Nursing Paper Example on Abscess: Understanding, Management, and Patient Education
Nursing Paper Example on Abscess: Understanding, Management, and Patient Education
Causes
Signs and Symptoms
Abscesses present with a constellation of signs and symptoms that vary depending on the location and size of the abscess, as well as the individual’s overall health status.
The most common symptom of an abscess is localized pain, often described as throbbing or sharp, which may intensify with pressure or movement. This pain is typically accompanied by swelling in the affected area due to the accumulation of pus and inflammatory fluid. The skin overlying the abscess may appear red, warm to the touch, and may exhibit increased sensitivity.
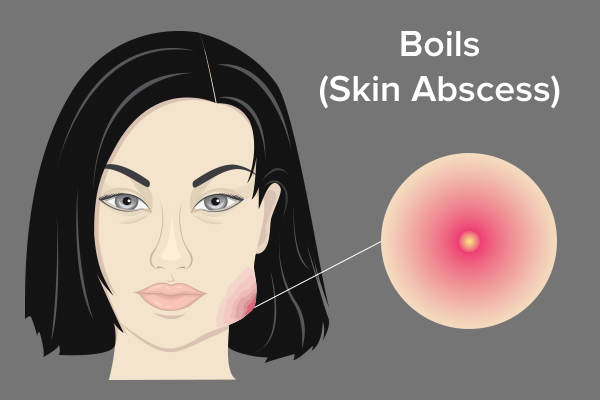
As the abscess matures, it may form a visible or palpable lump, often described as a “boil” or “pustule,” filled with pus. In some cases, the abscess may spontaneously rupture, leading to the drainage of purulent material. However, this drainage does not necessarily indicate resolution, as the abscess cavity may still require proper drainage and treatment.
Systemic symptoms such as fever, chills, and malaise may accompany abscess formation, particularly in cases of larger or deeper abscesses or those associated with more severe infections. These symptoms reflect the body’s systemic inflammatory response to the presence of infection and can serve as indicators of the abscess’s severity and potential complications.
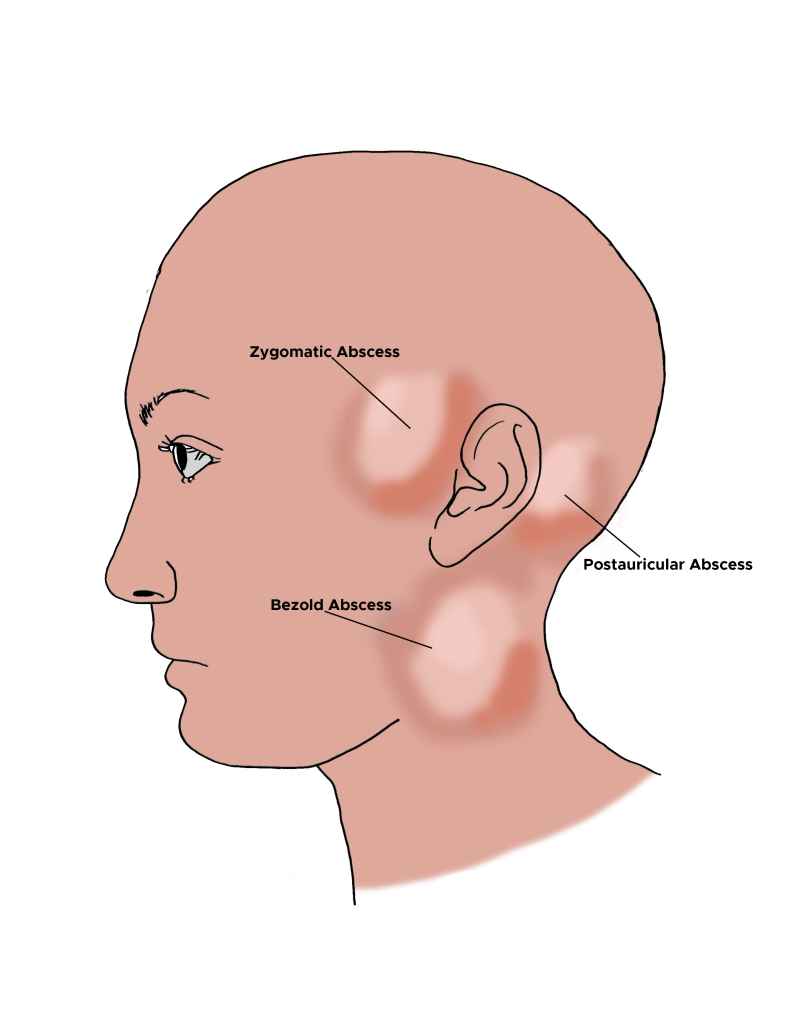
Depending on the location of the abscess, additional symptoms may arise. For example, an abscess in the oral cavity may cause difficulty chewing or swallowing, while a perianal abscess can lead to pain during bowel movements.
Overall, recognizing the signs and symptoms of an abscess is crucial for prompt diagnosis and initiation of appropriate treatment. Early intervention can help prevent complications and promote optimal outcomes for individuals affected by this common medical condition. (Nursing Paper Example on Abscess: Understanding, Management, and Patient Education)
Etiology
The etiology of abscess formation is multifaceted, involving a complex interplay of microbial pathogens, host factors, and environmental influences.
