typically involves deficits in proprioception, tactile sensation, and vibration sense, reflecting the disruption of sensory pathways within the spinal cord.
Conversely, individuals with Brown-Sequard Syndrome often retain sensation on the opposite side of the body, known as the contralateral side. This preservation of sensation on the unaffected side is a distinguishing feature of the syndrome and is attributed to the intact sensory pathways on the contralateral side of the spinal cord.
Furthermore, individuals with Brown-Sequard Syndrome may exhibit altered reflexes on the affected side of the body, such as hyperreflexia or hyporeflexia, depending on the level of the spinal cord injury and the involvement of specific reflex arcs.
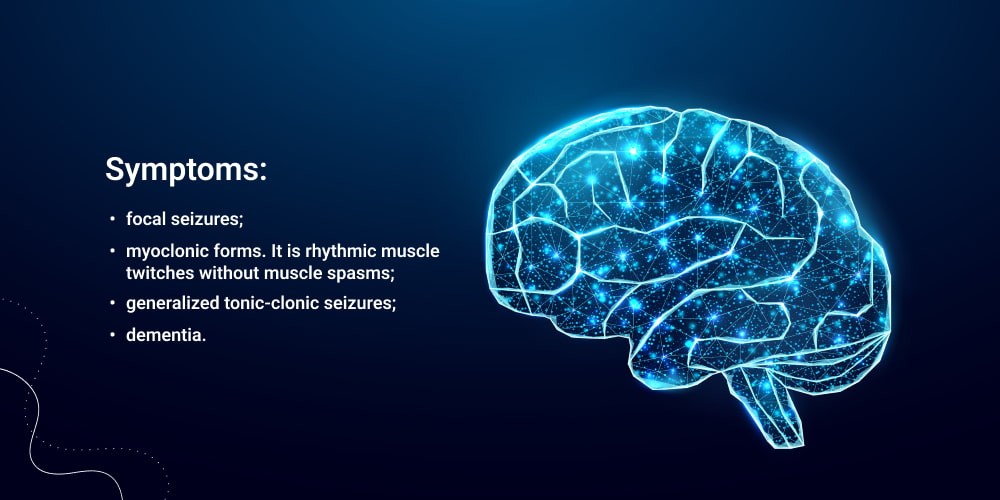
Other less common symptoms of Brown-Sequard Syndrome may include urinary or bowel dysfunction, sexual dysfunction, and disturbances in temperature regulation due to disruption of autonomic pathways within the spinal cord.
Overall, the signs and symptoms of Brown-Sequard Syndrome reflect the hemisection of the spinal cord, resulting in a characteristic pattern of motor, sensory, and autonomic deficits on the affected side of the body. Recognizing these symptoms is crucial for timely diagnosis and management of this rare neurological disorder. (Nursing Paper Example on Brown-Sequard Syndrome: An Overview)
Etiology of Brown-Sequard Syndrome
Brown-Sequard Syndrome arises from damage to one side of the spinal cord, leading to specific neurological deficits characteristic of the syndrome. The etiology of this condition can be attributed to various factors, including traumatic injuries, pathological conditions, and iatrogenic causes.
Traumatic injuries, such as those sustained in accidents, falls, or acts of violence, are among the most common causes of Brown-Sequard Syndrome. These injuries can result in compression, contusion, or laceration of the spinal cord, leading to disruption of sensory and motor pathways on one side of the body.
Pathological conditions, including tumors and infections, can also contribute to the development of Brown-Sequard Syndrome. Tumors, both primary and metastatic, can exert pressure on the spinal cord, causing damage and subsequent neurological deficits characteristic of the syndrome. Similarly, infections such as abscesses or inflammatory conditions like transverse myelitis can affect the spinal cord, leading to similar neurological deficits.
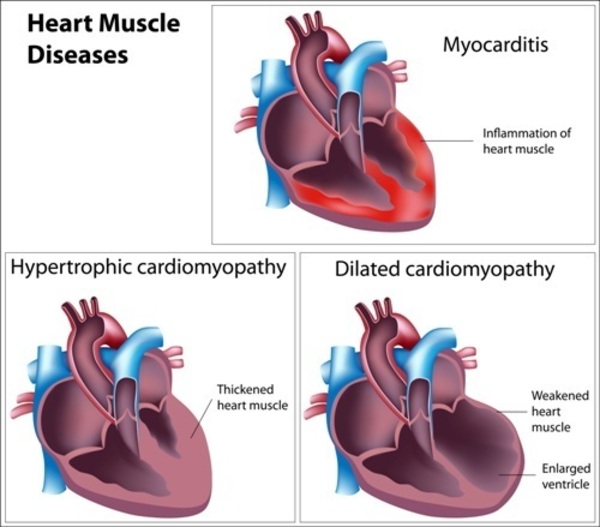
Degenerative diseases, such as multiple sclerosis or spinal cord ischemia due to vascular disorders, can also lead to Brown-Sequard Syndrome. These conditions can cause damage to the spinal cord, disrupting its normal function and resulting in characteristic symptoms of the syndrome.
