Nursing Exam Help Example on Lactose Intolerance: Understanding and Management
Nursing Exam Help Example on Lactose Intolerance: Understanding and Management
Causes
Lactose intolerance predominantly arises from genetic factors, notably variations in the LCT gene that encodes lactase, the enzyme responsible for breaking down lactose. These genetic variations result in reduced lactase activity, leading to impaired lactose digestion. Ethnicity plays a significant role, with certain populations exhibiting higher prevalence rates. For instance, lactose intolerance is more prevalent among individuals of East Asian, African, Hispanic, and Native American descent compared to those of Northern European ancestry.

Secondary causes of lactose intolerance include gastrointestinal diseases or conditions that damage the small intestine’s lining, thereby affecting lactase production. Conditions such as celiac disease, inflammatory bowel disease (IBD), Crohn’s disease ulcerative colitis, and intestinal infections can lead to temporary lactose intolerance due to injury to the intestinal mucosa.
Moreover, surgeries involving the small intestine, such as gastric bypass surgery, can also result in lactose intolerance, as the portion of the small intestine responsible for lactase production may be bypassed or removed during the procedure.
Additionally, age-related decline in lactase activity is another common cause of lactose intolerance. While infants typically produce abundant lactase to digest breast milk or formula, lactase production tends to decline with age in many individuals, particularly after childhood. This age-related decline in lactase activity contributes to the increased prevalence of lactose intolerance in adulthood.
Furthermore, medications or treatments affecting the gastrointestinal tract can also induce lactose intolerance as a side effect. For instance, certain antibiotics, chemotherapy drugs, and radiation therapy targeting the abdomen can damage the intestinal lining, impairing lactase production and leading to temporary lactose intolerance.
Overall, lactose intolerance can stem from a variety of causes, including genetic predisposition, ethnicity, gastrointestinal diseases or conditions, age-related decline in lactase activity, surgical interventions, and medications. Understanding these diverse factors contributing to lactose intolerance is essential for accurate diagnosis and effective management of this common gastrointestinal disorder. (Nursing Exam Help Example on Lactose Intolerance: Understanding and Management)
Signs and Symptoms
Lactose intolerance manifests through a range of gastrointestinal symptoms that typically occur within 30 minutes to two hours after consuming lactose-containing foods or beverages. These symptoms can vary in severity among affected individuals and may include:
- Abdominal Pain: One of the hallmark symptoms of lactose intolerance is abdominal pain, characterized by cramping or discomfort in the abdominal region. The pain may vary in intensity and duration, depending on the amount of lactose ingested and individual tolerance levels.
- Bloating: Bloating, or the sensation of abdominal fullness and distension, is commonly reported by individuals with lactose intolerance. Excessive gas production due to lactose fermentation in the colon contributes to abdominal bloating and discomfort.
- Flatulence: Increased gas production resulting from the fermentation of undigested lactose by colonic bacteria leads to excessive flatulence in individuals with lactose intolerance. This symptom is often accompanied by abdominal discomfort and bloating.
- Diarrhea: Diarrhea is a common symptom of lactose intolerance, characterized by loose or watery stools occurring shortly after consuming lactose-containing foods or beverages. The osmotic effect of undigested lactose in the colon draws water into the intestines, leading to diarrhea.
- Nausea: Some individuals with lactose intolerance may experience nausea or an uneasy sensation in the stomach after consuming lactose-containing foods. Nausea may be accompanied by other gastrointestinal symptoms such as abdominal pain or bloating.
- Vomiting: In more severe cases or individuals with heightened sensitivity to lactose, vomiting may occur as a response to ingesting lactose. Vomiting may be accompanied by other symptoms such as abdominal pain or diarrhea.
- Generalized Discomfort: Overall discomfort or unease in the abdominal region is a common complaint among individuals with lactose intolerance. This discomfort may not be localized to a specific area but rather encompasses a generalized feeling of gastrointestinal distress.
It is essential for individuals experiencing these symptoms to consult a healthcare professional for proper evaluation and diagnosis. Identifying lactose intolerance early can help individuals manage their symptoms effectively through dietary modifications and other treatment strategies, improving their overall quality of life. (Nursing Exam Help Example on Lactose Intolerance: Understanding and Management)
Etiology
The primary etiology of lactose intolerance lies in the deficiency or reduced activity of the lactase enzyme, which is responsible for breaking down lactose into its constituent sugars, glucose, and galactose, for absorption in the small intestine. This deficiency can be attributed to various factors, including genetic predisposition and ethnic background.