Bacterial infections, particularly by organisms such as Staphylococcus aureus and Streptococcus species, are primary drivers of abscess development. These bacteria can gain entry into the body through breaks in the skin or mucous membranes, leading to localized inflammation and the formation of pus.
Host factors play a significant role in determining susceptibility to abscess formation. Individuals with compromised immune systems, either due to underlying medical conditions like diabetes or HIV/AIDS, or as a result of immunosuppressive medications, are at increased risk. Immunodeficiency impairs the body’s ability to mount an effective immune response against invading pathogens, allowing bacteria to proliferate unchecked and form abscesses.
Chronic skin conditions, such as acne or hidradenitis suppurativa, predispose individuals to recurrent abscesses in affected areas. These conditions disrupt the normal structure and function of the skin, creating an environment conducive to bacterial colonization and inflammation.
Trauma and foreign bodies can also contribute to abscess formation. Injuries that breach the skin barrier provide a portal of entry for bacteria, while foreign materials like splinters or surgical implants can serve as niduses for infection and pus accumulation.
Environmental factors, including poor hygiene practices and overcrowded living conditions, can facilitate the transmission of infectious agents and increase the likelihood of abscess development.
Understanding the diverse etiological factors contributing to abscess formation is essential for implementing effective preventive measures and guiding targeted interventions. By addressing underlying risk factors and promoting proper wound care and hygiene practices, healthcare providers can help reduce the incidence of abscesses and improve outcomes for affected individuals. (Nursing Paper Example on Abscess: Understanding, Management, and Patient Education)
Pathophysiology
The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5), does not include abscess as a specific diagnostic category. However, abscesses may be relevant in the context of associated conditions or complications.
For instance, in cases where abscesses occur as a result of injection drug use, the DSM-5 may be used to diagnose Substance Use Disorder (SUD). Individuals with SUD may exhibit recurrent abscesses at injection sites as a consequence of their substance use behavior.
Furthermore, if abscesses occur in the context of a psychiatric disorder, such as dermatillomania or excoriation disorder, the DSM-5 may be used to diagnose the underlying mental health condition. These disorders involve compulsive skin-picking behaviors that can lead to the formation of abscesses due to skin trauma and secondary bacterial infections.
Additionally, abscesses may be considered in the differential diagnosis of certain psychiatric conditions associated with poor self-care or hygiene, such as schizophrenia or severe depression. In such cases, abscesses may serve as physical manifestations of underlying mental health issues and may prompt further evaluation and treatment by mental health professionals.
While abscesses themselves are not diagnosable using the DSM-5, their presence and associated factors may be relevant in the context of diagnosing and treating co-occurring mental health or substance use disorders. Collaborative care involving medical and mental health professionals may be necessary to address both the physical and psychological aspects of abscesses and their underlying causes. (Nursing Paper Example on Abscess: Understanding, Management, and Patient Education)
Treatment Regimens and Patient Education
Effective management of abscesses involves a combination of drainage procedures, antibiotic therapy, and patient education to promote optimal healing and prevent recurrence.
- Drainage Procedures: The primary goal of treatment is to facilitate drainage of the abscess, allowing for evacuation of pus and resolution of infection. This may be achieved through incision and drainage (I&D) performed in a medical setting under sterile conditions. During I&D, the healthcare provider makes a small incision in the abscess, allowing pus to drain freely. In some cases, needle aspiration may be used to withdraw fluid from the abscess cavity using a syringe and needle.
- Antibiotic Therapy: In addition to drainage, antibiotic therapy may be prescribed to eradicate bacterial infection and prevent recurrence. The choice of antibiotic depends on the suspected or confirmed causative organism, as well as local antimicrobial resistance patterns. Commonly used antibiotics for abscesses include oral agents such as dicloxacillin, cephalexin, or clindamycin. In cases of severe or complicated abscesses, intravenous antibiotics may be required.
- Pain Management: Pain associated with abscesses can be managed with over-the-counter analgesics such as acetaminophen or nonsteroidal anti-inflammatory drugs (NSAIDs). In some cases, prescription pain medication may be necessary to alleviate discomfort, particularly after drainage procedures.
- Patient Education: Patient education plays a crucial role in the management of abscesses to promote healing, prevent complications, and reduce the risk of recurrence. Key aspects of patient education include:
- Proper wound care: Patients should be instructed on how to clean the affected area with mild soap and water, and to apply clean dressings as directed by their healthcare provider.
- Antibiotic adherence: Patients should be educated on the importance of completing the full course of prescribed antibiotics, even if symptoms improve before the medication is finished.
- Recognition of warning signs: Patients should be informed about signs of worsening infection, such as increased pain, swelling, redness, or drainage from the abscess site, and instructed to seek medical attention promptly if these occur.
- Prevention strategies: Patients should be counseled on strategies to reduce the risk of abscess recurrence, including maintaining good hygiene, avoiding skin trauma, and seeking medical attention for any cuts or wounds that become infected.
By empowering patients with knowledge and guidance on proper wound care and preventive measures, healthcare providers can support successful outcomes in the management of abscesses while promoting overall health and well-being. (Nursing Paper Example on Abscess: Understanding, Management, and Patient Education)