Iatrogenic causes, including complications from medical procedures such as spinal surgeries or epidural steroid injections, can also result in Brown-Sequard Syndrome. These procedures carry a risk of complications that may include damage to the spinal cord, leading to neurological deficits characteristic of the syndrome.
Overall, the etiology of Brown-Sequard Syndrome is diverse and can include traumatic injuries, pathological conditions, degenerative diseases, and iatrogenic causes. Understanding these various etiologies is essential for accurate diagnosis and effective management of this neurological disorder. (Nursing Paper Example on Brown-Sequard Syndrome: An Overview)
Pathophysiology
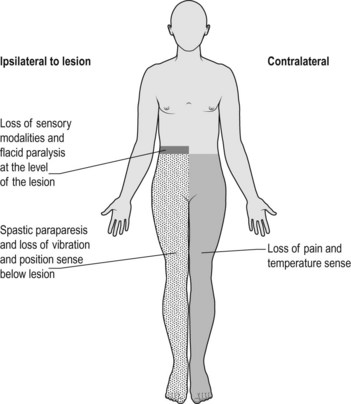
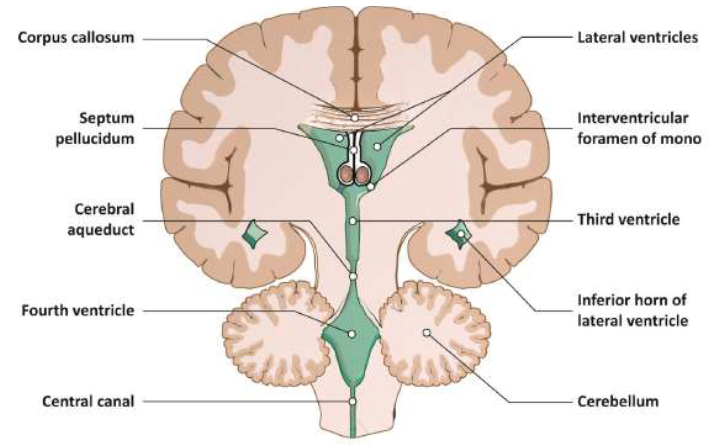
Brown-Sequard Syndrome is characterized by a distinct pattern of neurological deficits resulting from damage to one side of the spinal cord, leading to disruption of sensory and motor pathways. The pathophysiology of this syndrome involves the hemisection of the spinal cord, which affects sensory and motor functions differently depending on the location and extent of the injury.
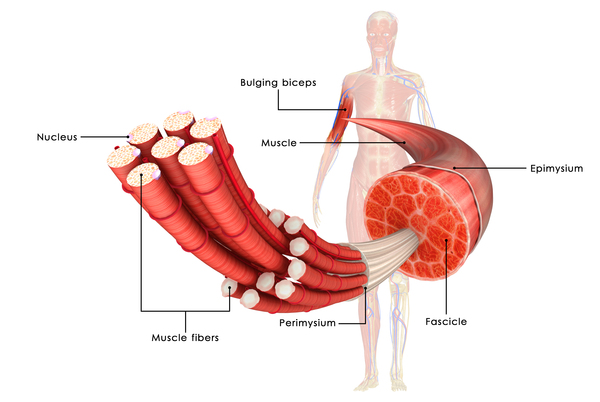
The spinal cord comprises white matter tracts that transmit sensory information from the periphery to the brain and motor commands from the brain to the muscles, as well as gray matter regions involved in processing and integrating this information. Damage to one side of the spinal cord disrupts these pathways, leading to specific deficits on the affected side of the body.
In Brown-Sequard Syndrome, the hemisection of the spinal cord results in ipsilateral paralysis or weakness on the same side of the body as the injury. This paralysis occurs due to the disruption of descending motor pathways that control voluntary movement.
Conversely, individuals with Brown-Sequard Syndrome typically retain proprioception and tactile sensation on the same side of the body as the paralysis. This preservation of sensation is attributed to intact dorsal columns on the ipsilateral side of the spinal cord, which transmit sensory information related to proprioception, tactile sensation, and vibration sense.
However, individuals with Brown-Sequard Syndrome often experience loss of pain and temperature sensation on the contralateral side of the body due to disruption of spinothalamic tracts that transmit these sensory modalities. This contralateral sensory loss is a distinguishing feature of the syndrome and reflects the hemisection of the spinal cord.
Overall, the pathophysiology of Brown-Sequard Syndrome involves disruption of sensory and motor pathways within the spinal cord, resulting in characteristic deficits on the affected side of the body. Understanding this pathophysiology is crucial for accurate diagnosis and targeted management of this neurological disorder. (Nursing Paper Example on Brown-Sequard Syndrome: An Overview)
DSM-5 Diagnosis
The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5), does not provide specific diagnostic criteria for Brown-Sequard Syndrome, as it primarily focuses on psychiatric disorders. However, diagnosis of Brown-Sequard Syndrome is typically based on clinical presentation, imaging studies, and neurological assessments.