Genetic Factors: Genetic variations in the LCT gene, which encodes the lactase enzyme, play a significant role in the development of lactose intolerance. Certain individuals inherit genetic variants that result in decreased expression or activity of the lactase enzyme, leading to reduced lactase levels in the small intestine. These genetic variations are more prevalent in populations with a history of dairy farming or cattle herding, where lactose consumption historically declined with age due to dietary changes.
Ethnic Background: Lactose intolerance exhibits variations in prevalence among different ethnic groups, reflecting the influence of genetic factors and cultural dietary practices. For example, lactose intolerance is more common in individuals of East Asian, African, Hispanic, and Native American descent compared to those of Northern European ancestry. This variation in prevalence is attributed to genetic differences in lactase enzyme activity among populations and historical dietary patterns, where lactose consumption was traditionally limited in certain ethnic groups.
Secondary Causes: In addition to genetic predisposition, certain gastrointestinal diseases or conditions can contribute to secondary lactose intolerance. Conditions such as celiac disease, inflammatory bowel disease (IBD), Crohn’s disease, ulcerative colitis, and intestinal infections can damage the intestinal mucosa, affecting lactase production and leading to temporary lactose intolerance.
Age-Related Decline: Another contributing factor to lactose intolerance is the age-related decline in lactase activity. While infants produce abundant lactase to digest breast milk or formula, lactase production tends to decrease with age in many individuals, particularly after childhood. This age-related decline in lactase activity contributes to the increased prevalence of lactose intolerance in adulthood.
Understanding the diverse etiological factors underlying lactose intolerance is essential for accurate diagnosis and appropriate management strategies tailored to individual patient needs. Identifying the underlying cause of lactose intolerance can guide healthcare professionals in recommending effective treatment options and dietary modifications to alleviate symptoms and improve patient outcomes. (Nursing Exam Help Example on Lactose Intolerance: Understanding and Management)
Pathophysiology
The pathophysiology of lactose intolerance involves the impaired digestion of lactose due to deficient or reduced lactase enzyme activity in the small intestine, leading to the characteristic gastrointestinal symptoms experienced by affected individuals.
Upon ingestion, lactose, a disaccharide found in dairy products, requires hydrolysis by the enzyme lactase into its constituent monosaccharides, glucose, and galactose, for absorption in the small intestine. In individuals with lactose intolerance, insufficient lactase activity hinders the complete hydrolysis of lactose, resulting in undigested lactose reaching the colon.
In the colon, undigested lactose serves as a substrate for colonic bacteria, which ferment lactose through the process of bacterial fermentation. This fermentation process produces gases, including hydrogen, methane, and carbon dioxide, as well as short-chain fatty acids. The production of gases leads to abdominal distension and discomfort, while the osmotic effect of undigested lactose draws water into the colon, contributing to diarrhea.
Furthermore, the fermentation of lactose by colonic bacteria results in the production of short-chain fatty acids, such as acetate, propionate, and butyrate. These fatty acids can stimulate colonic motility and secretion, exacerbating gastrointestinal symptoms such as abdominal pain and diarrhea.
The severity of symptoms in lactose intolerance can vary depending on several factors, including the degree of lactase deficiency, the amount of lactose ingested, individual tolerance levels, and the composition of colonic microbiota. Some individuals may experience mild symptoms with small amounts of lactose, while others may exhibit more pronounced symptoms with larger lactose loads.
It is important to note that lactose intolerance differs from milk allergy, which involves an immune-mediated response to proteins in milk rather than an enzymatic deficiency. Distinguishing between lactose intolerance and milk allergy is crucial for accurate diagnosis and appropriate management of gastrointestinal symptoms.
Overall, the pathophysiology of lactose intolerance centers around deficient lactase enzyme activity, impaired lactose digestion, bacterial fermentation of undigested lactose in the colon, and the subsequent production of gases and short-chain fatty acids, leading to the characteristic gastrointestinal symptoms experienced by affected individuals. Understanding the underlying pathophysiological mechanisms of lactose intolerance is essential for guiding effective management strategies and improving patient outcomes. (Nursing Exam Help Example on Lactose Intolerance: Understanding and Management)

DMS-5 Diagnosis
The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5), provides criteria for diagnosing lactose intolerance. While lactose intolerance is primarily a gastrointestinal disorder, it is not listed in the DSM-5 as a standalone diagnosis. However, healthcare professionals may consider the following diagnostic criteria and guidelines when assessing individuals for lactose intolerance:
- Clinical Evaluation: Healthcare providers typically begin the diagnostic process by conducting a thorough clinical evaluation, which includes assessing the patient’s medical history, dietary habits, and gastrointestinal symptoms.
- Symptom Presentation: The DSM-5 does not specify diagnostic criteria for lactose intolerance. However, healthcare providers consider the characteristic gastrointestinal symptoms associated with lactose intolerance, such as abdominal pain, bloating, flatulence, diarrhea, nausea, and vomiting, occurring after the consumption of lactose-containing foods or beverages.
- Dietary History: Healthcare providers may inquire about the patient’s dietary history, specifically their consumption of dairy products and any associated symptoms following lactose ingestion. Patients may be asked to maintain a food diary to track their dietary intake and symptom occurrence.
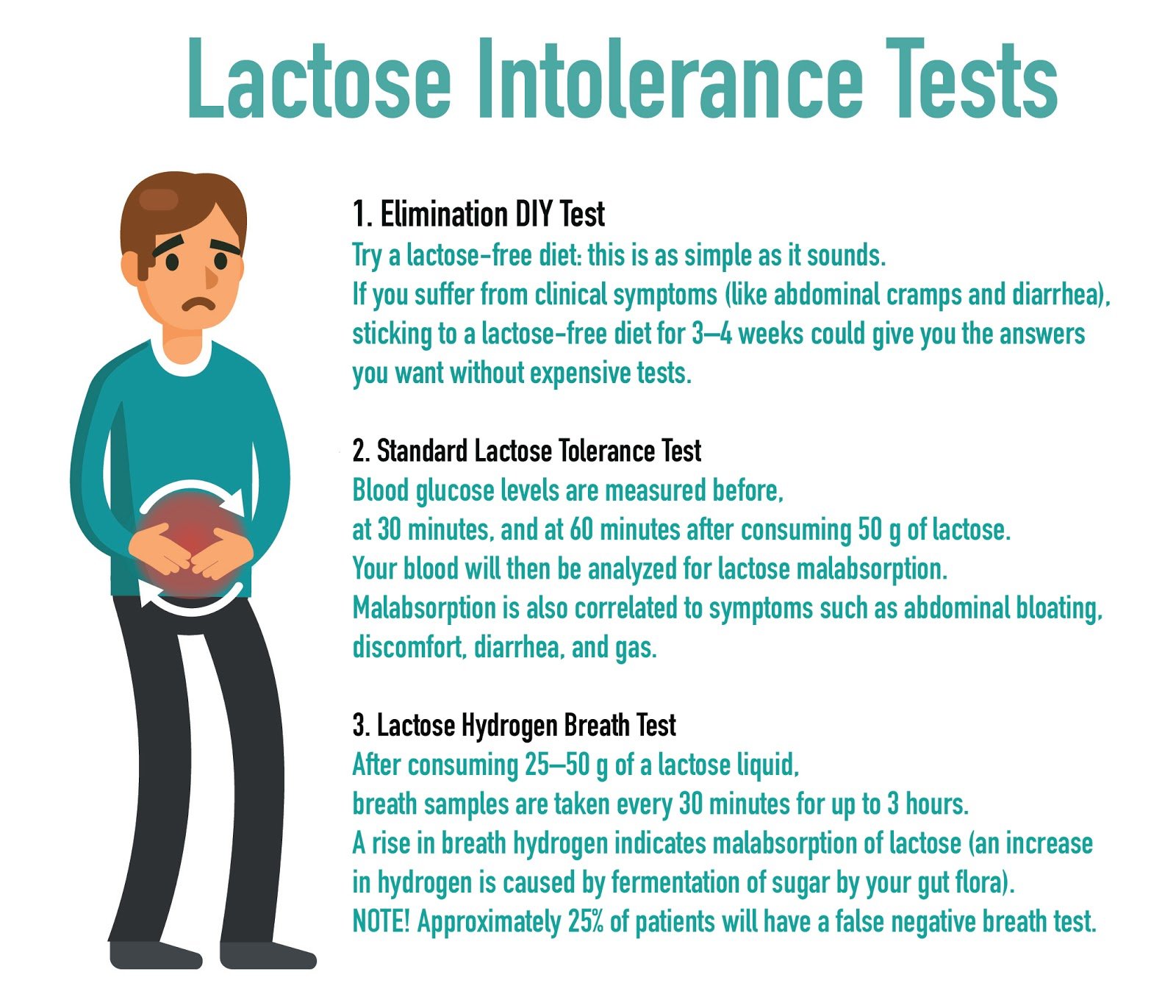
- Diagnostic Tests: While not explicitly outlined in the DSM-5, diagnostic tests such as lactose tolerance tests or hydrogen breath tests may be performed to confirm lactose intolerance. These tests measure the body’s ability to digest lactose by assessing blood glucose levels or hydrogen levels in breath samples after lactose ingestion.