Clinical presentation plays a key role in diagnosing Brown-Sequard Syndrome. Healthcare professionals evaluate the patient’s history of trauma or other underlying conditions, as well as the presence of characteristic signs and symptoms such as hemiparaplegia, sensory deficits, and altered reflexes.
Imaging studies, particularly magnetic resonance imaging (MRI), are instrumental in confirming the diagnosis of Brown-Sequard Syndrome. MRI can reveal the location and extent of spinal cord injury, which helps differentiate Brown-Sequard Syndrome from other spinal cord disorders.
Neurological assessments are essential for evaluating the severity and extent of neurological deficits associated with Brown-Sequard Syndrome. These assessments may include testing motor function, sensation, reflexes, and autonomic function on both sides of the body.
Overall, while the DSM-5 does not provide specific diagnostic criteria for Brown-Sequard Syndrome, healthcare professionals rely on clinical presentation, imaging studies, and neurological assessments to diagnose this rare neurological disorder. The diagnosis is based on a comprehensive evaluation of the patient’s history, symptoms, and objective findings, which guide appropriate management and treatment interventions. (Nursing Paper Example on Brown-Sequard Syndrome: An Overview)

Treatment Regimens and Patient Education
Effective management of Brown-Sequard Syndrome involves a multidisciplinary approach aimed at addressing the underlying cause, managing symptoms, and maximizing functional recovery. Treatment regimens may include a combination of medical interventions, physical therapy, occupational therapy, medications, and surgical procedures tailored to the individual patient’s needs.
Medical interventions focus on addressing the underlying cause of Brown-Sequard Syndrome, such as surgical decompression for spinal cord compression due to tumors or traumatic injuries. In cases of infection, antibiotics or antiviral medications may be prescribed to control the infection and prevent further damage to the spinal cord.
Physical therapy plays a crucial role in rehabilitation and maximizing functional recovery for individuals with Brown-Sequard Syndrome. Physical therapists design customized exercise programs to improve strength, flexibility, balance, and coordination, targeting specific areas affected by the syndrome. These exercises help individuals regain motor function and enhance their overall mobility and independence.
Occupational therapy focuses on enhancing activities of daily living (ADLs) and adaptive skills to promote independence and improve quality of life. Occupational therapists provide training in techniques to compensate for sensory deficits and develop strategies to overcome challenges related to mobility, self-care, and participation in meaningful activities.
Medications may be prescribed to manage symptoms associated with Brown-Sequard Syndrome, such as pain, spasticity, and neuropathic pain. Common medications include analgesics, muscle relaxants, and anticonvulsants, which help alleviate discomfort and improve overall comfort and well-being.
In some cases, surgical interventions may be necessary to address specific complications or improve outcomes for individuals with Brown-Sequard Syndrome. Surgical procedures may include spinal fusion, decompression laminectomy, or tumor resection, depending on the underlying cause and extent of spinal cord injury.
Patient education is essential for individuals with Brown-Sequard Syndrome to understand their condition, treatment options, and strategies for managing symptoms and promoting recovery. Healthcare professionals provide information about the nature of the syndrome, expected outcomes, and potential complications. Patients and their caregivers learn techniques for preventing complications such as pressure ulcers, urinary tract infections, and deep vein thrombosis.
Furthermore, patients receive guidance on lifestyle modifications, including maintaining a healthy diet, staying physically active within their abilities, and managing stress. Patient education empowers individuals with Brown-Sequard Syndrome to actively participate in their care, make informed decisions, and optimize their overall well-being and quality of life. (Nursing Paper Example on Brown-Sequard Syndrome: An Overview)
Conclusion
Brown-Sequard Syndrome is a rare neurological disorder characterized by specific deficits resulting from spinal cord injury. Understanding its causes, symptoms, diagnosis, and treatment is crucial for effective management and patient care. Traumatic injuries, tumors, infections, and degenerative diseases are common causes, leading to a distinct pattern of motor and sensory deficits. The pathophysiology involves disruption of sensory and motor pathways within the spinal cord, resulting in hemisection and ipsilateral paralysis. While the DSM-5 does not provide specific diagnostic criteria, clinical presentation, imaging studies, and neurological assessments aid in diagnosis. Treatment regimens include medical interventions, physical and occupational therapy, medications, and surgical procedures tailored to individual needs. Patient education plays a vital role in empowering individuals to actively participate in their care and optimize their quality of life. By addressing these aspects comprehensively, healthcare professionals can improve outcomes and enhance the overall well-being of individuals with Brown-Sequard Syndrome. (Nursing Paper Example on Brown-Sequard Syndrome: An Overview)













:max_bytes(150000):strip_icc()/VWH-MiraNorian-Encephalitis-4000x2700-d724354b09df4b4a81520987ba5f6b52.png)