- Elimination Diet: In some cases, healthcare providers may recommend an elimination diet to assess the impact of lactose-containing foods on symptoms. Patients may temporarily eliminate lactose from their diet and gradually reintroduce lactose-containing foods while monitoring symptom response.
- Differential Diagnosis: Healthcare providers also consider other gastrointestinal disorders with similar symptoms, such as irritable bowel syndrome (IBS), celiac disease, inflammatory bowel disease (IBD), and gastroenteritis, during the diagnostic process to rule out alternative diagnoses.
While lactose intolerance is not specifically listed in the DSM-5, healthcare providers utilize clinical evaluation, symptom presentation, dietary history, diagnostic tests, and differential diagnosis to assess and diagnose lactose intolerance in individuals presenting with characteristic gastrointestinal symptoms following lactose ingestion. Early diagnosis and management are essential for improving patient outcomes and alleviating symptoms associated with lactose intolerance. (Nursing Exam Help Example on Lactose Intolerance: Understanding and Management)
Treatment Regimens
Management strategies for lactose intolerance focus on reducing or avoiding lactose-containing foods and beverages while ensuring adequate nutrient intake and symptom relief. The following treatment regimens are commonly recommended:
- Dietary Modifications: Patients with lactose intolerance are advised to limit or avoid foods and beverages high in lactose, such as milk, cheese, yogurt, ice cream, and certain processed foods containing lactose as an additive. Instead, they can opt for lactose-free or lactose-reduced dairy products, including lactose-free milk, lactose-free cheese, and lactose-free yogurt. Additionally, individuals can choose lactose-free alternatives such as soy milk, almond milk, or lactose-free protein powders.
- Lactase Enzyme Supplements: Over-the-counter lactase enzyme supplements are available in various forms, including tablets, capsules, and drops, and can be taken before consuming lactose-containing foods or beverages. These supplements help break down lactose in the digestive tract, reducing the risk of gastrointestinal symptoms.
- Probiotics: Some studies suggest that probiotics containing lactase-producing bacteria may help improve lactose digestion and reduce symptoms of lactose intolerance. Probiotic supplements or foods containing live cultures, such as yogurt with active cultures, may be beneficial for certain individuals.
- Gradual Introduction of Lactose: Some individuals with lactose intolerance may tolerate small amounts of lactose-containing foods when consumed with other foods or in divided doses throughout the day. Gradually reintroducing lactose-containing foods while monitoring symptoms can help determine individual tolerance levels.
- Nutritional Counseling: Patients with lactose intolerance may benefit from nutritional counseling to ensure they maintain a well-balanced diet that meets their nutrient needs. Healthcare providers or registered dietitians can guide alternative sources of calcium, vitamin D, and other nutrients typically obtained from dairy products. (Nursing Exam Help Example on Lactose Intolerance: Understanding and Management)
Patient Education
Patient education plays a crucial role in managing lactose intolerance effectively. Key aspects of patient education include:
- Understanding Lactose Intolerance: Educating patients about the underlying cause of lactose intolerance, including deficient lactase enzyme activity in the small intestine, helps individuals understand why they experience symptoms after consuming lactose-containing foods.
- Identifying Lactose-Containing Foods: Providing patients with information about common sources of lactose in the diet, such as dairy products, and educating them on how to read food labels to identify lactose-containing ingredients helps patients make informed dietary choices.
- Dietary Modifications: Offering practical tips and recommendations for modifying the diet to reduce lactose intake, such as choosing lactose-free alternatives, incorporating calcium-rich non-dairy foods, and planning balanced meals, empowers patients to manage their symptoms effectively.
- Medication Management: Educating patients about the use of lactase enzyme supplements, including when and how to take them, helps individuals understand how these medications can alleviate symptoms and improve their quality of life.
- Monitoring Symptoms: Encouraging patients to keep a food diary to track their dietary intake and symptom occurrence helps identify specific trigger foods and monitor symptom improvement with dietary modifications or treatment regimens.
By providing comprehensive education and support, healthcare providers empower patients with lactose intolerance to make informed dietary choices, effectively manage their symptoms, and improve their overall quality of life. (Nursing Exam Help Example on Lactose Intolerance: Understanding and Management)



